Subcutaneous Dissociative Conscious Sedation a new approach to Endobronchial Intubation: Awake Endobronchial Intubation
Mihan J Javid1*, Shaabani S2
1 Department of Anesthesiology, Imam Khomeini Medical Center, Tehran University of Medical Sciences (TUMS), Tehran, IR Iran.
2 Resident in train, Tehran university of Medical Sciences, Iran.
*Corresponding Author
Mihan J Javid MD
Department of Anesthesiology,
Imam Khomeini Hospital,
Keshavarz Blvd, Tehran, IR Iran.
Tel: +98-9121216524
Fax: +98-2166581537
E-mail: mihanjavid@yahoo.com
Article Type : Research Article
Received: April 24, 2015; Accepted: September 14, 2015; Published: September 18, 2015
Citation: Mihan J Javid, Shaabani S (2015) Subcutaneous Dissociative Conscious Sedation a new Approach to Endobronchial Intubation: Awake Endobronchial Intubation. Int J Anesth Res. 3(8), 154-157. doi: dx.doi.org/10.19070/2332-2780-1500038
Copyright: Mihan J Javid© 2015. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: Lung isolation and one lung ventilation are inseparable components of thoracic surgery and thoracic anesthesia to provide patent airway and adequate surgical exposure. Endobronchial intubation is usually done under general anesthesia. The aim of this study is the evaluation of the feasibility of awake Double Lumen endobronchial intubation.
Subcutaneous Dissociative conscious sedation (as a recently introduced method) is defined as using subcutaneous injection of ketamine in conjunction with intravenous narcotics and topical oropharyngeal anesthesia to achieve an acceptable level of sedation, amnesia and pain relief for airway manipulation. This clinical trial was planned in order to evaluate subcutaneous Dissociative Conscious Sedation versus general anesthesia for endobronchial intubation.
Methods and Materials: This randomized clinical trial was conducted on 100 patients. In group A, patients were administered ketamine subcutaneously and morphine sulfate as premedication and general anesthesia was induced by administration of Na-thiopental and atracurium. In group B patients underwent DCS and were on spontaneous ventilation and received supplemental oxygen by simple mask before intubation. Hemodynamic variables were recorded. Side effects were recorded as well.
Results: In comparison to general anesthesia there was no significant hemodynamic instability, and no statistically significant increase in the incidence of nausea and vomiting was detected in this method. Despite cooperation during laryngoscopy and endobronchial intubation all the patients were amnestic.
Conclusion: Dissociative conscious sedation is an acceptable alternative to general anesthesia for endobronchial intubation.
2.Introduction
3.Materials and Methods
3.1 Statistical Analysis
4.Results
5.Discussion
6.Limitation of the study
7.Conclusion
8.Acknowledgement
9.References
Keywords
DLT; Endobronchial Intubation; Subcutaneous Dissociative Conscious Sedation; Subcutaneous Ketamine.
Introduction
Lung isolation and one lung ventilation are inseparable components of thoracic surgery and thoracic anesthesia [1-3]. General anesthesia using muscle relaxants is commonly used in order to facilitate endobronchial double lumen tube insertion [2, 3].
Patients with thoracic lesions are sometimes involved with compromised airway. Mediastinal masses and lung tumors with pressure effect on the airway are among these problems and using muscle relaxants may be accompanied by airway obstruction. Preservation of muscular tone is of paramount importance to provide airway patency and patient safety [10-12]. General anesthesia and using muscle relaxants could be life-threatening in mediastinal masses [13, 14].
Dissociative Conscious Sedation has been reported as a safe method of anesthesia with the capability to preserve spontaneous ventilation and muscle tone [15-19].
We compared sDCS and GA for double lumen endobronchial tube insertion in patients who needed thoracic surgery and one lung ventilation.
Dissociative conscious sedation is defined as using intravenous/subcutaneous injection of low dose ketamine in conjunction with intravenous narcotics to achieve an acceptable level of sedation, amnesia and pain relief [19, 20].
Material and Methods
This randomized control trial conducted on 100 patients, ASA class I and II, age 18-65, scheduled for elective thoracotomy which needed lung isolation. The study was approved by ethics committee of Tehran University of Medical Sciences. An informed written consent was obtained from the patients. Patients with predicted difficult airway or compromised airway were excluded from the study.
Exclusion criteria included predicted difficult airway or compromised airway, history of coronary artery disease, psychological disorders, increased ICP and history of drug abuse.
Noninvasive blood pressure, oxygen saturation, ETCo2, heart rate and 5 leads ECG were established before anesthesia. Vital signs were recorded 5 minutes before and 5 minutes after anesthetic administration and after endobronchial intubation.
Direct laryngoscopies performed by the same anesthesiologist for all patients by a Macintosh Laryngoscope and appropriate size of left or right sided double lumen tube (DLT) was inserted and appropriate localization of DLT was checked by fiberoptic bronchoscope. This trial was not blinded because there were obvious differences in the anesthesia method in two groups. Arterial oxygen saturation, heart rate and blood pressure were recorded before and immediately after laryngoscopy and on the second and fifth minutes after endobronchial intubation.
Patients were randomly assigned into two groups of 50 patients; A (general anesthesia) and B [subcutaneous dissociative conscious sedation (sDCS)].
In group A, patients were administered 0.5 mg/kg ketamine subcutaneously and 0.1 mg/kg morphine sulfate as premedication. Anesthesia was induced by administration of 5 mg/kg Na-thiopental and 0.6 mg/kg atracurium.
In group B patients underwent dissociative conscious sedation by administration of 0.5 mg/kg ketamine subcutaneously, 0.15 mg/ kg morphine sulfate and 1-2μ/kg fentanyl. Also tongue and pharynx were anesthetized topically by 1-2 ml lidocaine spray (4%). Spontaneous ventilation was supplemented by oxygen through face mask. Patients were asked to breath if any event of respiratory depression occurred. Unique advantage of this method of induction is that the patient is cooperative and obeys verbal commands during the procedure, but he has no recall about the events later. About 10 minutes after subcutaneous injection of ketamine on desirable level of unconsciousness-when the eyes were closed (in the absence of verbal or physical stimulation)- the patients were asked to open their mouth, then laryngoscopy and endobronchial intubation were performed. If the patient was not cooperative enough for first try intubation, additional dose of 50-100 μg fentanyl was administered to achieve optimal depth of anesthesia. The desirable level of conscious sedation is defined as “an arousable patient with proper response to verbal commands”.
The site of subcutaneous injection in both groups was infront of forearm. Increased systolic blood pressure more than 20% and/or exceeded 170 mmHg was controlled by incremental dose of TNG 50 ug IV until the systolic blood pressure reached 140 mmHg.
Patients were evaluated for the feasibility and facility of laryngoscopy and endobronchial intubation, hemodynamic changes, desaturation (SpO2<90%), nausea and vomiting, hallucination, nystagmus and salivation (need for aspiration before laryngoscopy).
In group B adverse events including irreversible apnea, desaturation (SpO2 < 90%), need for positive pressure mask ventilation, extra additional doses of fentanyl, intubation failure, visual disturbance and hallucination were recorded.
The facility of laryngoscopy was evaluated through asking the operator about satisfaction during laryngoscopy and intubation.
The incidence of nausea and vomiting in post-operative cares unit was recorded in both groups.
The day after the surgery when the patients in group B were fully awake and in stable condition they were asked about memorizing the events during laryngoscopy and intubation (recall).
Statistical Analysis
The sample size was estimated using α = 0.05 and power = 0.80. Data analysis was performed using SPSS Version 16. P value less than 0.05 was considered significant. T test and chi square test were used for quantitative and qualitative data analysis respectively.
Results
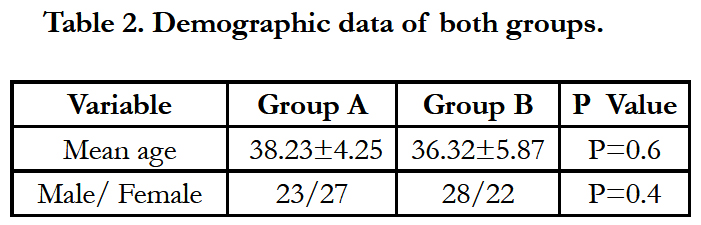
The mean age of the patients was 38.23 ± 5.25 in group A and 36.32 ± 4.17 in group B. All the patients were intubated successfully on the first attempt in both groups.
There were no event of irreversible respiratory depression, desaturation, hallucination and visual disturbance in group B. All the patients were cooperative and obedient during the laryngoscopy in this group. Mild nystagmus was detected in 3 patients in group B. Reversible apnea was detected in 4 patients in group B which was reversed by asking the patients to breathe. One patient needed additional dose of 50μg fentanyl in group B before first try laryngoscopy. Increased heart rate more than 20% from the base line was recorded during the intubation in 2 patients in group A and 2 patients in group B. Increased blood pressure more than 20% from the base line was recorded during the intubation in one patient in group A and no patient in group B. The incidence of nausea and vomiting were comparable in two groups.
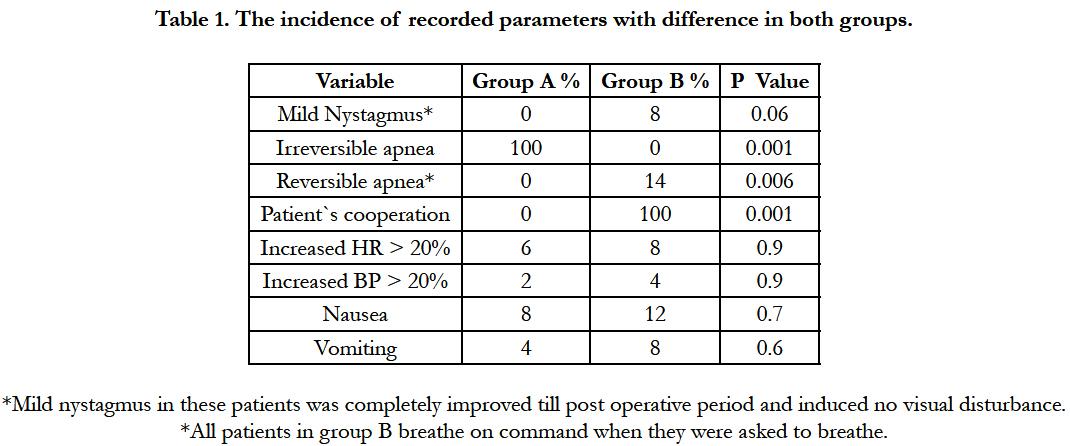
There was no report of recall about the events of laryngoscopy and intubation in two groups. It was mentioned by the operator that muscle relaxation facilitated the procedure in group A. (Table 1,2)
*Mild nystagmus in these patients was completely improved till post operative period and induced no visual disturbance.
*All patients in group B breathe on command when they were asked to breathe.
Discussion
Lung isolation and one lung ventilation are inseparable components of thoracic surgery and thoracic anesthesia [1-3]. General anesthesia using muscle relaxants is commonly used in order to facilitate endobronchial double lumen tube insertion [2, 3].
Laryngoscopy and intubation are painful procedures and in an awake patient and in the presence of inadequate anesthesia it will result in sympathetic over activity which would cause marked increase in heart rate and blood pressure [1-3]. There are many different technique of anesthesia recommended to provide optimal situation for laryngoscopy and tracheal intubation [2, 3]. Induction of anesthesia with intravenous anesthetics and neuromuscular blocking agents is one of the popular methods for this purpose [2, 3]. On the other hand some of the thoracic surgeries such as mediastinal masses are accompanied by a compromised airway due to the pressure effect of these pathologies on the airway especially after loss of airway muscle tone resulted from induction of general anesthesia [4-9]. Death after induction of anesthesia in patients with these pathologies has been reported, as a result of loss of bronchial smooth muscle tone [10-12]. So general anesthesia could be life-threatening in mediastinal tumors [13] and it is so important to maintain spontaneous ventilation and avoid positive pressure ventilation in these settings [10-12]. Administering muscle relaxant agents to these patients reduces transpleural pressure gradient, as a result of which the caliber of the airway would decrease and consequently enhance extrinsic compression [14].
In an wake process of laryngoscopy and intubation the patient would be cooperative with the anesthesiologist, while preserving spontaneous ventilation which would guarantee the patient`s safety [10-12]. Subcutaneous dissociative conscious sedation is a new method of sedation first published by Javid et al on 2011 for laparoscopic implantation of peritoneal dialysis catheter as an alternative for general anesthesia in patients involved with end stage renal disease [15]. Then the method was introduced as a safe alternative to airway regional blocks in patients with predicted difficult airway [16, 17]. This method also was introduced to be as effective as conventional methods of sedation in remote anesthesia [18]. Recently the method has been presented as effective as general anesthesia for laryngoscopy and endotracheal intubation [19]. Dissociative conscious sedation is defined as using subcutaneous injection of low dose ketamine in conjunction with intravenousnarcotics to achieve an acceptable level of sedation, amnesia and pain relief [15-20]. The known bronchodilator effect of ketamine [20] and preserving the muscular tone of the upper airway [21] are unique characteristics of this agent. Increasing the ventilator drive due to the direct effect of ketamine on the medullary respiratory neurons and the proven role of hypercarbia in increasing this effect of ketamine on ventilation are the other desirable effects of ketamine in airway management [20, 21]. In the subcutaneous route of ketamine administration, adverse effects of the drug are attenuated while desirable effects such as spontaneous ventilation, the tone of the upper airway and patient cooperationare preserved [15-19]. The gradual absorption of ketamine while using subcutaneously results in lower serum concentration and attenuates the adverse effects [17]. An important advantage of this method is preserving patient`s cooperation with the operator [15-19]. This clinical trial was conducted to find out whether this new method of anesthesia would provide an optimal situation for DLT insertion – endobronchial intubation – as effective as general anesthesia. According to our results there were no event of irreversible respiratory depression, desaturation, hallucination and visual disturbance by employing this method. All the patients were cooperative and obedient during the laryngoscopy in this group. Mild nystagmus was detected in 3 patients which was not statistically significant. All the patients had spontaneous ventilation and reversible apnea was detected in 4 patients in group B due to narcotic administration which was reversed by asking the patients to breathe. In comparison to general anesthesia there was no significant hemodynamic instability, and no statistically significant increase in the incidence of nausea and vomiting was detected in this method. Despite cooperation during laryngoscopy and endobronchial intubation all the patients were amnestic about all the events of laryngoscopy and endobronchial intubation. These results were similar to the obtained results in our previous study of comparing dissociative conscious sedation with general anesthesia for endotracheal intubation [19]. As a result of this control trial the sDCS method can be an acceptable alternative to general anesthesia for laryngoscopy and endobronchial intubation. The advantage of general anesthesia is in using neuromuscular blocking agent which facilitates intubation for the operator. The superiority of sDCS method is maintaining spontaneous ventilation in a calm and obedient patient which would be optimal choice in predicted compromised airway.
Limitation of the study
Although this method has been used successfully several times in patients with compromised airway by the author prior to the study, we excluded patients with predicted compromised airway to avoid catastrophic outcome of administering neuromuscular blocking agent in control group.
Conclusion
Dissociative conscious sedation is a safe alternative method to general anesthesia for endobronchial intubation.
Acknowledgement
The study was supported by Research Center of School of Medicine, Tehran University of Medical sciences. Mihan J Javid and Sanaz Shabani developed the original idea and the protocol, wrote the manuscript.
References
- Hillman DR, Platt PR, Eastwood PR (2003) The upper airway during anaesthesia. Br J Anaesth 91(1): 31-39.
- Donati F (2003) Tracheal intubation: Unconsciousness, analgesia and muscle relaxation. Can J Anaesth 50(2): 99-103.
- Caplan RA, Benumof JL, Berry FA, Blitt CD, Bode RH, et al. (2003) Practice guidelines for management of the difficult airway. Anesthesiology 98:1269-1277.
- Prakash UB, Abel MD, Hubmayr RD (1988) Mediastinal Mass and Tracheal Obstruction during general anesthesia. Mayo Clinic Proc 63(10): 1004-1011.
- Azizkhan RG, Dudgeon DL, Buck JR, Colombani PM, Yaster M, et al. (1985) Life-threatening Airway Obstruction as a Complication to the Management of Mediastinal Masses in Children. J Pediatr Surg 20(6): 816-822.
- Northrip DR, Bohman BK, Tsueda K (1986) Total Airway Occlusion and Superior Vena Cava Syndrome in a Child with Anterior Mediastinal Tumour. Anesth Analg 65(10): 1079-1082.
- Bitter D (1975) Respiratory Obstruction Associated with Induction of General Anesthesia in a Patient with Mediastinal Hodgkin’s Disease. Anesth Analg 54(3): 399-403.
- Levin H, Bursztein S, Heifetz M (1985) Cardiac Arrest in a Child with an Anterior Mediastinal Mass. Anesth Analg 64(11): 1129-1130.
- Béchard P, Létourneau L, Lacasse Y, Côté D, Bussières JS (2004) Perioperative Cardiorespiratory Complications in Adults with Mediastinal Mass: Incidence and Risk Factors. Anesthesiology 100(4): 826-834.
- Viswanathan S, Campbell CE, Cork RC (1995) Asymptomatic Undetected Mediastinal Mass: A Death during Ambulatory Anesthesia. J Clin Anesth 7(2): 151-155.
- Keon TP (1981) Death on induction of anesthesia for Cervical Lymph Node Biopsy. Anesthesiology 55(4): 471-472.
- Sharma RK, Swain L, Dave N (2003) Anesthetic Management of a Patient with Malignant Mediastinal Mass. Indian J Anaesth 47(3): 205- 207.
- Slinger P, Karsli C (2007) Management of the Patient with a Large Anterior Mediastinal Mass: Recurring Myths. Curr Opin Anaesthesiol 20(1): 1-3.
- Goh MH, Liu XY, Goh YS (1999) Anterior Mediastinal Masses: An Anesthetic Challenge. Anesthesia 54(7): 670-682.
- Javid MJ, Rahimi M, Keshvari A (2011) Dissociative Conscious Sedation an Alternative to General Anesthesia for Laparoscopic Peritoneal Dialysis Catheter Implantation: A Randomized Trial Comparing Intravenous and Subcutaneous Ketamine. Perit Dial Int 31(3): 308-314.
- Javid MJ (2009) Conscious Sedation with Subcutaneous Ketamine as an Alternative to Airway Regional Blocks. In 1st International Congress of Airway Management and Anesthesia in Head and Neck Surgery, Tehran. 131.
- Javid MJ (2011) Subcutaneous Dissociative Conscious Sedation (sDCS) an Alternative Method for Airway Regional blocks: A New Approach. BMC Anesthesiology 11: 19.
- Javid MJ, Karvandian K, Sha`bani S, Zebardast J (2013) Subcutaneous dissociative conscious sedation outside the operating theatre: prospective randomized double-blind study. OA Anaesthetics 1(1): 4.
- Shabani S, Javid MJ, Zebardast J (2014) Feasibility of endotracheal intubation with subcutaneous dissociative conscious sedation versus general anesthesia: a prospective randomized controlled trial. Open Journal of Anesthesiology 4(2): 41-45.
- Kim G, Green SM, Denmark TK, Krauss B (2003) Ventilatory Response during Dissociative Sedation in Children: A Pilot Study. Academic Emergency Medicine 10(2): 140-145.
- Soliman MG, Brindle GF, Kuster G (1975) Response to Hypercapnia under Ketamine Anesthesia. Can Anaesth Soc J 22(4): 486-494.