Postoperative Intractable Headache Resolving after Occipital Nerve Block
Atherton C1*, Varbanova M2, Burckhardt K3, Grigorov M4, Atherton ML5
1 Assistant Professor, Department of Anesthesiology and Perioperative Medicine, University of Louisville School of Medicine, S Jackson Street, Louisville KY, USA.
2 Associate Professor, Department of Anesthesiology and Perioperative Medicine University of Louisville School of Medicine, South Jackson Street,
Louisville KY, USA.
3 Department of Anesthesiology and Perioperative Medicine, University of Louisville KY, USA.
4 Kansas City University of Medicine and Biosciences, Kansas City, MO, USA.
5 College of Arts and Sciences University of Louisville, Louisville, KY, USA.
*Corresponding Author
Cornelia Atherton MD,
Assistant Professor, Department of Anesthesiology and Perioperative Medicine,
University of Louisville School of Medicine, 530 S Jackson Street (C2A01),
Louisville KY 40202, USA.
Tel: +1-502-852-5851 or 502-689-5442
Fax: 502-852-3762
E-mail: c0athe01@louisville.edu
Received: January 29, 2017; Accepted: February 14, 2017; Published: February 17, 2017
Citation: Atherton C, Varbanova M, Burckhardt K, Grigorov M, Atherton ML (2017) Postoperative Intractable Headache Resolving after Occipital Nerve Block. Int J Anesth Res. 5(2), 397-400. doi: http://dx.doi.org/10.19070/2332-2780-1700082
Copyright: Atherton C© 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
We present the case of a 59-year-oldman who had an unusual severe and debilitating postoperative headache and its challenging management. The patient had undergone a routine general anesthetic through his permanent tracheal stoma for this 30 minutes procedure of direct laryngoscopy and esophagoscopy with esophageal dilation. Upon arrival at recovery room, patient complained of a severe, debilitating headache not responding to aggressive pharmacologic treatment, which resolved utilizing a novel treatment. Performing an occipital nerve block in the recovery room provided rapid and complete resolution of this condition, thus avoiding further escalation of additional medication with potential unnecessary side effects and further workup and consultations. We also offer a discussion of this condition and its treatment.
Herein, we review current literature from the fields of anesthesiology, neurology and otolaryngology. This case emphasizes the impact of patient positioning regardless of duration of the procedure. It stresses on the need for awareness among anesthesia providers of the patient’s preexisting neck pathology and its possible contribution to severe postoperative headaches, resistant to pharmacologic treatment. We discuss the role of the occipital nerve block as a simple therapeutic modality for resolution of this debilitating morbidity in the postoperative period.
2.Introduction
3.Case Report
4.Discussion
5.Conclusion
6.References
Keywords
Direct Laryngoscopy Complication; Headache; Occipital Neuralgia; Occipital Nerve Block.
Introduction
Headache is the most prevalent pain disorder, affecting 66% of the global population. The most common form of headache is tension-type headache with a global prevalence of 38%. Migraine has a prevalence of 10%, chronic daily headache 3%, and cervicogenic headache (CGH) 2.5–4.1% [1]. Headache is a common postoperative complication reported by 10% to 38% of the patients during the first 24 hours after surgery, along with drowsiness, sore throat, muscle aches, vomiting (the most undesirable) and pain at surgical site. Risk factors associated with postoperative headache mentioned are: caffeine intake, alcohol consumption, history of regular headaches, age < 51yrs, female sex, and dehydration. Increased frequencies of headache and alcohol consumption were found to be independent risk factors in a prospective, observational study [2].
Research from the Mayo Clinic showed that caffeine (a cerebral vasoconstrictor) given to patients intravenously during recovery after surgery can diminish or eliminate headaches caused by rebound vasodilatation from caffeine withdrawal.
We report here in a case of a severe, debilitating postoperative headache that had a complete resolution after a simple occipital nerve block.
Case Report
A 59 year old, 95 kg man presented for direct laryngoscopy and esophagoscopy with esophageal dilation under general anesthesia as outpatient. He had a history of laryngeal cancer that was previously treated with radiation and total laryngectomy. He now complained of painless dysphagia and was scheduled for dilatation of esophageal stricture. Additional history consisted of 45 pack years of smoking, coffee intake 1 – 2 cups/day, chronic sinusitis, COPD with home O2, controlled hypertension, hyperlipidemia, non-ST elevation myocardial infarction 3 years prior (subsequent cardiac catheterization with non-obstructive coronary artery disease), chronic back pain, previous C5-C6 fusion for degenerative disk disease, and occasional shoulder pain. Home medications included atenolol, gabapentin, hydrocodone, acetaminophen, lisinopril, omeprazole, oxycodone, sertraline, and zolpidem. Current laboratory values were largely unremarkable. Physical exam showed a mildly obese gentleman that appeared his stated age and showed the expected post-operative changes after a total laryngectomy. He had a #10 stoma at the site of previous tracheostomy. His airway was a Mallampati 3 with greater than 3 finger breadths thyromental distance. Limited range of motion with extension of his neck secondary to neck fusion was noted. The remainder of the exam was benign.
After premedication with midazolam 2 mg IV he was taken to the operating room. Following preoxygenation, slow induction was performed with fentanyl 100 mcg and propofol titrated up to 200 mg; 4 cc of lidocaine 4% was sprayed down the tracheostomy and a size 7-0 endotracheal tube was placed easily through his stoma; the procedure was facilitated by rocuronium 40 mg and maintained with 2.7% sevoflurane and FiO2 60%. He underwent routine direct laryngoscopy and esophagoscopy with esophageal dilatation. A brief spike of hypertension to 180/70 was treated prompt with hydralazine 10 mg IV and labetalol 10 mg IV. Otherwise his vital signs remained at or near baseline during the 20-minute procedure. Muscular relaxation was reversed with neostigmine/glycopyrrolate and the stoma was successfully extubated upon emergence. The patient was taken to the Post Anesthesia Care Unit awake, alert, with O2 on trach mask and with vital signs at baseline.
Approximately 20 minutes after arriving to the PACU, on 40% O2 trach mask, the patient began complaining of a severe, throbbing type headache located across his bilateral occiput and radiating to the frontal region of his head. The pain was rated at 10 on a scale 0 – 10. This pain proved difficult to treat and he reported no significant relief after fentanyl (50 mcg X2), hydromorphone 0.5 mg X4), ketorolac 30 mg, intravenous administration of caffeine, acetaminophen 1g, and lorazepam. Labetalol and his home scheduled dose of lisinopril (to maintain BP at preoperative levels) werealso given. Three 20 mg boluses of propofol were followed by a 25mcg/kg/min propofol drip (20). His vital signs remained stable at baseline during his entire course. He showed no neurological symptoms or deficits, apart from the severe pain of his headache.
The severity of this headache with sudden onset and resisting to medication administered raised the suspicion of intracerebral pathology and prompted surgeons to take him emergently for a CT scan of the brain, which ruled out a subarachnoid hemorrhage. While in CT, we learned from patient’s wife that three weeks earlier he was admitted to a community hospital for the first occurrence of a headache with same characteristics and intensity as the current one. He spent several days in ICU at that time with intractable headache for which he underwent extensive workup. Unfortunately, the patient did not mention the prior ICU stay for this problem during preoperative assessment.
Medical records were obtained from the outside hospital and showed a CT and MRI of his head that were negative for any intracranial pathology. Pheochromocytoma work-up was also negative. A neurology evaluation at that time suggested the possibility of occipital neuralgia. He had not had any recurrent symptoms between that admission and the present event. Based on this history and the current presentation we decided to perform bilateral occipital nerves block as a relatively low risk intervention. In a sitting position with neck slightly flexed, 4 cc of mepivicaine 1.5% and 4cc of ropivicaine 0.5% were injected on each side along the superior nuchal ridge and in the region of the mastoid process bilaterally in the area of the greater and lesser occipital nerves for a total of 16 cc. The patient tolerated this procedure well and shortly afterwards reported near complete resolution of his head pain, confirming our diagnosis of occipital neuralgia. He was admitted and observed overnight and a neurology consultation was obtained. He did well with no recurrence of his symptoms and was discharged home the next day with the appropriate follow up.
Discussion
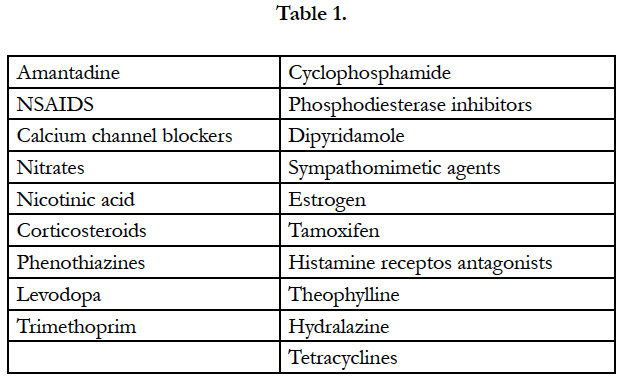
Headache is the most prevalent pain disorder, affecting 66% of the global population. The most common form of headache is tension-type headache.10% to 30% of surgical patients complain of postoperative headache during first 24 hours. Risk factors associated with postoperative headache mentioned are: caffeine intake, alcohol consumption, history of regular headaches, age < 51yrs, female sex, and dehydration. Increased frequencies of headache and alcohol consumption were found to be independent risk factors in a prospective, observational study [2]. Medications known to cause headache are included in Table 1 [3].
Research from the Mayo Clinic showed that caffeine (a cerebral vasoconstrictor) given to patients intravenously during recovery after surgery can diminish or eliminate headaches caused by rebound vasodilatation from caffeine withdrawal. In our case, caffeine failed to ameliorate the symptoms, prompting us to look for a different cause.
Other causes of headache specific to perioperative period which were ruled out are: hypoxia/hypercapnia induced cerebral vasodilatation, hypoglycemia, dehydration which causes traction on venous sinuses [4], severe arterial hypertension with cerebral edema and increased in intracranial pressure; pharmacological (hydralazine given intraoperative can cause postoperative headache through a vasodilatatory mechanism), and withdrawal of daily analgesics. Other causes include meningitis, trauma with head injury, raised ICP, and subarachnoid hemorrhage. There are two basic categories of headaches, primary and secondary. Primary headaches include those of vascular origin (cluster and migraine headaches) as well as those of muscular origin (tension-type headaches). Secondary headaches result from another source including inflammation or head and neck injuries [4].
Norwegian physician Ottar Sjaastad introduced the term, “cervicogenic headache” in 1983 by recognizing a sub-group of headache patients with concomitant head and neck pain. Cervicogenic headaches are considered “secondary headaches.”
Medical management usually begins with pharmacologic intervention; however, cervicogenic headache patients frequently do not respond to medications. Cervicogenic headache involves the posterior neck and head, it is predominantly, but not exclusively unilateral, has infrequent nausea and photophobia, the pain does not increase when bending forward, anti-migraine medications are not helpful and it is provoked by sustained, awkward neck position. Cervicogenic headache usually occurs without any demonstrable abnormality in cervical or brain imaging [3]. More invasive procedures have been suggested in the literature such as occipital nerve blocks, anesthetic and steroid blocks and treatment with pulsed radiofrequency energy [5].
In our patient, we believe that the severe cervicogenic headache was triggered mechanically, by neck extension needed for this surgical procedure, with subsequent musculofascial compression and irritation of occipital nerves. Sawin p, Todd M, Traynelis V, et al., have shown that direct visualization of the pharyngo-laryngeal structures may cause considerable motion in the cervical segments [6]. Direct laryngoscopy and rigid esophagoscopy require neck manipulation and positioning of neck extension. Direct visualization of the pharyngo-laryngeal structures is known to cause considerable motion of the cervical spine in normal patients, primarily at the occipital-C2 segments and less so at C3 to C5 [6]. Though the likelihood of spine misalignment and injury with laryngoscopy or procedures like rigid esophagoscopy seem to be low, the severe extension required for visualization of the structures combined with the muscle relaxation under general anesthesia occurs. This can be of concern in patients with preexisting spine pathology and may contribute to nerve irritation, and generated impulses from the stretched nerves may induce a headache [7, 8].
With our patient’s history of degenerative disc disease and C4/C5 fusion, organic disease at the craniocervical junction cannot be excluded. Malformation or instability of the joint space between the first and second cervical segments might cause intermittent subluxation or root compression, with referral of pain to the occiput, neck and retrobulbar area [9]. While further investigation in this patient might be contemplated, the relatively benign successful treatment with occipital nerves block may serve as sufficient diagnosis.
The rationale behind the use of peripheral nerve blocks for pain suppression is based on the ability of local anesthetics to selectively block sensory fibers at relatively low concentrations. Blockade of number of nerves in the head and neck can produce beneficial effects in pain syndromes involving regions outside the territory served by the anesthetized nerve. This is often explained by the concept of convergence in the nociceptive system of the head and neck. Not all observations can be accounted for by this mechanism. There are three phenomena associated with responses to nerve blocks described in the literature: pain relief may outlast the conduction blockade; block distal to the site of the pain inducing lesion may stop or alleviate the pain and blocking a peripheral nerve supplying a large part, but not the whole of the region of pain, may provide pain relief in the entire region [10, 11].
Conclusion
Procedures involving severe neck extensions require our awareness and discussion with the patient of the possibility of postoperative head and neck pain. Preoperative history in regard of preexisting neck problems, trauma, arthritis, previous surgery, may place the patient under increased risk for postoperative headache and should be sought. There is limited evidence from controlled studies that peripheral nerve blocks seem to be viable treatment option for selected groups of headache patients, particularly those with intractable headache or facial pain. Further studies are needed to establish the efficacy of nerve blocks in intractable headache disorders. Challenges include the difficulty in creating valid designs and controlling for headache diagnosis excluding other confounding factors that might influence clinical improvement or lack of benefit. We present the occipital nerve block as a useful treatment for intractable headache in the indicated population in the postoperative setting.
References
- Stovner L, Hagen K, Jensen R, Katsarava Z, Lipton R, et al., (2007) The global burden of headache: A documentation of headache prevalence and disability worldwide. Cephalalgia. 27(3): 193–210.
- Gill PS, Guest C, Rabey PG, Buggy DJ (2003) Perioperative headache and day case surgery. Eur J Anaesthesiol. 20(5): 401-403. doi:10.1017/S0265021503000619.
- Frese A, Evers S (2008) Biological markers of cervicogenic headache. Cephalgia. 28(1): 21-23.
- Werrett G (2002) Perioperative headache Update in Anesthesia.
- Bogduk N (2001) Cervicogenic headache: anatomic basis and pathophysiologcal mechanisms. Curr Pain Headache Rep. 5(4): 382-386.
- Sawin P, ToddM, Traynelis V, Farrell SB, Nader A, et al., (1996) Cervical spine motion with direct laryngoscopy and orotracheal intubation. An in vivo cinefluoroscopic study of subjects without cervical abnormality. Anesthesiology. 85(1): 26-36.
- Przybyla A, Skrzypiec D, Pollintine P, Dolan P, Adams MA (2007) Strength of the Cervical Spine in Compression and Bending Spine. 32(15): 1612-1620.
- Vincent M (2011) Headache and Neck. Curr Pain Headache Rep. 15(4): 324-331.
- Occipital neuralgia. http://imigraine.net/other/occipital.html
- Levin M (2010) Nerve blocks in the treatment of headaches. Neurotherapeutics. 7(2): 197-203.
- Vlassakov K, Narang S, Kissin I (2011) Local anesthetic blockade of peripheral nerves for treatment of neuralgias: systematic analysis. Anesth Analg. 112(6): 1487-1493.
- Maeley RA, Swanson J (2001) Patient Care After Discharge From the Ambulatory Surgical Center. J PeriAnesth Nurs. 16(6): 399-417.
- Fennelly M, Galletly DC, Purdie GI (1991) Is caffeine withdrawal the mechanism of postoperative headache? Anesth Analg. 72(4); 449-53.
- International Headache Society,http://ihsclassification.org
- Drezner DA (1995) Complications of direct laryngoscopy. Otolaryngol Head Neck Surg. 112(4): 630–631.
- Sjaastad O, Fredriksen TA, Pfaffenrath V (1998) Cervicogenic headache: Diagnostic criteria. The Cervicogenic Headache International Study Group. Headache. 38(6): 442–445.
- Yi X, Cook AJ, Hamill-Ruth RJ, Rowlingson JC (2005) Cervicogenic headache in patients with presumed migraine: missed diagnosis or misdiagnosis? J Pain. 6(10): 700- 703.
- Janis JE, Hatef DA, Ducic I, Reece EM, Hamawy AH, et al., (2010) The Anatomy of the greater occipital nerve: Part II. Compression point topography. Plast Reconstr Surg J. 126(5): 1563-1572.
- Krusz JC, Scott V, Belanger J (2000) Intravenous propofol: unique effectiveness in treating intractable migraine. Headache. 40(3): 224-30.