Meyerson Phenomenon: Report of Three Cases
Sergeev Y1, Mordovtseva V2, Sergeev V3
1 Chair of Skin and Veneral Diseases, I.M. Sechenov First MSMU, Moscow, Russia.
2 Chair of skin and Veneral Diseases with Cosmetology Course, IMST MGUPP, Moscow, Russia.
3 Society for Dermatoscopy and Optical Diagnosis of Skin, Moscow, Russia.
*Corresponding Author
Sergeev Yury
Chair of Skin and Veneral Diseases with Cosmetology Course, IMST MGUPP, Moscow, Russia.
E-mail: tosergeev@gmail.com
Received: July 07, 2017; Accepted : August 04, 2017; Published: August 07, 2017
Citation: Yury S, Mordovtseva V, Vasiliy S (2017) Meyerson Phenomenon: Report of Three Cases. Int J Clin Dermatol Res. 5(6), 147-150. doi: dx.doi.org/10.19070/2332-2977-1700033
Copyright: Yury S© 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Meyerson phenomenon represents an eczematous reaction around various types of melanocytic and non-melanocytic tumors. We present three cases of Meyerson phenomenon, including atypical variant, around three different melanocytic lesions.
2.Introduction
3.Case Report
3.1 Case 1
3.2 Case 2
3.3 Case 3
4.Discussion
5.References
Keywords
Meyerson Phenomenon; Meyerson Nevus; Dermoscopy; Halo Eczema; Melanoma.
Introduction
First mention of the development of an eczematous reaction around melanocytic nevi dates back to 1971. At that time such reaction was regarded as an atypical pityriasis rosea with Koebner phenomenon around the nevi [1]. Since then similar reaction, also called Meyerson’s phenomenon or halo eczema, has been described around various melanocytic (common acquired nevus, congenital nevus, dysplastic nevus, Spitz nevus, melanoma) and non-melanocytic (sebaceous nevus, seborrheic keratosis, dermatofibroma, nevus flammeus, basal cell carcinoma and squamous cell carcinoma) tumors [2]. By now, different causes of Meyerson phenomenon have been proposed, including sunburns, atopic predisposition, chemotherapy and interferon-α treatment, but the exact reason of such reaction remains unknown [3, 4].
Meyerson phenomenon typically occurs as a symmetrical erythema, vesiculation and scaling around one, some or all nevi of the patient. Lesions may be asymptomatic or pruritic and accompanied by eczema-like rash on healthy skin. More often Meyerson phenomenon occurs in males, locates on the trunk or proximal extremities [3-5]. The eczematous reaction doesn’t modify the dermoscopic structures of the lesion, but can make them look blurred [6]. Dermoscopic patterns mainly depend on type of the lesion around which Meyerson phenomenon occurs and are combined with typical features of eczema - dotted vessels, scales and yellow crusts [3]. Histopathology reveals spongiosis, vesiculation and parakeratosis in the epidermis and superficial inflammatory infiltration in the dermis, associated with lymphocytic exocytosis.
Predominance of the CD4+ lymphocytes in the infiltrate accentuates the inflammatory nature of the Meyerson phenomenon [2, 6].
The eczematous reaction can last up to 12 weeks without treatment and relapse several times. Treatment modalities include observation, topical steroids and excision of the nevus [2].
Case Report
We report our experience with three cases of Meyerson phenomenon.
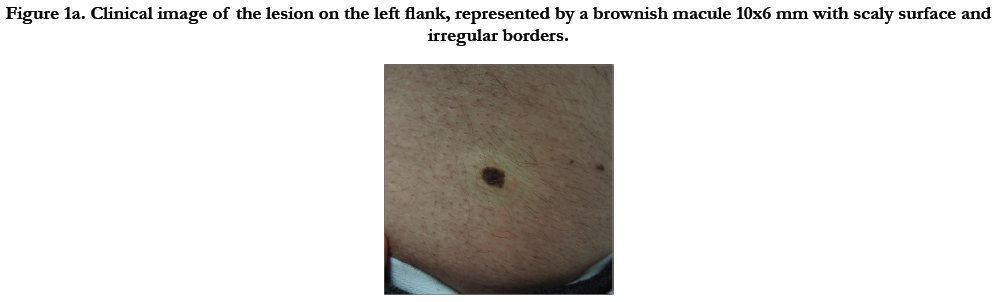
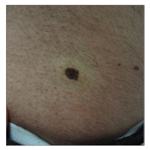
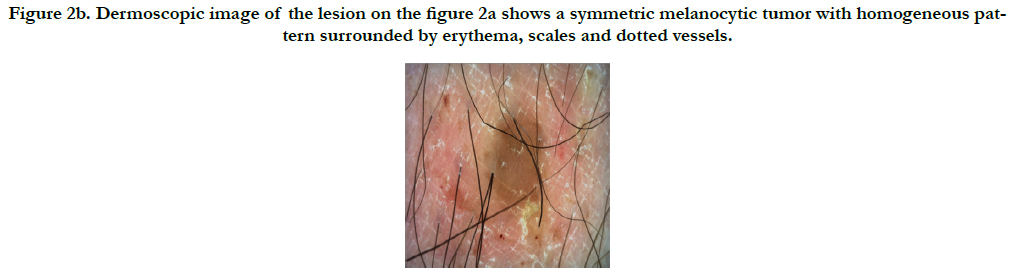
A 34-year-old male presented to our clinic with a 2-week history of pruritus around a pigmented lesion on the left flank. The patient denied any possible triggers. Physical examination revealed pronounced xerosis and multiple melanocytic nevi (congenital, common acquired and dysplastic). Lesion on the trunk was represented by a brown macule 10x6 mm with scaly surface and irregular borders (Figure. 1a). Dermoscopic examination revealed a slightly asymmetric melanocytic tumor with a blurry silhouette due to scales (Figure. 1b). Three additional dome-shaped brown papules with symmetric halo eczema were present on the upper extremities (Figure. 2a). Dermoscopic examination revealed typical melanocytic nevi with homogeneous and globular patterns, surrounded by erythema, dotted vessels, scales and yellow crusts (Figure. 2b). Topical steroid and moisturizing ointment were prescribed for 14 days with subsequent follow-up, but the patient didn’t return.
Figure 1a. Clinical image of the lesion on the left flank, represented by a brownish macule 10x6 mm with scaly surface and irregular borders.
Figure 1b. Dermoscopic image of the same lesion shows a slightly asymmetric melanocytic tumor with a blurry silhouette due to scales.
Figure 2a. Lesion on the arm of the same patient presented by brown dome-shaped papule with symmetric halo eczema.
Figure 2b. Dermoscopic image of the lesion on the figure 2a shows a symmetric melanocytic tumor with homogeneous pattern surrounded by erythema, scales and dotted vessels.
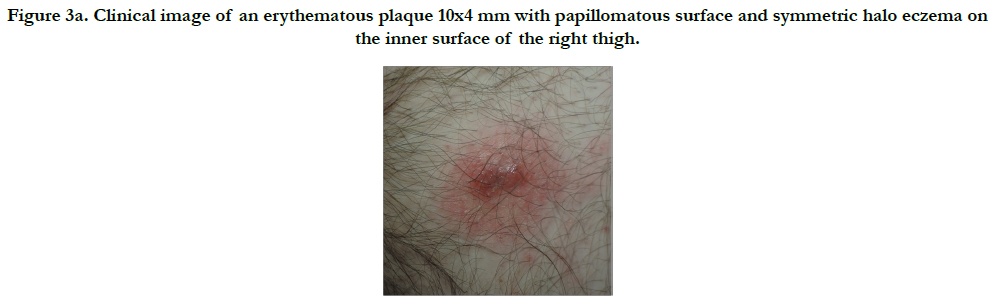
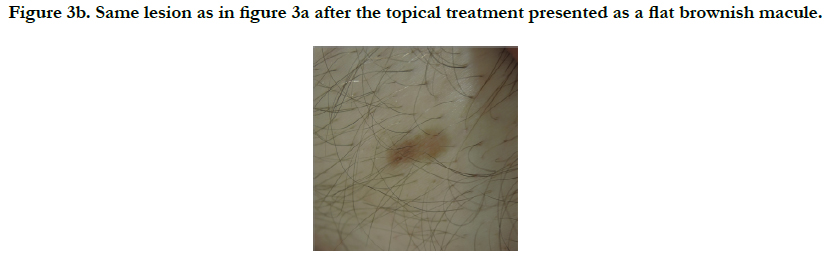
A 19-year old male presented to our clinic with a 1-week history of pruritic rash on his right leg. The patient denied any possible triggers, but had a history of atopic dermatitis and allergic rhinitis in childhood. Physical examination revealed an erythematous plaque 10x4 mm with papillomatous surface and symmetric halo eczema on the inner surface of the right thigh (Figure. 3a). Dermoscopic examination of the lesion didn’t reveal any nevus associated structures and was represented mostly by glomerular vessels on milky-red background, but the structures were blurry due to scales, crusts and edema. Additionally, focuses of eczema were found on the legs and arms. Topical steroid was prescribed for 14 days and following treatment, the lesion on the leg turned into a flat brownish macule (Figure. 3b) with homogeneous pattern upon dermoscopy. After one-year follow-up no relapses occurred and the nevus was stable.
Figure 3a. Clinical image of an erythematous plaque 10x4 mm with papillomatous surface and symmetric halo eczema on the inner surface of the right thigh.
Figure 3b. Same lesion as in figure 3a after the topical treatment presented as a flat brownish macule.
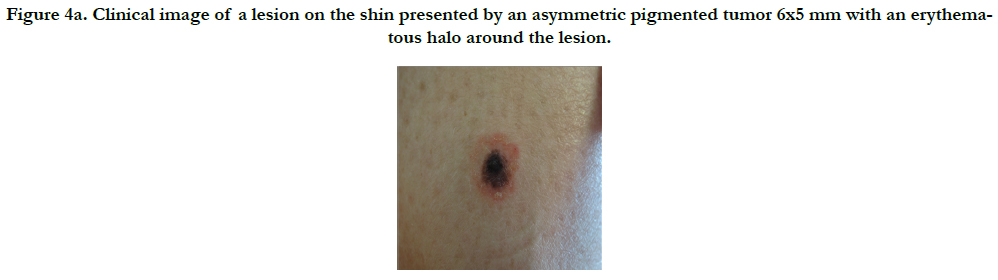
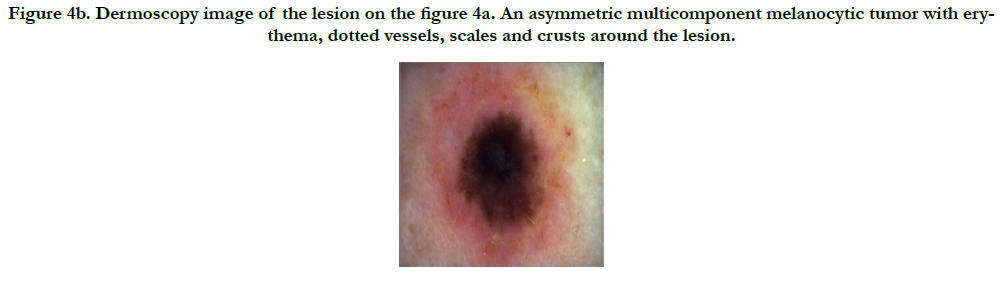
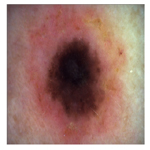
A 44-year-old woman presented to our clinic with a 2-week history of pruritus around the pigmented lesion on the shin. The patient denied any possible triggers, her medical history had nothing specific. Physical examination revealed an asymmetric pigmented lesion 6x5 mm with an erythematous halo around the lesion (Figure. 4a). Dermoscopically, pigment network, eccentric hyperpigmented area and chrysalis structures were observed, surrounded by erythema, yellow crusts and scales (Figure. 4b). Excisional biopsy confirmed the clinical diagnosis of superficial spreading melanoma, Clark level III, Breslow thickness 1.1 mm. Sentinel lymph node biopsy was negative.
Figure 4a. Clinical image of a lesion on the shin presented by an asymmetric pigmented tumor 6x5 mm with an erythematous halo around the lesion.
Figure 4b. Dermoscopy image of the lesion on the figure 4a. An asymmetric multicomponent melanocytic tumor with erythema, dotted vessels, scales and crusts around the lesion.
Discussion
These cases provide additional confirmation that Meyerson phenomenon may affect any type of melanocytic lesions. In contrast to the general assumption that the eczematous reaction doesn’t involve the melanocytic lesion itself, we report a patient with pronounced changes of the nevus, making a correct diagnosis a challenge to the physician. We strongly believe that interpretation of the dermoscopic structures of a lesion with a Meyerson phenomenon should be carried out only after topical steroid treatment, unless melanoma-specific structures are observed.
References
- Meyerson LB (1971) A peculiar papulosquamous eruption involving pigmented nevi. Arch Dermatol. 103(5): 510-512.
- Pižem J, Stojanovič L, Luzar B (2012) Melanocytic lesions with eczematous reaction (Meyerson's phenomenon) - a histopathologic analysis of 64 cases. J CutanPathol. 39(10): 901-10. doi: 10.1111/j.1600-0560.2012.01960.
- Oliveira A, Arzberger E, Massone C, Fink-Puches R, Zalaudek I, et al., (2014) Dermoscopy, reflectance confocal microscopy and immunohistochemical analysis in melanocytic lesions with Meyerson's phenomenon. Dermatology. 229(4): 297-305. doi: 10.1159/000365657.
- Rolland S, Kokta V, Marcoux D (2009) Meyerson phenomenon in children: observation in five cases of congenital melanocytic nevi. Pediatric Dermatology. 26(3): 292–297. doi:10.1111/j.1525-1470.2009.00931.
- Loh J, Kenny P (2010) Meyerson Phenomenon. J Cutan Med Surg. 14(1): 30-2. doi: 10.2310/7750.2009.08065.
- GabbiT VB, Omar ED, Criado PR, Valente NYS, Martins JEC (2010) Clinical, dermoscopic and histopathological evaluation of the Meyerson nevus – case report. An Bras Dermatol. 85(5): 681-3.