Orbital Lymphoma as Cause of Proptosis in Right Eye
Parada-Vasquez RH1*, Medina-Lopez JP1, Velasco-Calvo CM1, del Valle-Penella A1, Martins-Baia R2
1 Department of Anterior Segment, Vision Institute, Hospital La Carlota, Montemorelos, Nuevo Leon, Mexico.
2 Department of Oculoplastic, Vision Institute, Hospital La Carlota, Montemorelos, Nuevo Leon, Mexico.
*Corresponding Author
René Hernán Parada Vásquez,
Department of Anterior Segment, Vision Institute,
Hospital La Carlota, Montemorelos, Nuevo León, México.
Vision Institute. Camino al vapor 209. Col.
Zambrano, Montemorelos, Nuevo León, México.
Tel: +528262651079
E-mail: rene_hernan@hotmail.com
Received: February 06, 2017; Accepted: February 27, 2017; Published: February 28, 2017
Citation: Parada-Vasquez RH, Medina-Lopez JP, Velasco-Calvo CM, del Valle-Penella A, Martins-Baia R (2017) Orbital Lymphoma as Cause of Proptosis in Right Eye. Int J Ophthalmol Eye Res. 5(2), 277-279. doi: dx.doi.org/10.19070/2332-290X-1700059
Copyright: Parada-Vasquez RH© 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Purpose: A case of B-cell non-Hodgkin lymphoma is presented in the right orbit, which, after treatment with excisional biopsy plus chemotherapy, reached a favorable resolution after 9 months of treatment.
Case Report: 83-year-old male, who at physical exam presents with infraorbital proptosis at the right eye and a 1 cm mobile mass in the right orbit. An excisional biopsy via transconjunctival inferior orbitotomy showed a non-Hodking B cell lymphoma.
Discussion: Surgical resection plus chemotherapy gave a favorable outcome at follow-up. The fundamental pillars for a good therapeutic approach is the correct histological classification, and the timely multidisciplinary management in this type of diagnosis.
Conclusion: The correct histological classification and appropriate multidisciplinary management of these patients are the fundamental pillars of good therapeutic results.
2.Introduction
3.Clinical Case
4.Discussion
5.Conclusion
6.References
Keywords
Orbital tumors; Lymphoma; Biopsy; Chemotherapy; Mexico.
Introduction
Lymphomas of the ocular adnexa constitute approximately 8% of all extra ganglionic lymphomas [1]. They represent 8% of orbital tumors and close to 13% of primary malignant tumors of the eyelid [2]. The majority of orbital lymphomas are non-Hodgkin type, and of these, 80% originate in B cells [3]. In Latin America, those affected tend to be middle-aged to elderly people, with preference for the male sex (2:1). This high prevalence and the possibility of having an effective treatment for healing, makes this type of tumors important for study in ophthalmology. The condition may be primary, involving one or both orbits, or secondary if one or more identical foci exist in another part of the body [3, 4].
Clinical Case
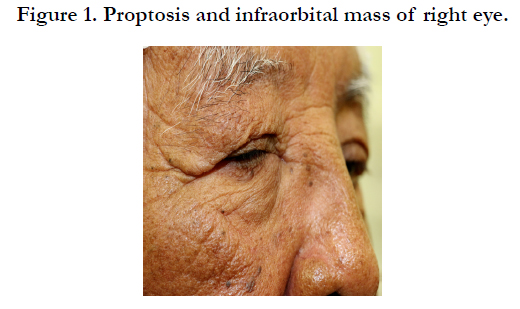
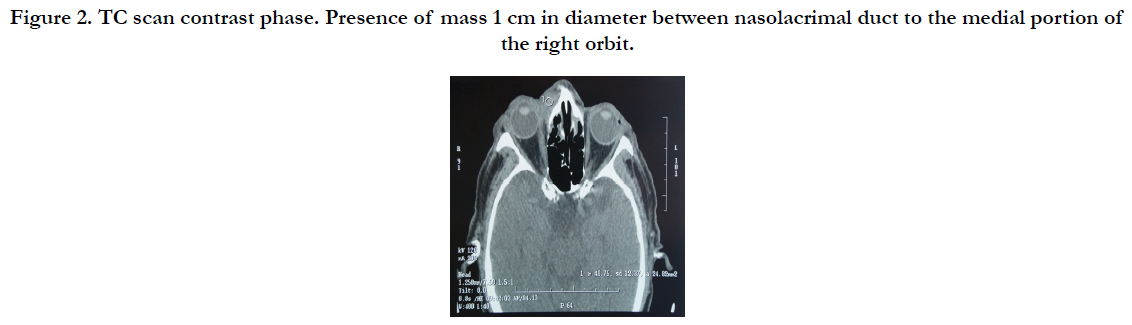
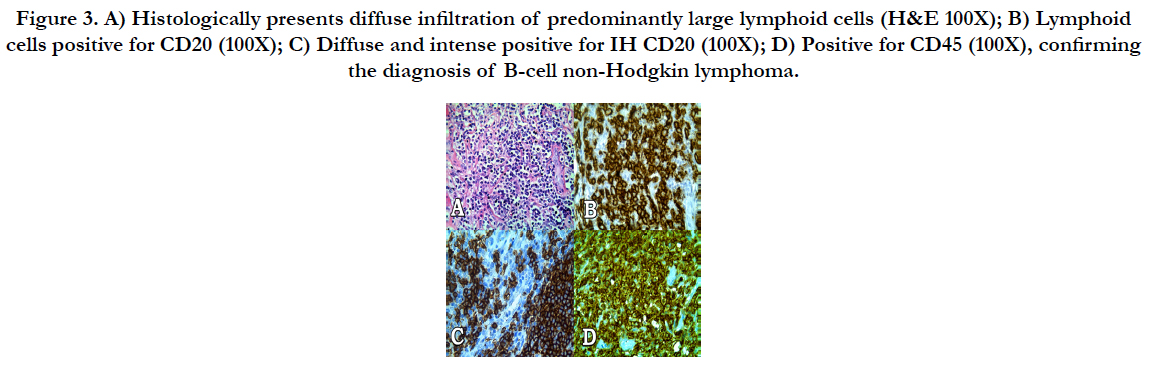
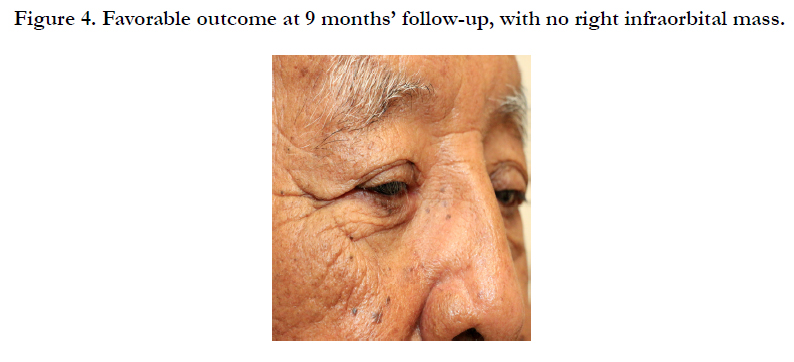
83-year-old male, with no history of medical pathologies. Consultation due to inflammation of the lower eyelid of the right eye (OD) with 6 months of evolution, denies other symptomology. Best corrected visual acuity in the right eye is 20/100, and in the left eye is 20/30. Primary position is in ortho position, with conserved ductions and versions; exophthalmometry in the right eye of 19.6 mm and in the left eye of 18.2 mm. Upon clinical examination, proptosis plus increased volume in the inferior periorbital zone is observed in the OD, with the presence of a mobile mass 1 cm in diameter, which does not crackle, with regular edges, well-delineated, with a reddish appearance to the skin of the lower eyelid (Figure 1); the rest of the anterior and posterior segment is within normal limits. Computed tomography (CT) is requested of the orbit with 1 mm cuts in single and contrast phase to evaluate the orbital mass. It revealed the presence of an occupation of the right nasolacrimal duct, extending to the medial extraconal portion of the right orbit, without affecting the extraocular muscles, only displacing the orbit towards the right side (Figure 2). We proceeded to perform excision surgery via medial orbitotomy plus a biopsy of the orbital tumor of the right eye. Tissue sample was sent to pathology in the shape of a diamond measuring 1.5 x 1 x 0.5 cm, with yellowish gray surface. Sample revealed diffuse infiltration by predominantly large lymphoid cells, with scant cytoplasm and ovaloid to round nucleus with clumps of chromatin, prominent nucleolus and scant eosinophils. Studies were performed with Hematoxylin and Eosin (H&E) and immunohistochemistry (IH) for common leukocyte antigen, CD20 and CD45 (Figure 3), resulting in diffuse and intense positives (+++), confirming the diagnosis of B-cell non-Hodgkin lymphoma. He was therefore referred to hematology, where he began chemotherapy treatment under the CHOP regimen (cyclophosphamide, doxorubicin, vincristine and prednisone) beginning with 375 mg/ m2 of rituximab at the standard dosage every 28 days. The patient showed good overall health during the treatment, as well as strict systemic control in search of foci of dissemination in: the brain, liver and lungs, without evidence of tumor activity. He presented clinical improvement from the first cycle of treatment. Followed up with ophthalmology every 3 months until reaching the current complete resolution (Figure 4).
Figure 2. TC scan contrast phase. Presence of mass 1 cm in diameter between nasolacrimal duct to the medial portion of the right orbit.
Figure 3. A) Histologically presents diffuse infiltration of predominantly large lymphoid cells (H&E 100X); B) Lymphoid cells positive for CD20 (100X); C) Diffuse and intense positive for IH CD20 (100X); D) Positive for CD45 (100X), confirming the diagnosis of B-cell non-Hodgkin lymphoma.
Discussion
A case of B-cell non-Hodgkin lymphoma is presented in the right orbit, which, after treatment with excisional biopsy plus chemotherapy, reached a favorable resolution after 9 months of treatment. Taking into account the patient’s diagnosis, nuclear magnetic resonance imaging (MRI) was performed of the thorax and abdomen, yielding results within the normal limits. These analyses were taken into account, since previous studies have shown that, as in our case, the affectation of the orbital often is not associated with systemic disease, in many cases being the only manifestation of the disease [3, 4].
Orbital lymphoma is an extremely rare form, making up 1% of all lymphomas, with primary malignant neoplasia being more common in the orbit (55%) [5-7].
The literature states that the most frequent age of appearance is beyond the fourth decade of life, which is coherent with our patient who is in his ninth decade; it rarely presents before the age of 20 and when this happens, leukemia should be suspected [6, 7]. On the other hand, the case presents a male patient despite a greater prevalence among females in Spain [8, 9]. As with this patient, various studies mention the infraorbital localization (58%) as the most frequent among orbital lymphomas [9, 10]. Regarding the clinical evolution of our case, it is worth mentioning that the presentation of orbital lymphomas occurs insidiously as a palpable tumor of the conjunctiva, eyelid or orbit, with no painful characteristics, appearing chronically, displacing the ocular globe and diminishing visual acuity [9, 10].
As for imaging studies, ultrasound can be used; however, CT with a contrast method and MRI are preferred because their greater precision allows for the evaluation of the localization and extent of the tumor [10]. In spite of this, a biopsy-excision of the lymphoma is needed for definitive diagnosis [10, 11]. Histologically, this type of lymphoma is characterized as presenting a diffuse lymphoid infiltration, situated below the epithelium, whose lymphoid infiltration is comprised of small centrocyte type cells, niduses of monocytoid cells, centroblasts and many plasmatic cells [11-15]. In immunohistochemical tests, various studies mention that all of their patients with lymphomas were reactive for the B-cell marker (CD20), as with the case described in this report [16, 17]. Differential diagnosis is made with autoimmune, infectious and inflammatory processes, such as idiopathic orbital inflammation, thyroid ophthalmopathy, or local lymphoid hyperplasia [17, 18]. It is worth noting that primary orbital lymphomas have a favorable prognosis [19, 20]. With regard to therapeutic options, they include: biopsy, radiotherapy and chemotherapy [18-20]. The surgical approach is determined by the localization, extent and type of lesion, without seeking additional morbidity [20].
Conclusion
The correct histological classification and appropriate multidisciplinary management of these patients are the fundamental pillars of good therapeutic results.
References
- Bowlin B (2016) Kanski’s Clinical Ophthalmology: A Systematic Approach. 8th (Edn), Elsevier, Philadelphia.
- Perry JD, Singh AD (2014) Clinical ophthalmic oncology - Orbital and adnexal lymphoma. 2nd (Edn), Springe-Verlag, Berlin Heidelberg.
- Galnares-Olalde JA, González LF, Cadena-Camacho JA, Muñoz-Abrahama O (2014) Linfoma orbitario: reporte de un caso y revisión de la literatura. Rev Mex Oftalmol. 88(3): 141-145.
- Hervás-Ontiveros A, España-Gregori E, Hernández-Martínez P, Vera-Sempere FJ, Díaz-Llopis M (2014) Orbital involment by Nk T-cell non-hodgkin lymphoma Orbital involvment by non-Hodgkin lymphoma NK T cells. Arch Soc Esp Oftalmol. 89(11): 450–453. DOI: 10.1016/j.oftal.2013.10.006.
- Pizarro-Barrera ME, Corredor-Casas S, Salcedo-Casillas G, Rodríguez-Reyes A (2006) Orbital lymphoma: a case report. Rev Mex Oftalmol. 80(2): 89-92.
- Soriano-Lafarga A, García-Delpech S, Verdejo-Gimeno C, Navarro-Piera J, Capmany-Ros L, et al., (2003) Orbital lymphoma as the first manifestation of non-Hodgkin's lymphoma .Arch Soc Canar Oftal. 14: 111-114.
- Volpe NJ, Gausas RE (1999) Optic nerve and orbital tumors. Neurosurg Clin N Am. 10(4): 699–715.
- Gordon LK (2006) Orbital inflammatory disease: a diagnosic and therapeutic Challenger. Eye 20(10): 1196-206. DOI: 10.1038/sj.eye.6702383
- Fernández-Hermida RV, Pinar S, Muruzábal N (2008) clinical manifestations of thyroid opthalmo. An Sist Sanit Navar. 31(3): 45-56.
- Valvassori GE, Sabnis SS, Mafee RF, Brown MS, Putterman A (1999) Imaging of orbital lymphoproliferative disorders. Radiol Clin NA. 37(1): 135–150.
- Uta Schick, Oliver Lermer, Renate Unsold, Werner Hassler (2004) Treatment of primary orbital lymphomas. Eur J Haematol. 72(3): 186-192. DOI :10.1046/j.0902-4441.2003.00192.
- White WL, Ferry JA, Harris NL, Grove AS Jr (1995) Ocular adnexal lymphoma: A clinicopathologic study with identification of lymphomas of mucosa- associated lymphoid tissue type. Ophthalmology. 102(12): 1994-2006.
- Vilar-González S, Lamas-Oliveira C, Fagúndez-Vargas MA, Núnez-Quintanilla AT, Pérez-Rozos A, et al., (2015) Thyroid Orbitopathy, a global visión with special attention to the role of radiotherapy. Endocrinol Nutr. 62(4): 188-199.
- Whitcup SM, de Smet MD, Rubin BI, Palestine AG, Martin DF, et al., (1993) Intraocular lymphoma. Clinical and histopathologic diagnosis. Ophthalmology. 100(9): 1399-1406.
- Rey-Porca C, Pérez-Encinas M, Gonzalez F (2008) Orbital lymphomas . presentation of nine cases. Arch Soc Esp Oftalmol 83(2): 95-104.
- Yeo JH, Jakobiec FA, Abbott GF, Trokel SL (1982) Combined clinical and computed tomographic diagnosis of orbital lymphoid tumors. Am J Ophthalmol. 94(2): 235-45.
- Du MQ (2007) MALT lymphoma: Recent advances in aetiology and molecular genetics. J Clin Exp Hematopatol. 47(2): 31-40.
- Haradome K, Haradome H, Usui Y, Ueda S, Kwee TC, et al., (2014) Orbital lymphoproliferative disorders (OLPDs): value of MR imaging for differentiating orbital lymphoma from benign OPLDs. AJNR Am J Neuroradiol. 35(10): 1976-82. DOI: 10.3174/ajnr.A3986.
- Lazzarino M, Morra E, Rossi R, Brusamolino E, Pagnucco G, et al., (1985) Clinicopathologic and immunologic characteristics of non-Hodgkin´s lymphomas presenting in the orbit. A report of eight cases. Cancer. 55(9): 1907-1912.
- Díaz Llopis M (1996) Aids in Opthamology. 1st (Edn), Tecnimedia, Valencia.