Radiological Assessment Of Cervical Spine Mobility Comparing Direct Laryngoscopy With Miller Blade And Video-Laryngoscopy With CMAC In Healthy Adults
Niño C1, Cohen D1, Reyes Uscátegui LI1, Bermúdez S2, Useche JN2, Morillo AJ2, Pasternak JJ3*
1 Department of Anesthesia, University Hospital Fundación Santafe de Bogotá, Calle, Bogotá, Colombia.
2 Department of Radiology, University Hospital Fundación Santafe de Bogotá, Calle, Bogotá, Colombia.
3 Department of Anesthesiology and Perioperative Medicine, Mayo Clinic College of Medicine, Rochester, MN, USA.
*Corresponding Author
Jeffrey J. Pasternak, MS, MD,
Mayo Clinic College of Medicine,
200 First Street SW. Rochester, Minnesota, USA.
Tel: (507) 255-4235
Fax: (507)255-6463
E-mail: pasternak.jeffrey@mayo.edu
Received: July 31, 2017; Accepted: August 29, 2017; Published: August 30, 2017
Citation: Niño C, Cohen D, Reyes Uscátegui LI, Bermúdez S, Useche JN, Pasternak JJ, et al. Radiological Assessment Of Cervical Spine Mobility Comparing Direct Laryngoscopy With Miller Blade And Video-Laryngoscopy With CMAC In Healthy Adults. A Case Report Study. Int J Anesth Res. 2017;5(7):473-478. doi: dx.doi.org/10.19070/2332-2780-1700096
Copyright: Pasternak JJ© 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Study Objective: Quantify cervical spine range of motion during laryngoscopy via either direct laryngoscopy with a Miller blade or via video laryngoscopy with a CMAC system.
Design: Prospective case series.
Setting: Interventional radiology suite at an academic medical center.
Patients: Five adults requiring general anesthesia with tracheal intubation to facilitate interventional radiology procedures.
Interventions: Fluoroscopic imaging of cervical spine anatomy prior to induction of general anesthesia and then during both direct laryngoscopy and video laryngoscopy.
Measurements: Quantification of angles between skull base and prespecified cervical vertebrae and between the first cervical vertebrae and lower prespecified cervical vertebrae. These groups of measurement either do or do not account for movement of the atlanto-occipital joint, respectively.
Main Results: There was a tendency toward reduced cervical extension both relative to skull base and intrinsicly within the cervical spine during laryngoscopy with the CMAC video laryngoscope as compared to direct laryngoscopy with a Miller blade.
Conclusions: We describe a novel technique to quantify cervical motion during laryngoscopy. Laryngoscopy with a CMAC video laryngoscope may reduce cervical extension as compared to direct laryngoscopy with a Miller blade. Video laryngoscopy may attenuate cervical extension during laryngoscopy, an effect that can be useful in patients with cervical spine disease or instability.
2.Introduction
3.Materials and Methods
3.1 Anesthetic Management
3.2 Laryngoscopy and Comparison of Cervical Motion
3.3 Quantification of Cervical Mobilization
4.Results
5.Discussion
6.Conclusion
7.References
Keywords
Laryngoscopy; Airway; Intubation; Video laryngoscopy, Direct Laryngoscopy; Fluoroscopy.
Introduction
The degree of mobilization of the cervical spine (CS) during orotracheal intubation maneuvers (OTI) is of great importance during airway management in patients with pathology or instability of the CS, such as in those with cervical spinal cord trauma (CT) or other chronic diseases [1]. A reduction in CS movement during OTI is beneficial for these patients because undesirable mobilization can create or worsen a neurological injury [2]. Moreover, patients with cervical instability and acute cardiovascular or airway compromise may require a rapid intubation which should be made in the fewest attempts possible while minimizing cervical mobilization (CM) as much as possible [3]. Patients with other spinal cord diseases also benefit from a reduction in CS motion during direct laryngoscopy (DL), because this decreases the possibility of nerve and vascular structure compression due to vertebral displacement.
Video-laryngoscopy (VL) has been evaluated in different clinical context showing high success rates for OTI with [4-6] or without predictors of difficult airway [7]. VL in patients with cervical pathology can match or exceed the success rate of direct laryngoscopy, using comparable times and possibly reducing extension of the CS [8]. The difference in CS mobilization angles during OTI via DL have not been compared to those encountered with the Cmac video laryngoscope (Karl Storz, Tuttlingen - Germany). The aim of the study is to compare the range of motion of the CS during OTI with the CMAC video laryngoscope using a DBlade blade against DL with a Miller blade in healthy patients using fluoroscopy.
Materials and Methods
The institutional ethics committee approved the study protocol. Five patients were included without randomization, all > 18 years of age without cervical pathology and without predictors for a difficult airway. Patients were all previously scheduled for radiologic procedures distant to the CS, requiring the use of fluoroscopy, and requiring general anesthesia and OTI. Patients signed their approval form for the inclusion in the study by signing an informed consent.
All patients were assessed in a pre-anesthetic consultation. They underwent conventional anesthesia according to hospital protocol in an interventional radiology suite. Induction of general anesthesia was conducted with a combination of propofol and remifentanil. Rocuronium was administered to facilitate laryngoscopy and OTI. Maintenance of general anesthesia consisted of sevoflurane and remifentanil with additional doses of rocuronium administered to maintain muscle relaxation. Basic monitoring was performed with electrocardiography, noninvasive blood pressure, pulse oxymetry, capnography, body temperature and a gas analyzer. Patients then underwent their radiologic procedure. Once the procedure ended, each patient was allowed to emerge from general anesthesia, the tracheal tube was removed when appropriate, and the patient was then transferred to the post anesthetic care unit.
For each patient, a baseline fluoroscopic image of the lateral CS was obtained with the neck in the neutral position prior to induction of general anesthesia. All images were obtained with a digital angiograph Philips Integris Allura Xper FD20 (Philips Medical Systems DMC GmbH, Hamburg, Germany). All laryngoscopies were conducted with the standard technique by the same trained anesthesiologist. Following induction of general anesthesia and complete muscle relaxation, a second fluoroscopic image of the lateral CS was obtained during DL with a number 2 Miller blade and a conventional laryngoscope with an occipital support in place. Finally, laryngoscopy was performed with a CMAC video laryngoscope and a D-Blade without occipital support during which a third fluoroscopic image of the lateral CS was obtained. Normal oxygenation, blood pressure, and body temperature were ensured throughout the whole process. At this time, the patient was intubed using a guide stylet and the scheduled surgical procedure commenced.
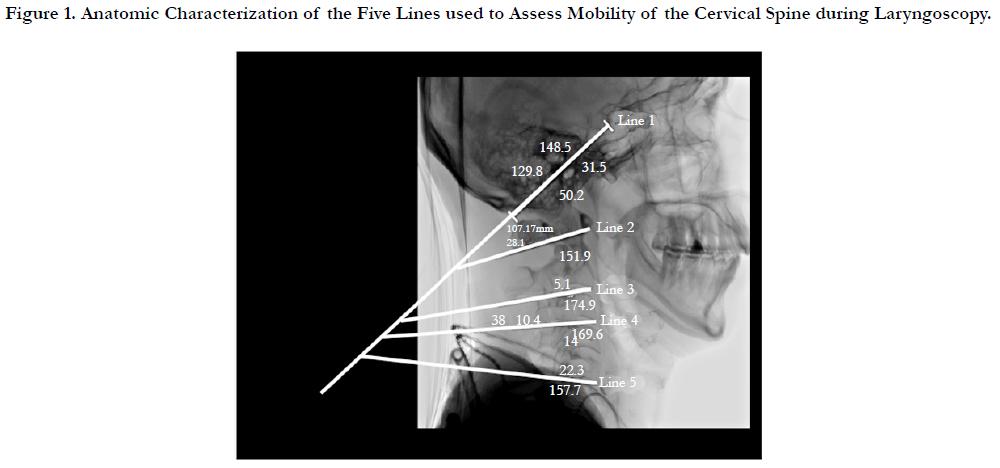
Five lines were constructed and used for the measurements of CS mobility as illustrated in Figure 1:
• Line 1, between the occipital base to the floor of the "sella turcica" (base of the skull).
• Line 2, between the lower edge of the anterior arch of C1 to the lower edge of the spinous process of C1.
• Line 3, between the lower edge of the vertebral body of C2 to the lower edge of spinous process of C2.
• Line 4, between the bottom edge of the vertebral body C3 to the lower edge of the spinous process of C3.
• Line 5, between the bottom edge of the vertebral body of C5 to the lower edge of the spinous process of C5.
To quantify mobility of the neck and cervical spine, seven angles were determined via intersections of the lines defined above. The angle between Line 1 and Line 2: corresponded to movement at the occipito-atlantal joint only. The angles between Line 1 and either Line 3, Line 4, or Line 5 corresponded to movement at the occipito-atlantal joint as well as within the cervcial spine. The angle between Line 2 and either Line 3, Line 4, or Line 5 corresponded to motion only intrinsically within the cerivcal spinal vertebrae. Smaller angles indicated less extension integrated over the corresponding vertebral segments.
To quantify the degree of mobilization of laryngeal structures, the minimum distance between the tip of each laryngoscope and the closest point of the most anterior portion of the cervical spine was deteremined.
All images and measurements were performed by neuro-radiologists.
Given the small sample size, a formal statistical analysis was not feasible. Data are reported in summary format. In addition, each angle obtained during laryngoscopy was subtracted from the angle determined in the neutral position for each patient. Medians and ranges were reported for each of the differences in angles.
Results
Five patients participated in the study of whom 2 were male (40%). Median age was 57 years, with a range from 34 years to 74 years.
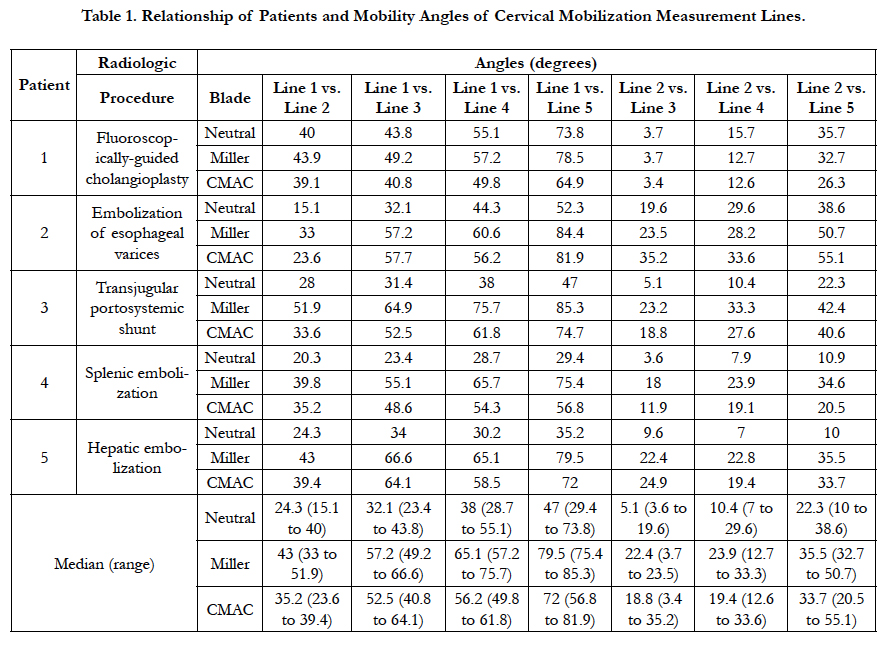
The degrees of angulation were measured in the cervical segments in the neutral head position, when viewing the glottis with direct laryngoscopy with Miller blade, and during video laryngoscopy with CMAC with a D blade. These data are summarized in Table 1. OTI maneuvers with both the Miller blade and the CMAC system increased all angles compared to those obtained in the neutral position and occurred with respect to the skull based and intrinsically within the cervical spine. The increase in most angles were greater with DL than with the use fo the CMAC system.
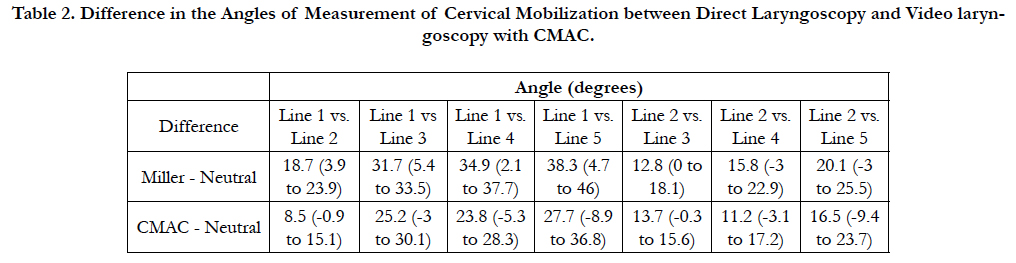
Each angle obtained during laryngoscopy with both Miller blade and CMAC device were subtracted from the corresponding angle obtained with the patient in the neutral position and these data are summarized in Table 2. There was a tendancy to generate a greater neck extension during DL with a Miller blade as compared to that obtained during VL with the CMAC system both in comparison to skull base and intrinsically with the cervical spine.
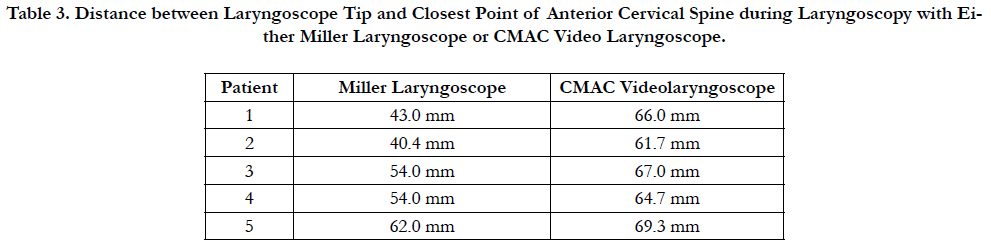
In all five patients, a greater anterior displacement of airway structures was obtained with the CMAC VL compared to the Miller laryngoscope as determined by a greater distance achieved between the tip of the laryngoscope and closest and most anterior portion of the cerivcal spine as shown in Table 3.
Discussion
To our knowledge, the difference in CM during DL has not been previously studied with a Miller blade compared to VL CMAC with D-Blade blade in healthy patients, as measured by fluoroscopy. Previous studies evaluated the cervical mobilization by fluoroscopy during laryngoscopy with Macintosh blade [9, 10]. In these studies the joints C1 and C2 showed the greatest range of motion relative to the occiput.
Our study suggested that the extension of the CS was higher with DL with a Miller blade that when CMAC VL was used. This finding was observed in the mobilization of all joints evaluated from C1 to C5 relative to the skull base, but was also intrinsically within the cervical spine. This shows an advantage regarding this device when compared to the standard method of OTI, which is especially useful in patients with cervical pathology. A reduction in the range of cervical spine motion during OTI in patient with cervical pathology is critical as it reduces the risk of causing or worsening a spinal cord injury at that level [3].
In patients with CT, an OTI rapid sequence accompanied by manual inline stabilization is recommended for securing the airway in emergency situations [11]. Manual in line stabilization reduces the possibility of moving the spine during DL, but it may hinder laryngoscopy [12, 13]. Although manual inline stabilization can also be used with VL, its potential to hinder OTI is much lower because it does not require alignment of the laryngeal, pharyngeal and oral axes [7].
The study findings support the use of CMAC with a D-Blade over direct laryngoscopy in patients with cervical pathology, since the reduction in CM is a protective factor against the risk of exacerbating a spinal cord injury. An interesting aspect is that the study not only proves a reduction in CM in subjects in which the VL CMAC with D-Blade blade was used; the analysis of the fluoroscopic images helps explain why the visualization of glottal and epiglottal tissues is optimized with VL [14, 15].
Several design features improve the glottal CMAC visualization [16]. The blade is thinner than traditional blades (maximum 14 mm) with a beveled edge which reduces the chance of oral or dental trauma. The optical device includes a chip that produces an image of 320x240 pixels from a lens located in the distal third of the blade and creates a viewing angle of 80 degrees. It also has a high power light-emitting diode and an anti-fogging system [15]. This design magnifies the image and extends in front of the lens in 60 degrees in the longitudinal direction and 80 degrees crosswise offering an advantage for patients with an anterior located larynx [17, 18].
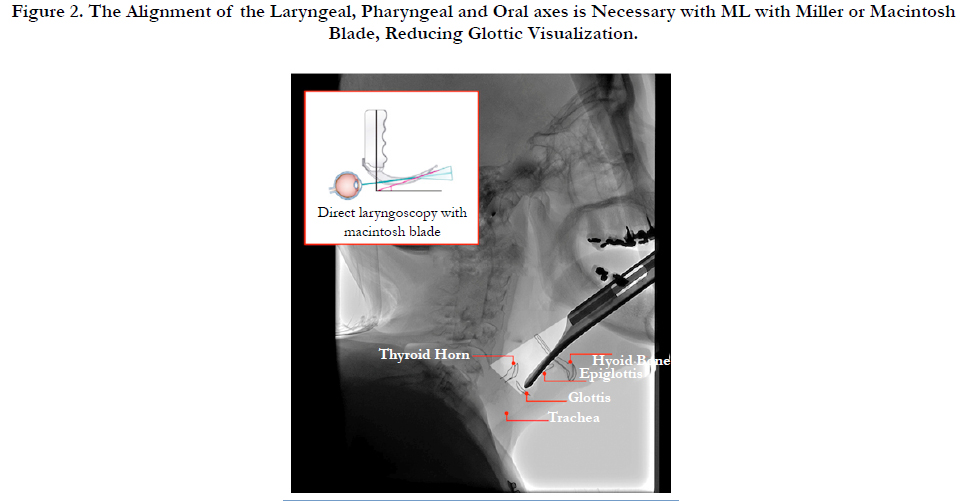
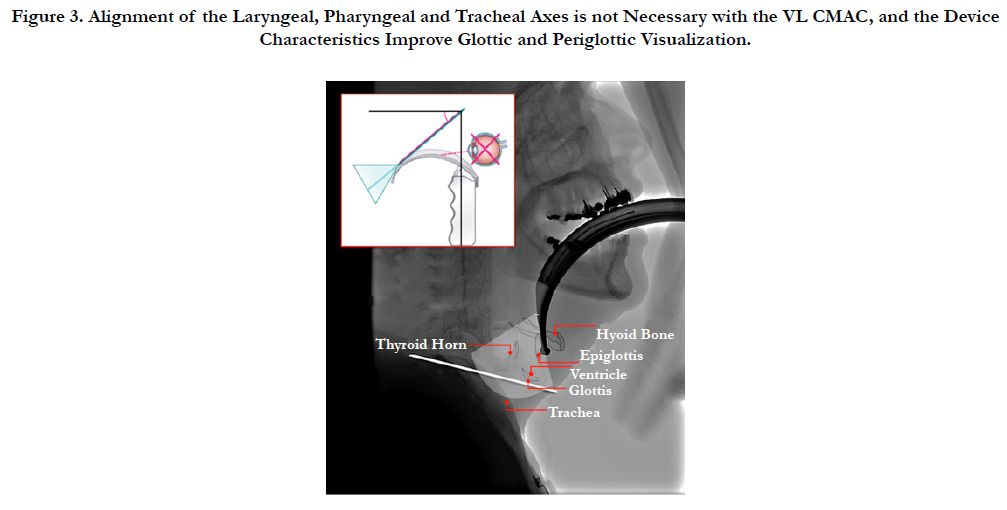
The CMAC VL device allows the retraction of periglotic soft tissue without aligning the laryngeal, pharyngeal and oral axes as illustrated in Figure 2 [19], which happens with conventional laryngoscopes (see Figure 3). Clinical studies have compared the display quality between different VL; taking into account light intensity, contrast between anatomical structures and view field [20]; finding clinical and design advantages in favor of CMAC that could explain the high efficiency in patients with predictors of a difficult airway [21].
The 40º curvature of the blade D-Blade contrast with 18º of traditional McIntosh blade [8], favoring a more anterior location of the tip of the blade with an anterior displacement of the vallecula [22]. This creates a distension of the supra-glottis structures below the blade, visually separating the glottis and facilitating the differentiation, increasing the success rate. This is illustrated en Figure 3.
We were also able to demonstrate that, despite less cervical spine extension, laryngoscopy with the CMAC VL was able to provide great anterior displacement of the anterior supralaryngeal structures and a wider field of view than DL with a Miller blade. Specifically, in each case, there was a largery distance between the CS and the tip fo the laryngoscope. See the Figures 2 and 3 to compare.
The main limitation of this study is its small sample value. This pilot study may be complemented by a study of greater size and statistical power. Our institution underwent a practice change that limited recruitment of more patients for this series. The Miller straight blade was used in this work as comparative to Cmac. This decision was based on the fact that in our hospital the DL Miller blade is used routinely. Previous studies have shown that differences in CM valued by fluoroscopy were comparable during a DL with Miller, Macintosh or McCoy blades [23]. We believe that our results can be extrapolated to the use of Macintosh blades. Finally, the lack of monitoring of the laryngoscopy technician may generate observer bias, and a tendency to overestimation of the beneficial effect of video laryngoscope.
Conclusions
With the use of fluoroscopy, we were able to demonstrate that laryngoscopy with a CMAC VL provided a wider separation of anterior airway structures and the cerivcal spine despite less intrinsic and extrinsic CS motion during laryngoscopy compared to laryngoscopy with a Miller laryngoscope. This, in patients with known or presumed cervical spine injuries, the use of the CMAC VL can limit CM during airway management without sacrificing airway structure displacement during laryngoscopy.
References
- McLeod ADM, Calder I. Spinal cord injury and direct laryngoscopy- The legend lives on. Br J Anaesth. 2000 Jun;84(6):705-709.
- Martini RP, Larson DM. Clinical Evaluation and Airway Management for Adults with Cervical Spine Instability. Anesthesiol Clin. 2015 Jun 30;33(2):315-327.
- Stein D, Pineda J, Roddy V, Knight W. Emergency Neurological Life Support: Traumatic Spine Injury. Neurocrit Care. 2015 Dec 1;23(2):S155-164.
- Healy DW, Picton P, Morris M, Turner C. Comparison of the glidescope, CMAC, Storz DCI with the Macintosh laryngoscope during simulated difficult laryngoscopy: a manikin study. BMC Anesthesiol. 2012 Jun 21;2(1):11.
- Jain D, Bala I, Gandhi K. Comparative effectiveness of McCoy laryngoscope and CMAC(®) videolaryngoscope in simulated cervical spine injuries. J Anaesthesiol Clin Pharmacol. 2016 Jan;32(1):59-64.
- Stroumpoulis K, Pagoulatou A, Violari M, Ikonomou I, Kalantzi N, Kastrinaki k, et al. Videolaryngoscopy in the management of the difficult airway: a comparison with the Macintosh blade. Eur J Anaesthesiol. 2009 Mar 1;26(3):218-222.
- Cavus E, Thee C, Moeller T, Kieckhaefer J, Doerges V, Wagner K. A randomised, controlled crossover comparison of the CMAC videolaryngoscope with direct laryngoscopy in 150 patients during routine induction of anaesthesia. BMC Anesthesiol. 2011 Mar 1;11(1):6.
- Jain D, Dhankar M, Wig J, Jain A. Comparison of the conventional CMAC and the D-blade CMAC with the direct laryngoscopes in simulated cervical spine injury-a manikin study. Braz J Anesthesiol. 2014 Aug 31;64(4):269-274.
- Sawin PD, Todd MM, Traynelis VC, Farell SB, Nader A, Sato Y, et al. Cervical spine motion with direct laryngoscopy and orotracheal intubation. An in vivo cinefluoroscopic study of subjects without cervical abnormality. Anesthesiol. 1996 Jul 1;85(1):26-36.
- MacIntyre P, McLeod A, Hurley R, Peacock C. (1999) Cervical spine movements during laryngoscopy. Anaesthesia. 1999;54:413-418.
- Theodore N, Hadley M, Aarabi B, Dhall SS, Gelb DE, Hurlbert RJ, et al. Prehospital cervical spinal immobilization after trauma. Guidelines for the management of acute cervical spine and spinal cord injuries. Neurosurgery. 2013 Mar;72(S2):22-34.
- Thiboutot F, Nicole P, Trépanier C, Turgeon AF, Lessard MR. Effect of manual in-line stabilization of the cervical spine in adults on the rate of difficult orotracheal intubation by direct laryngoscopy: a randomized controlled trial. Can J Anesth. 2009 Jun 1;56(6):412-418.
- Suppan L, Tramèr MR, Niquille M, Grosgurin O, Marti C. Alternative intubation techniques vs Macintosh laryngoscopy in patients with cervical spine immobilization: systematic review and meta-analysis of randomized controlled trials. Br J Anaesth. 2016 Jan;116(1):27-36.
- Niño MC, Ramirez FJ, Perez AC. Radiological measurement of cervical angulation comparing direct laryngoscopy with miller blade vs. Lightwand. Rev Col Anest. 2011 Apr;39(1):119-127.
- Hagber C. Benumof and Hagberg’s Airway Management. 3rd ed. Elservier: Philadelphia; 2012 Sep.1088.
- Chemsian RV, Bhananker S, Ramaiah R. Videolaryngoscopy. Int J Crit Illn Inj Sci. 2014 Jan-Mar;4(1):35–41.
- Aziz M, Brambrink A. The Storz CMAC video laryngoscope: Description of a new device, case report, and brief case series. J Clin Anesth. 2011 Mar;2(2):149–152.
- Enomoto Y, Asai T, Arai T, Kamishima K, Okuda Y. Pentax-AWS, a new videolaryngoscope, is more effective than the Macintosh laryngoscope for tracheal intubation in patients with restricted neck movements: A randomized comparative study. Br J Anaesth. 2008 Apr;100(4):544–548.
- Malik MA, Subramaniam R, Churasia S, Maharaj CH, Harte BH, Laffey JG. Tracheal intubation in patients with cervical spine immobilization: a comparison of the Airwayscope, LMA CTrach, and the Macintosh laryngoscopes. Br J Anaesth. 2009 May;102(5):654-661.
- Cierniak M, Timler D, Wieczorek A, Sekalski P, Borkowska N, Gaszynski T. The comparison of the technical parameters in endotracheal intubation devices: the Cmac, the Vividtrac, the McGrath Mac and the Kingvision. Clin Monit Comput. 2016 Jun 29;30:379–387.
- Ng I, Hill AL, Williams DL, Lee K, Segal R (2012) Randomized controlled trial comparing the McGrath videolaryngoscope with the CMAC videolaryngoscope in intubating adult patients with potential difficult airways. Br J Anaesth. 2012 Sep;109(3):439-443.
- Missaghi SM, Krasser K, Zadrobilek E. The D-BLADE: a significantly modified blade for the Storz CMAC Videolaryngoscopy System. Int J Airway Manage. 2010 Jan – 2011 dec;(6).
- LeGrand SA, Hindman BJ, Dexter F, Weeks JB, Todd MM. Craniocervical motion during direct laryngoscopy and orotracheal intubation with the Macintosh and Miller blades: an in vivo cinefluoroscopic study. Anesthesiol. 2007 Dec;107(6):884-891.