Non-Invasive Implanto Prosthetic Rehabilitation in the Lower Arch Subsequent to Ameloblastoma Removal. A Case Report
Alberto Maltagliati1, Samer Helal Zaky2, Andrea Ottonello1*
1 Dipartimento di Scienze Chirurgiche e Diagnostiche Integrate, Università degli studi di Genova, Genoa, Italy.
2 Center for Craniofacial Regeneration, Department of Oral Biology, University of Pittsburgh, USA.
*Corresponding Author
Andrea Ottonello DMD PhD,
Università degli studi di Genova,
Dipartimento di Scienze Chirurgiche e Diagnostiche Integrate,
Largo Rosanna Benzi 10, 16132 Genoa, Italy.
E-mail: andrea.ottonello@unige.it
Article Type: Case Report
Received: March 05, 2015; Accepted: May 23, 2015; Published: May 26, 2015
Citation: Alberto Maltagliati, Samer Helal Zaky, Andrea Ottonello (2015) Non-Invasive Implanto Prosthetic Rehabilitation in the Lower Arch Subsequent to Ameloblastoma Removal. A Case Report. Int J Dentistry Oral Sci. 2(5), 72-74. doi: dx.doi.org/10.19070/2377-8075-1500015
Copyright: Ottonello A© 2015. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Aim: Describing the surgical/therapeutic and the prosthetic/functional approaches for the treatment and rehabilitation of a patient with an ameloblastoma in the posterior area of mandible.
Materials and Methods: Enucleation of the lesion took place by surgical resection with bone margin extending to more
than 1cm beyond the lesion’s macroscopic margins, without performing guided bone regeneration. A year after surgery, a panoramic radiograph (OPG) was performed and seven implants were inserted to rehabilitate the lower arch. The upper arch was rehabilitated with implant-prosthetic full-arch structure (flat-one-bridge) and immediate functional loading within 72 hours.
Results and Conclusions: A 30 month follow-up shows good peri-implant tropism with bone margins continuity and osteointegration to the bone previously compromised by the lesion. The non-invasive treatment of lesions of maxillary bones is very useful to maintain the interarch occlusal relationship since it accelerates bone healing and optimizes the soft tissues morphology.
2.Introduction
3.Materials and Methods
4.Results and Conclusive Considerations
5.References
Keywords
Ameloblastoma; Dental implants; Non-Invasive Implanto-Prosthetic Rehabilitation
Introduction
Ameloblastoma is a benign epithelial odontogenic tumour first described by Cusack in 1827 [1]. It presents 1% of all oral tumours and 18% of tumours of odontogenic origin with age peak at the 4th decade of life [2]. It affects primary the posterior mandible (75%) [3] with annual incidence per million of 1.96 among black males, 1.2 among black females, 0.18 among white males and 0.44 among white females [4]. Its symptoms include painless swelling that may cause severe facial deformity, teeth loss, ulcers and periodontal problems. Upon palpation, ameloblastoma is known by its “egg shell” crepitus and could generally be diagnosed by its “honey comb” or “soap bubble” radiographic appearances indicating a multilocular lesion. The unilocular form of ameloblastoma is radiographically similar to a cystic lesion and rarely, as in our case, engulfing a tooth simulating a dentigerous cyst.
The therapy of choice for ameloblastoma is surgical excision with safety margins with simulation of revascularization for healing and osseous repair. [5] Since no radio or chemotherapies are indicated for ameloblastoma [6, 7], the patient can be rehabilitated with non invasive dental implants techniques while preventing direct implants insertion at the surgical excision bed.
Materials and Methods
We report here a case of rehabilitation by implant therapy for a 59 year old white male affected by ameloblastoma in the left ascending ramus of the mandible. (Figure.1A) The tumour was enucleated and removed according to the conventional surgical protocol [8] with extended bone margins 1cm beyond the evident macroscopic boundaries of the lesion. The tumour was investigated by histology (Figure.1B).
Figure 1. A: Solid multicystic ameloblastoma of the left posterior mandible in a 59 y.o. white male patient. The lesion was removed according a normal surgical protocol. B: Histological analysis of the ameloblastoma shows epithelial palissading columnar cells with hyperchromatic nuclei around a cyst-like cavity. Scale bar: 50 μm.
A full thickness flap was raised and the lesion was separated from the surrounding tissues and released. Particular attention was given to separate the wall of the lesion from the bone and mucosa without laceration to reduce any probability of eventual recurrence. All epithelial residues were removed afterwards by a surgical curette. To ensure repopulation of the defect by the natural coagulum and active osteoblasts we did not use any type bone graft.
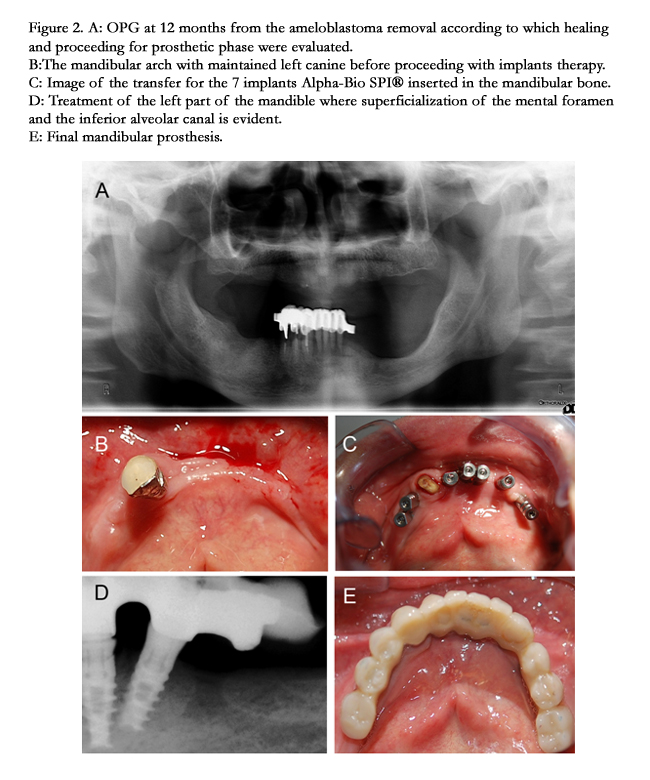
In our case, to monitor healing time for rehabilitation, the patient was subjected to periodic OPG along the following 12 months (Figure.2A). The patient was then subject to rehabilitation by selftapping implants with immediate loading. The mandibular left canine not affected by the pathology was conserved in place to maintain unilateral canine guidance and the preserve the vertical dimension for the planned prosthetic phase (Figure.2B). The canine was extracted at the conclusion of the rehabilitation phase.
We employed Alpha-Bio SPI© conical implants with self tapping/ drilling apices for maximum primary stability. Seven implants were inserted in the mandibular bone in the interforamenal region with distal elements extension on the right and left canines (Figure.2C&D). The implants reached a torque of 50 N/cm and the prosthesis was screwed at 25 N/cm according to the manufacturer’s instructions (Figure. 2C-E).
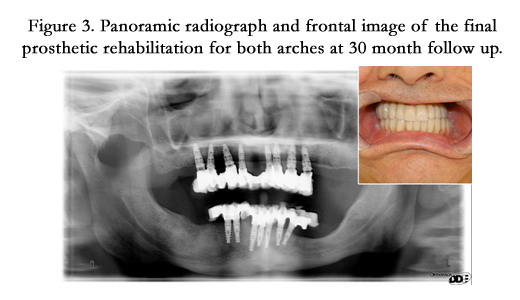
After evaluation, we decided not to insert any implants at the previously operated area due to proximity to the inferior alveolar nerve and to the mental foramen (Figure.2D). We managed to compensate the postoperative osseous defect (Figure.3) prosthetically by a gingival flange in occlusion with the rehabilitated maxillary arch (8 implants were used in the maxilla). This results in “Flat-One-Bridge” full arch rehabilitation with self tapping and immediately loaded implants at 72 hours [9].
Figure 2. A: OPG at 12 months from the ameloblastoma removal according to which healing and proceeding for prosthetic phase were evaluated. B:The mandibular arch with maintained left canine before proceeding with implants therapy. C: Image of the transfer for the 7 implants Alpha-Bio SPI® inserted in the mandibular bone. D: Treatment of the left part of the mandible where superficialization of the mental foramen and the inferior alveolar canal is evident. E: Final mandibular prosthesis.
Figure 3. Panoramic radiograph and frontal image of the final prosthetic rehabilitation for both arches at 30 month follow up.
Results and Conclusive Considerations
The most common mandibular rehabilitation option after ameloblastoma resection is bone grafting with or without supporting implants. [10-12] In addition, distraction osteogenesis has been reported for mandibular rehabilitation, yet with the lengthy and complicated technique the long term outcomes are also satisfactory [13]. In this study, we employed solely dental implants for mandibular rehabilitation without bone grafting or distraction osteogenesis. We followed up the herein mentioned case for 12, 18, 24 and 30 months (Figure.3) by OPG and transmucosal probing for the implants collar. The implants had good tropism and the bone healing from the removed lesion showed continuous and integrated margins. No loss of attachment from the peri-implant collar was evident nor any grade of bone resorption. Our prosthetic implant rehabilitation for this case report demonstrates and confirms that the non invasive treatment with immediate loading implants for maxillo-facial lesions represents the gold standard and remains an important indication for maintaining proper occlusal relationship while accelerating the bone healing process and optimizing the contour of soft tissue.
References
- Cusack JW (1827) Report of the amputations of the lower jaw. Dublin Hosp Rec 4: 1-38.
- Gordon J (2008) Clinical Quiz: Painless Mass. Appl Radiol 3: 8-10.3
- Reichart PA, Philipsen HP, Sonner S (2007) Ameloblastoma: biological profile of 3677 cases. Eur J Cancer B Oral Oncol 31B: 86–99.
- Shear M, Singh S (1978) Age-standardized incidence rates of ameloblastoma and dentigerous cyst on the Witwatersrand, South Africa. Community Dent Oral Epidemiol 6(4): 195–199.
- Nastro Siniscalchi E, Catalfamo L, Rinaldo F, Ieni A, Tuccari G, et al. (2012) Odontoameloblastoma: five years follow up of a surgical case and review of literature. Eur Rev Med Pharmacol Sci 16(4): 125-128.
- Atkinson CH, Harwood AR, Cummings BJ (1994) Ameloblastoma of the jaw. A reappraisal of the role of megavoltage irradiation. Cancer; 53(4): 869–873.
- Miyamoto CT, Brady LW, Markoe A, Salinger D (1991) Ameloblastoma of the jaw. Treatment with radiation therapy and a case report. Am J Clin Oncol 14(3): 225–230.
- De Silva I, Rozen WM, Ramakrishnan A, Mirkazemi M, Baillieu C, et al. (2012) Achieving adequate margins in ameloblastoma resection: the role for intra-operative specimen imaging. Clinical report and systematic review. PLoS One 7(10): e47897.
- Bucci Sabbatini V (2010) New frontiers in immediate loading. Martina, Bologna.
- Schlieve T, Hull W, Miloro M, Kolokythas A (2015) Is immediate reconstruction of the mandible with nonvascularized bone graft following resection of benign pathology a viable treatment option. J Oral Maxillofac Surg 73(3): 541-549.
- Avraham T, Franco P, Brecht LE, Ceradini DJ, Saadeh PB, et al. (2014) Functional outcomes of virtually planned free fibula flap reconstruction ofthe mandible. Plast Reconstr Surg 134(4): 628e-34e.
- Ooi A, Feng J, Tan HK, Ong YS (2014) Primary treatment of mandibular ameloblastoma with segmental resection and free fibula reconstruction: achieving satisfactory outcomes with low implant-prosthetic rehabilitation uptake. J Plast Reconstr Aesthet Surg 67(4): 498-505.
- Bousdras VA, Kalavrezos N (2014) Distraction osteogenesis of free flap reconstructed mandible following ameloblastoma resection for optimal functional rehabilitation. Ann Maxillofac Surg 4(2): 237-239.