Influence of Tooth Thickness on Degree of Conversion of Photo-Activated Resin Composite Irradiated Through the Tooth
Alexander Tarimo S, Mabula Machibya F*, Zhi Min Z
Department of Orthodontics, Paedodontics and Community Dentistry, Muhimbili University of Health and Allied Sciences, Dar es salaam, Tanzania.
*Corresponding Author
Dr. Ferdinand Mabula Machibya,
Lecturer (Orthodontist), Department of Orthodontics,
Paedodontics and Community Dentistry,
Muhimbili University of Health and Allied Sciences, P. O. Box 65014, Dar es salaam, Tanzania.
Tel: +255-222151135
Fax: +255222150465
E-mail: frmachibya@yahoo.com
Received: February 18, 2017; Accepted: March 22, 2017; Published: March 24, 2017
Citation: Alexander Tarimo S, Mabula Machibya F, Zhi Min Z (2017) Influence of Tooth Thickness on Degree of Conversion of Photo-Activated Resin
Composite Irradiated Through the Tooth. Int J Dentistry Oral Sci. 4(3), 450-456. doi: dx.doi.org/10.19070/2377-8075-1700089
Copyright: Mabula Machibya F©2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: To investigate the influence of trans-dental photo-curing on the degree of conversion (DC) of a resin composite irradiated by a light curing unit operating in different curing modes.
Methods: A curing lamp having six different curing modes was used for indirect photo-activation of a Nanocomposite through different thicknesses of tooth tissues. Fourier transformation infrared (FTIR) spectroscopy was used to determine DC. Three main experimental groups were formed in accordance with the 0.5mm, 1mm and 1.3mm, tooth thicknesses which were further subdivided into six minor groups formed according to irradiation modes. Control groups employed direct irradiation.
Results: For each of the six light curing modes, the average DC decreased with increase in intervening tooth thickness. Among the groups, 0.5mm had the highest DC mean values, 21.5mm group had the lowest mean values (P<0.05). The composite resin showed lower DC mean values when irradiated indirectly compared to control direct curing (P<0.05). DC mean values for turbo and high light modes were statistically significantly higher compared to Normal, Soft Start, Pulse and Pulse Soft light modes.
Conclusions: A Nano-composite resin cured through different tooth thickness has lower DC compared to direct curing. DC decreases with increasing intervening tooth thickness. DC mean values for turbo and high light modes were statistically higher compared to normal, soft start, pulse and pulse soft light modes.
2.Introduction
2.1 Assessment of Light-cured Composite Resin Polymerization Degree
3.Methods and Materials
3.1 Curing Technique
3.2 FTIR Spectroscopy technique- Evaluation of Degree of conversion (DC)
3.3 Statistical Analysis
4.Results
4.1 Assessment of Conversion Degree (DC)
5.Discussion
5.1 Influence of trans-dental curing on the composite resin DC
5.2 Influence of different curing modes on the polymerization degree of composite resins
6.Conclusions
7.References
Keywords
Indirect Curing; Degree of Conversion; Irradiation Modes; Photosensitive Composite Resin; FTIR.
Introduction
Dental caries is a bacterial infectious disease of the hard dental tissues, and is one of the most common human diseases affecting a vast majority of adults and children [1]. The current treatment for caries aims at filling technology, and the main restorative materials are metal alloys, ceramics and composite resin materials. Following research development of the dental materials, light-cured composite resins, due to their good mechanical strength and aesthetic performance, are widely used in the clinics [2]. According to modern restoration concepts, during cavity preparation more tooth structure may be retained. Clinical cavity filling procedures meet complex cavity shapes. In order to obtain composite restorations with minimal level of shrinkage while maintaining the greatest degree of polymerization, ensuring marginal seal and adequate bonding strength, placement of composite resin in layers and successive curing is widely applied [3]. The filling thickness of the material should be determined by the properties of the materials and the curing device performance. It is advocated that each filling layer thickness should be approximately 2mm, while selecting the soft-start mode to further reduce polymerization shrinkage [4]. Incomplete curing can lead to composite resin restoration early degradation, wear and affect the functional durability, eventually leading to restoration failure. The depth of cure (DoC) and degree of conversion (DC) are also affected by material particle size, light intensity, curing time and variety of other factors [5, 6]. Achieving optimum degree of polymerization is still a challenge to dentists all over the world.
Polymerization degree of photo-sensitive composite resins is influenced by many factors, such as the type of curing light, irradiation modes and intervening tooth structure. Depth of cure (DoC) as well as DC governs and influence the quantity and quality of polymerization [7]. There are at least four main types of curing lights, quartz-tungsten halogen bulbs (QTH), plasma-arc lamps (PAC), argon-ion lasers, and light emitting diodes (LED).
]
LEDs have been hailed as presenting greater efficacy on polymerization of light cured composites. LEDs have the advantages of using less energy, longer working life, and giving out light with a wavelength between 410 ~ 490nm, which is the light spectrum most effective for light curing. The 468nm wavelength is the absorption peak of camphorquinone (CQ), a photo-initiator present in most modern composite resins [8-12]. Studies show that, LED light output power is related to different curing modes [12]. Different light curing techniques (irradiation modes) have been introduced to the dental profession with claims that they significantly offer polymerization advantages than the traditional methods by decreasing internal stresses in order to achieve better marginal adaptation in bonded composite resin restorations [13, 14]. There are at least 6 different irradiation modes, which are standard mode (normal mode), soft start mode, pulse soft start mode, pulse mode, high-light mode and turbo mode. Polymerization shrinkage during composite resin filling process is a major drawback. Composite resins gradually harden during curing process through reaction between monomers, accompanied by dense packing of molecules to form complex and long polymer chains, resulting in the reduction in total volume of the resin, leading to polymerization shrinkage or curing shrinkage [15]. Soft Start polymerization has been suggested as a clinical technique to reduce contraction stress [4, 16]. The Soft Start (SS) curing mode is the one in which curing process begin with a low intensity and finishes with a high intensity thus lowering the speed of monomer conversion. This mode reduces the time to reach the gel point, thus offering sufficient time for the resin flow and make up for the polymerization shrinkage generated by the reaction; however some authors have reported drawbacks with the soft start technique despite the claimed advantages [17-19]. The pulse soft (PS) mode is the one in which light intensity gradually increases, each increase separated by a dark interval. The Pulse (P) curing mode is a series of exposure pulses, each separated by a dark interval [20-22]. Turbo and high intensity modes are based on a concept of total energy introduced to decrease exposure time and are claimed to have a greater depth of cure compared to conventional lights [23]. A layering technique with filling thickness of 2mm or less is usually recommended [8, 23], in order to improve polymerization efficiency and decreasing the complexity and time to place and cure a composite filling, reduce polymerization shrinkage, improve cavity margin seal integrity [24, 25]. Some authors [26, 27] advocate a composite curing technique through the tooth structure, in order to maximize the retention of tooth structure. Through tooth structure indirect exposure may reduce conversion degree and depth of cure [28]. When the light beam transmits across the tooth structure, due to the presence of light absorption and scattering, can lead to incomplete cure of composite resins. This phenomenon is influenced by the thickness of tooth structure and optical properties [7, 29, 30].
Several methods can be employed to measure polymerization degree of a cured composite resin. These techniques include the ISO 4049 standard technique which is a simple test method measuring DoC. This method measures the height of the remaining hardened material after scrapping away the unset soft material. DoC is then calculated as 50% of the remaining specimen height. Optical method is another simple method indirectly measuring DoC of light-cured composite resins. An optical microscope is employed to visualize photo-curable resin transparency changes in the cured and uncured resin. There is a clear distinction by the transparent lines; a resin height above the transparent line is termed DoC. Like the scraping method, optical method can not specify curing resin quality at any given point [31, 32]. Stepped surface hardness is another method of measuring DoC using a micro-hardness indenter, which measures resin composite hardness at different levels along the length of the cured resin composite [33-36]. Although the surface hardness method shows curing degree of light-cured composite resin gradual decrease from the top surface, it cannot quantitatively indicate the actual level of conversion. Employing Fourier transform infrared spectroscopy (FTIR) to observe degree of conversion of composite resin double bonds is a more direct and more objective methods [35]. Through an infrared absorption spectrometer wavelength measurements are recorded. The absorption peak most commonly measured is the aliphatic C=C bonds in the mid-infrared (MIR) region at 1638cm-1 and the aromatic C-C reference peak at 1608cm-1. During polymerization, this absorption height decreases as the carbon-carbon double bonds react via free radical addition. The ratio of the absorbance intensities of C=C to C-C is compared before and after polymerization to determine the percentage of unreacted carbon double bonds. The DC is obtained by subtracting this percentage from 100 [37-42].
To date, there are only few researches devoted to studying the effects of through- tooth structure indirect light curing of composite materials, and clarify that the intervening tooth structure may affect the final properties of the composite restorations [43, 44]. Some studies have shown that curing through enamel is just one-third to two-thirds as effective as direct curing and is appropriate only when there is no alternative [45, 46]. Another research reported the least critical record situation when 0.5mm of composite Z100 was cured through 1mm enamel [47]. Although the experiments involved through-tooth-tissue curing, only the quantitative analyses of hardness-based measurements on the degree of polymerization were employed, no qualitative analyses were done.
The current study aimed at evaluating the tooth thickness influence on degree of conversion of a Nano-composite using LED light operating in different irradiation modes. This experiment focused on the indirect exposure through the tooth structure of composite resin, at the same time taking into account the effects of different light curing modes on the polymerization of composite resin. Using dental tissue slices prepared from extracted human teeth, to establish in vitro indirect composite resin curing models.
Methods and Materials
Ethical clearance to conduct the study was obtained from the ethical committee of the Jilin University, China. Recently extracted caries-free human molar teeth were collected. The teeth were temporarily stored for a period of seven days in 8% formalin solution of for disinfection and fixation.
Dental calculus and attached periodontal soft tissues on the surfaces of the teeth were removed with a hand scaling instrument, cleaned with running water in a rubber cup and slurry of pumice and then kept in 1% thymol solution at room temperature for storage.
The teeth were sliced into small squared pieces about 6 x 6 mm (Figure 1), at different thicknesses using a 0.1mm thick diamond disc (Jiangyin disc, Jiangsu, China). The thickness of the slices was approximately 0.5mm, 1mm, 1.5mm. The thickness for each slice was measured using a digital caliper (Shan 132A Series Digital Caliper, Guilin China) at three different points to get an average thickness. The dental slices were allocated into six groups according to their thickness.
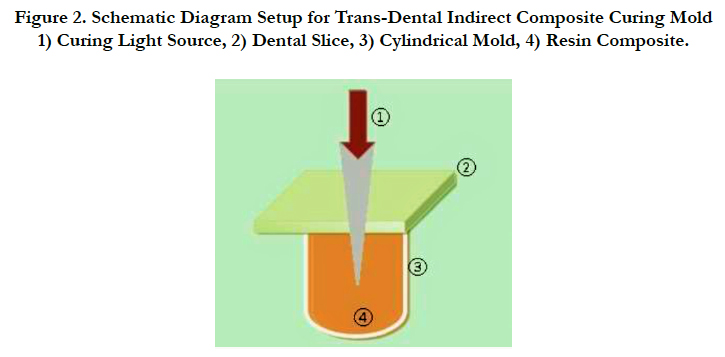
The prepared dental slices were removed from the water, treated for 15 seconds with 37% phosphoric acid etching agent (SCi- PHARM Gel Etch, USA), the etchant was washed away by water spray and air dried. A thin layer of single bond adhesive system (DenFilTM Flow adhesive, USA) was applied on the side of the tooth slice facing the composite mold by using a non-linting brush in accordance with the manufacturer’s instructions. In order to obtain a thin layer of adhesive on the tooth as per requirement of a standard composite filling procedure, air spray was used to blow away any excess. The bonding agent was then indirectly cured for 20 seconds by the LED light unit (Dr’s Light, Good Doctors Co, Ltd. South Korea) by transmitting the light through the tooth slice. Figure 2 shows a schematic diagram of the composite resin trans-dental curing in vitro experiment model setup.
Figure 2. Schematic Diagram Setup for Trans-Dental Indirect Composite Curing Mold. 1) Curing Light Source, 2) Dental Slice, 3) Cylindrical Mold, 4) Resin Composite.
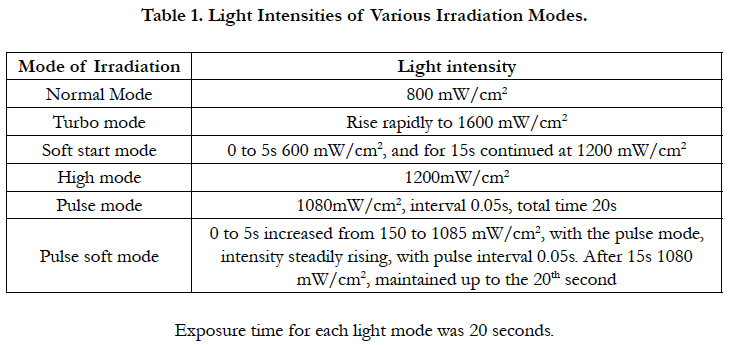
The curing light operated in six different modes; normal, high, pulse, soft start, pulse soft and turbo modes was done using LED light curing unit (Dr’s Light, Good Doctors Co, Ltd. South Korea). The tip of the light source was placed close enough to touch the tooth specimen being irradiated. Lateral direct light was prevented from curing the composite by using a shutter fabricated from light-proof x-ray film paper folds, so that only light filtered through the dental slices was allowed to cure the composite. Table 1 shows the light curing modes, exposure time and the light intensities for each curing technique. At the beginning of the experiment a dental radiometer (cure rite Caulk Dentsply, Milford, USA) was used for the measurements of power output of the curing light (Figure 3).
The composite resin prepared for FTIR spectroscopy analysis was meticulously packed into cylindrical molds 4mm inner diameter and 2mm height: Whereas, the control direct curing groups used 10mm height. The composite resin was either indirectly cured by light transmitted through the tooth slices (experiment) or cured directly (control). Care was taken to avoid air voids during composite placement by adequate condensing. Immediately after photo curing, at room temperature and under light protection, each cured specimen was reduced into fine powder by using a diamond disc 0.1mm thick with 20mm diameter (Jiangyin disc, Jiangsu, China) mounted on a slow speed hand-piece motor. The fine powder was collected and subjected to the FTIR spectrophotometer (Nicolet 5700, Thermo Electron Corporation, Verona Madison USA) for analysis (Figure 4).
Ten milligrams of the composite powder was mixed with 100 mg of potassium bromide (KBr) powder salt. This mixture was placed into a pelleting device and then pressed in a hydraulic press (Carver Laboratory Press, Wabash, St. Morris, USA) with a load of 8 tons to obtain a pellet. This pellet was then placed in a holder attachment within the spectrophotometer for analysis. The uncured composite was analyzed using a metal siliceous window. The measurements were recorded in absorbance mode with the FTIR Spectrophotometer as previousely described by Obici et al., [48]. All experiments were carried out in triplicates. The FTIR analysis of C=C peaks was done using Origin Lab Pro 8.6.0 software.
Statistical Package for the Social Sciences (SPSS) 18.0, (Chicago, IL, USA), was used to analyze original data collected. A paired sample t-test was run to compare the mean depths of cure and degrees of conversion for the experimental (indirect curing) and control (direct curing) groups. For the experimental groups oneway ANOVA tests were also done to compare DCs between the groups according to irradiation mode and tooth thickness. Multiple comparisons of DC by Tukey’s test (α=5%) followed the analysis.
Results
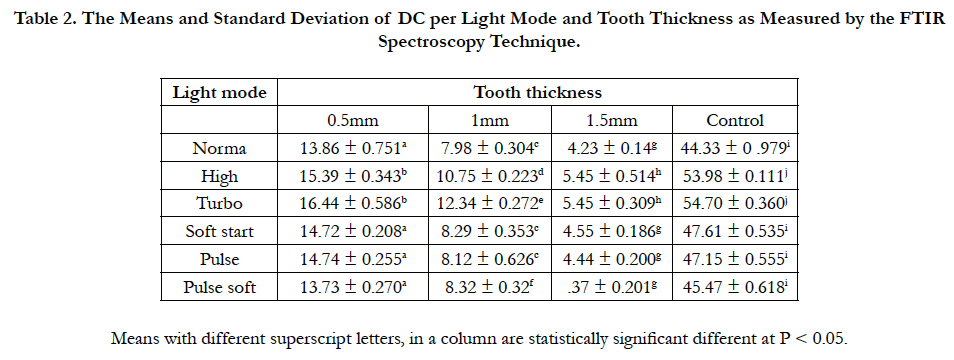
Our dependent variables DC were normally distributed as assessed by the Shapiro-Wilk tests. Statistically, the experimental (indirect curing group) showed significant difference when compared to control (direct curing) group (P < 0.05) (Table 2.).
Table 2. The Means and Standard Deviation of DC per Light Mode and Tooth Thickness as Measured by the FTIR Spectroscopy Technique.
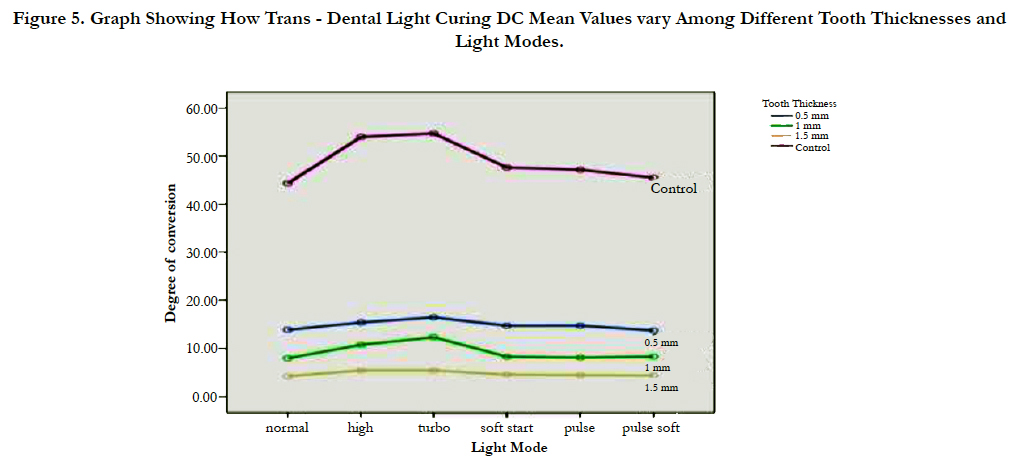
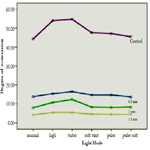
Regardless of the type of light-curing mode, DC mean values for all tooth slice groups were statistically significant different from each other (P < 0.05). It was also noted that DC mean values decreased with increasing tooth thickness with 0.5mm groups having the greatest DC values while thicker dentin groups showed the least values. DC could only be assessed to the maximum 1.5mm tooth thickness at which a 2mm layer of composite was assessed. Generally turbo light mode recorded the highest mean DC values than any other light mode while normal light presented lowest values. Statistical significant differences for the groups according to light curing modes are summarized in Table 2. Figure 5 Illustrates how trans-dental light curing DC mean values vary among different tooth thicknesses and light modes.
Figure 5. Graph Showing How Trans - Dental Light Curing DC Mean Values vary Among Different Tooth Thicknesses and Light Modes.
Discussion
So far scholars have tried a variety of methods in order to maximize the extent of polymerization of light-cured composite resins. There are many factors affecting degree of polymerization of light-cured resin composites. These factors include composite materials’ own internal composition; clinical situation related factors, such as procedural techniques and curing equipment performance related factors [36, 49, 50]. Due to the use of different types of equipments, materials and test conditions, there is no study homogeneity among most available literature. In previous experiments; ceramic materials, artificial light filters and other analogs were applied to indirectly cure composite resin using a transmitted light beam [44, 47], and then evaluated the effects on the depth of cure of composite resin. In this experiment freshly extracted human caries-free teeth were used to prepare dental slices of different thickness (Figure 1).
The experiments employed different thickness of tooth structure to irradiate light-cured composite resin. Seen in table 2 are mean DC values for the experimental and control groups. The average DC values for all experimental groups were lower than the control groups. For the experimental groups, 0.5mm group recorded the highest DC mean values, with every increase in tooth structure thickness, the DC decreased. FTIR spectroscopy is a common method used to determine degree of conversion [36, 49, 51]. Degree of conversion (DC) of methyl-acrylate bonds is the percentage to which carbon double bonds is converted to single carbon bonds to form cross-linked polymer chains [8, 37]. Conversion degree is an important parameter in the performance of composite resins. It’s apparent that as curing light travel through tooth tissue, its curing intensity is reduced by absorption and scattering of the light beam rendering lower conversion degree values. As expected, the thicker the tooth slices the less light intensity reaching the resin composite photo initiator, as a result, the formation of free radicals (which are responsible for the curing process) is reduced. Thus, 0.5mm groups had the highest conversion degree mean values while 1.5 mm recorded the lowest values. There were statistically significant differences of conversion degree mean values for the 0.5mm, 1mm and 1.5mm groups (P < 0.05).
Dental composite resin degree of double bond conversion ranges between 43% -75% [42, 52, 53]. According to our findings with more reliable FTIR spectroscopy analysis showed that there is substantial under polymerization for the indirect curing methods and none of the through-the-tooth curing met the optimum polymerization percentages which are in the range of 43-75%. Curing degree of visible light-cured resins depends on the intensity and quantity of light reaching the resin. Experimental groups with lower averages DC than the control groups may be related to the attenuation of light (by absorption and scattering effects), as the light beams transmit through the tooth structure to reach the composite resin. Arikawa et al., [44] who evaluated the lightattenuating effects of human enamel on the final properties of composite resins using artificial filters simulating dental tissues. They concluded that the light attenuating effects of the dental tissues reduced polymerization efficiency, resulting in poorer mechanical properties of light cured composite resins [44]. This finding is consistent with the observation of our experiment. The light intensity after transmittance through tooth tissue, depending on the thickness of the tooth tissue, may undergo different degree of scattering or absorption, resulting in minimized polymerization degree, thus reducing the DC. The least critical situation was recorded when 0.5 mm of composite Z100 was cured through 1mm enamel [47]. Although the experiments involved through tooth- tissue curing, only the quantitative analyses of hardness based measurements on the degree of polymerization were employed, no qualitative analyses were done.
The DC mean values for all groups differ according to different curing modes.
Purbo light mode recorded the highest DC values for all tooth thickness groups while Pulse soft and Normal light modes showed the lowest values. Turbo light showed statistically significant difference (P < 0.05) among the groups when compared to the normal, pulse, pulse soft and the soft start modes. High light also showed significant difference (P < 0.05) with the pulse soft mode. Generally there was no significant difference between pulse soft, soft start, normal and pulse modes, while turbo mode showed significant difference among the groups.
According to Sakaguchi and Berge [54]; polymerization process seems to be more dependent on the total energy available for photo-activation so any method that provides a higher amount of energy to the resin composite material would have a higher depth of cure and degree of conversion values [54].
Energy density (J/cm2 or mWs/cm2) is the product of the power intensity (mW/cm2) and irradiation time(s). Turbo light mode has its intensity rapidly rising to 1600mW/cm2. In 20 seconds the energy density is calculated to be approximately 32J/cm2, being the highest energy density of all the light modes employed in our study, it was expected to show the highest DC mean values as noted in our result findings. Similarly, the Normal and Pulse Soft modes which have the lowest energy densities 16J/cm2 and 18J/ cm2 respectively showed the lowest DC mean values. In a study done by Belvedere [29], it was found that the hardness of the indirect cured bulk-filled restorations was significantly less than the incrementally direct cured restorations. The findings are in consistency with our study where dental tissues are found to reduce dramatically the intensity of the light transmitted across it, rendering composite inadequate polymerization. The authors further suggested that when curing through tooth structure the energy density should be increased by a factor of 2-3 [29]. The current study concurs with the idea of increasing energy density for compensating lower polymerizations observed when curing light gets attenuated by a 0.5mm or greater tooth thickness. Based on this study's findings we suggest that composite resin curing process should avoid indirect irradiation. In the premise of attempting to save tooth structure during cavity preparation; should the need arise for indirect irradiation, the composite filling thickness should be less than 2mm, and the operator should consider ways to increase the energy density in order to improve the degree of polymerization.
This experiment utilized relatively reliable FTIR spectroscopy method of DC analysis, natural tooth slices for indirect irradiation, same composite resin material (shade A2) and standardized (curing distance and time) irradiation procedure to minimize possible study errors. However, it is worth acknowledging some limitations with this study: The tooth tissue sections used in the experiment were cut by a hand held instruments, thus rendering a certain degree of difficulty to obtain uniform thickness, each group used approximated value which may have introduced some errors. Temperature effect was not taken into account in our study due to difficulty in controlling temperatures led us into irradiating the tooth pieces and composite at significantly lower temperatures. Curing reaction being positively affected by higher temperatures would probably have recorded higher values in temperatures similar to those in the human oral cavity.
The current study findings do not warrant direct inference to clinical practice conclusions and guidelines due to differences between in vitro and in vivo environments. However, the experiment presents the general trend of trans-dental and curing modes on polymerization degree of composite resin that should be considered during clinical practices. In this respect, indirect light curing should be avoided as much as possible. An increase in the curing light energy density must be considered in order to improve the degree of polymerization in indirect irradiation. Hence, turbo light mode should be favored by clinicians over pulse soft and normal lights in trans-dental irradiation.
Conclusions
Nano-composite resins cured through different tooth thickness have lower DC compared to direct curing. The DC decreases with increasing intervening tooth thickness. The FTIR analysis mean DC values for the through-tooth-structure indirect curing were lower than the 45% -75% direct curing values. The DC mean values for turbo and high light modes were statistically higher compared to normal, soft start, pulse and pulse soft light modes.
References
- Marinho VC, Worthington HV, Walsh T, Clarkson J E (2013) Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 11(7): CD002279.
- Rosenstiel SF, Land MF, Crispin BJ (1998) Dental luting agents: A review of the current literature. J Prosthet Dent. 80(3): 280–301.
- Blank JT, Latta M (2005) Composite resin layering and placement techniques: Case presentation and scientific evaluation. Pract Proced Aesthet Dent. 17(6): 385-90.
- Feilzer AJ, Dooren LH, de Gee AJ, Davidson CL (1995) Influence of light intensity on polymerization shrinkage and integrity of restoration cavity interface. Eur J Oral Sci. 103(5): 322-326.
- Stanislawski L, Lefeuvre M, Bourd K, Soheili-Majd E, Goldberg M, et al., (2003) TEGDMA-induced toxicity in human fibroblasts is associated with early and drastic glutathione depletion with subsequent production of oxygen reactive species. J Biomed Mater Res A. 66(3): 476–82.
- Ferracane JL (2006) Hygroscopic and hydrolytic effects in dental polymer networks. Dent Mater. 22(3): 211–22.
- Jiménez-Planas A, Martín J, Ábalos C, Llamas R (2008) Developments in polymerization lamps. Quintessence Int. 38(2): e74-84.
- Krämer N, Lohbauer U, García-Godoy F, Frankenberger R (2008) Light curing of resin-based composites in the LED era. Am J Dent. 21(3): 135- 142.
- Robbins JW, Hilton TJ, Schwartz RS (2006) Fundamentals of operative dentistry: a contemporary approach. (3rd Edn), Quintessence Pub, UK.
- Hasler C, Zimmerli B, Lussi A (2006) Curing capability of halogen and LED light curing units in deep class II cavities in extracted human molars. Oper Dent. 31(3): 354-363.
- Ye Q, Wang Y, Williams K, Spencer P (2007) Characterization of photopolymerization of dentin adhesives as a function of light source and irradiance. Biomed Mater Res B Appl Biomater. 80(2): 440-446.
- Uhl A, Sigusch BW, Jandt KD (2004) Second generation LEDs for the polymerization of oral biomaterials. Dent Mater. 20(1): 80-7.
- Cavalcante LMA, Peris AR, Amaral CM, Ambrosano GMB, Pimenta LAF (2003) Influence of polymerization technique on microleakage and microhardness of resin composite restorations. Oper Dent. 28(2): 200-206.
- Amaral CM, de Castro AK, Pimenta LA, Ambrosano GM (2002) Influence of resin composite polymerization techniques on microleakage and microhardness. Quintessence Int. 33(9): 685-9.
- Soh MS, Yap AUJ, Siow KS (2004) Comparative depths of cure among various curing light types and methods. Oper Dent. 29(1): 9- 15.
- Hofmann N, Hugo B, Klaiber B (2002) Effect of irradiation type (LED or QTH) on photo-activated composite shrinkage strain kinetics, temperature rise, and hardness. Eur J Oral Sci. 110(6): 471-479.
- Ferracane JL, Mitchem JC, Condon JR, Todd R (1997) Wear and marginal breakdown of composites with various degrees of cure. Dent Res. 76(8): 1508-1516.
- Asmussen E, Peutzfeldt A (2001) Influence of pulse-delay curing on softening of polymer structures. Dent Res. 80(6): 1570-3.
- Rueggeberg FA, Caughman WF, Curtis Jr JW, Davis HC (1993) Factors affecting cure depths within light activated resin composites. Am J Dent. 6(2): 91-95.
- Ferracane JL, Greener EH (1986) The effect of resin formulation on the degree of conversion and mechanical properties of dental restorative resins. Biomed Mater Res. 20(1): 121-31.
- Asmussen E (1975) NMR–analysis of monomers in restorative resins. Acta Odontol Scand. 33(3): 129-34.
- Pfeifer CS, Braga RR, Ferracane JL (2006) Pulse-delay curing: influence of initial irradiance and delay time on shrinkage stress and microhardness of restorative composites. Oper Dent. 31(5): 610-615.
- Rueggeberg F (1999) Contemporary issues in photocuring. Compend Cont Edu Dent. 25: S4-S15.
- Feilzer AJ, De Gee AJ, Davidson CL (1998) Curing contraction of composites and glass ionomer cements. Prosthet Dent. 59(3): 297-300.
- Perdigao J, Lopes M (1999) Dentin bonding - State of the Art 1999. Comp Cont Edu Dent. 20(12): 1151-1162.
- Lösche G (1999) Marginal adaptation of class II composite fillings: guided polymerizationn vs reduced light intensity. Adh Dent. 1(1): 31-39.
- Lutz F, Krejci I, Oldenberg TR (1986) Elimination of polymerization stressess at the margins of posterior composite resin restorations: a new restorative technique. Quintessence Int. 17(12): 777-784.
- Sideridou ID, Achilias DS (2001) Elution study of unreacted Bis-GMA, TEGDMA, UDMA, and Bis-EMA from light cured dental resins and resin composites using HPLC.
- Belvedere PC (2001) Contemporary posterior direct composites using stateof- the-art techniques. Dent Clin North Am. 45(1): 49-70.
- Shortall AC, Wilson HJ, Harrington E (1995) Depth of cure of radiationactivated composite restoratives- Influence of shade and opacity. Oral Rehab. 22(5): 337–342.
- Muarry GA, YatesJ L, Newman SM (1981) Ultraviolet light and ultarviolet light - activated composite resins. Prosthet Dent. 46(2): 167-170.
- Newman SM, Murray GA (1983) Visible lights and visible light activated composite resins. Prosthet Dent. 50(1): 31-35.
- Yap AU, Soh MS, Siow KS (2002) Effectiveness of composite cure with pulse activation and soft-start polymerization. Oper Dent. 27(1): 44-49.
- Standard I (2000) ISO 4049 Polymer based filling, restorative and luting materials. (3rd edn), 1-27.
- De Wald JP, Ferracane JL (1987) A comparison of four modes of evaluating depth of cure of light-activated composites. Dent Res. 66(3): 727-730.
- Aravamudhan K, Rakowski D, Fan PL (2006) Variation of depth of cure and intensity with distance using LED curing lights. Dent Mater. 22(11): 988-994.
- Beun S, Glorieux T, Devaux J, Vreven J, Leloup G (2007) Characterization of nanofilled compared to universal and microfilled composites. Dent Mater. 23(1): 51–9.
- Ferracane JL, Greener EH (1984) Fourier transform infrared analysis of degree of polymerization in unfilled resins--methods comparison. Dent Res. 63(8): 1093-5.
- Halvorson RH, Erickson RL, Davidson CL (2003) The effect of filler and silane content on conversion of resin-based composite. Dent Mater. 19(19): 327-33.
- Atmadja G, Bryant RW (1990) Some factors influencing the depth of cure of visible light-activated composite resins. Aust Dent. 35(3): 213-218.
- Owens BM, Rodriguez KH (2007) Radiometric and spectrophotometric analysis of third generation light-emitting diode (LED) light-curing units. J Contemp Dent Pract. 8(2): 43-51.
- Moraes LGP, Rocha RSF, Menegazzo LM, Araujo EB, Yukimitu K, et al., (2008) Infrared Spectroscopy: A tool for determination of the degree of conversion in dental composites. Appl Oral Sci. 16(2): 145-9.
- Peutzfeldt A, Asmussen E (1996) In vitro wear, hardness and conversion of diacetylcontaining and propanal-containing resin materials. Dent Mater. 12(2): 103-8.
- Arikawa H, Kanie T, Fujii K, Shinohara N (2004) Bending strength and depth of cure of light-cured composite resins irradiated using filters that simulate enamel. J Oral Rehabil. 31(1): 74–80.
- Standlee JP, Caputo AA, Hokama SN (1988) Light cured composites. CDA j. 16(3): 25-28.
- Weaver WS, Blank LW, Pelleu GB (1987) A visible light-activated resin cured through tooth structure. Gen Dent. 36(3): 136-713.
- D Dietschi, N Marret, I Krejci (2003) Comparative efficiency of plasma and halogen light sources on composite micro-hardness in different curing conditions. Dent Mater. 19(6): 493–500.
- Obici AC, Sinhoreti MAC, Frollini E, Correr Sobrinho L, Consani S (2004) Degree of conversion of Z250 composite determined by fourier transform infrared spectroscopy: comparison of techniques, storage periods and photo-activation methods. Mater Res. 7(4): 605-610.
- da Silva EM, Poskus LT, Guimarães JG, de Araújo Lima Barcellos A, Fellows CE (2008) Influence of light polymerization modes on degree of conversion and crosslink density of dental composites. J Mater Sci Mater Med. 19(3):1027–32.
- Davidson CL, de Gee AJ (2000) Light-curing units, polymerization, and clinical implications. J Adhesive Dent. 2(3): 167-173.
- Stansbury JW, Dickens SH (2001) Determination of double bond conversion in dental resins by near infrared spectroscopy. Dent Mater. 17(1): 71–79.
- Yap AU, Wang HB, Siow KS, Gan LM (2000) Polymerization shrinkage of visible light-cured composites. Oper Dent. 25(2): 98-103.
- Tezvergil-Mutluay A, Lassila LV, Vallittu PK (2007) Degree of conversion of dual-cure luting resins light-polymerized through various materials. Acta Odontol Scand. 65(4): 201-205.
- Sakaguchi RL, Berge HX (1998) Reduced light energy density decreases post-gel contraction while maintaining degree of conversion in composites. Dent. 26(8): 695-700.