Relationship between Periodontal Disease and Diabetes: A Survey among Internal Medicine Residents in Saudi Arabia
AlAhmari F*
Lecturer/Department of Periodontics and Community Dentistry/ King Saud, University Riyadh, Saudi Arabia.
*Corresponding Author
Fatemah AlAhmari,
Lecturer, Department of Periodontics and Community Dentistry,
King Saud, University Riyadh, Saudi Arabia.
Tel: +966551234955
E-mail: falahmari@ksu.edu.sa
Received: January 28, 2018; Accepted: February 10, 2018; Published: February 13, 2018
Citation:AlAhmari F. Relationship between Periodontal Disease and Diabetes: A Survey among Internal Medicine Residents in Saudi Arabia. Int J Dentistry Oral Sci. 2018;5(2):589-594. doi: dx.doi.org/10.19070/2377-8075-180000115
Copyright: AlAhmari F©2018. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Numerous epidemiological studies provide consistent evidence of greater prevalence and severity of periodontal disease (PD) among diabetes. Health care providers should have the knowledge of the bi-directional relationship between diabetes and PD and discuss it with their diabetic patients. The present study investigates the knowledge and awareness of the relationship between PD and diabetes among internal medicine residents in Saudi Arabia.
Methods: The questionnaire was distributed to 200 Saudi internal medicine residents from various institutions and hospitals in Saudi Arabia. It had 4 true/false knowledge items and 7 Likert-scale questions. Questions aimed to assess the knowledge levels of the subjects about PD and their attitudes toward discussing and evaluating the periodontal status of their patient.
Results: Out of 200 residents queried, 131 responded (response rate: 65.5%). The Age was ≥24 years, majority of the respondents were male (64.1%) and senior intern medical residents (75.6%). 72% of the residents correctly answered all 4 true/false knowledge questions. 100% reported no prior training received about PD in medical school. Majority (64.1%) felt discussing about periodontal status to their patients was peripheral and 58% reported feeling very uncomfortable performing simple periodontal examination. 51.9% reported never screened patients for periodontal disease and rarely referred their patients to dentists. 18.3% agreed that patients expect physicians to discuss about periodontal disease.
Conclusions: The study demonstrated that Saudi internal medicine residents had meager knowledge and awareness of PD and its association with diabetes. They were also uncomfortable with performing a simple periodontal examination. Oral health education is recommended as part of medical school curriculum.
2.Introduction
3.Case Report
4.Discussion
5.Conclusion
6.Acknowledgments
7.References
Keywords
Periodontitis; Diabetes; Oral Hygiene; Awareness; Internal Medicine Residents.
Introduction
Periodontitis is defined as an inflammatory disease of supporting tissues of teeth in response to dental plaque. Various forms of periodontitis with differing clinical manifestations, responses to treatment result from differences in the microbial etiology among individuals and/or factors that modify host response mechanisms [1]. Of many risk factors associated with the development of periodontal disease (PD), diabetes has long been confirmed as a major risk factor, increasing the chances of its occurrence threefold among type I and II diabetic patients [2, 3]. PD has been reported as the sixth complication of diabetes, along with neuropathy, nephropathy, retinopathy, and micro-and macrovascular diseases [4].
The International Diabetes Federation (IDF) [5] report estimated around 425 million diabetes in the world, where with more than 39 million people alone in the North Africa MENA and the Middle East region. Saudi Arabia ranks the second highest in the Middle East and seventh in the world for the rate of diabetes with 3,852, 000 cases in 2017 [6]. The most worrying is the increasing pattern of diabetes noted in the recent past [7]. Numerous epidemiological studies provide consistent evidence of greater prevalence and severity of PD among type I and II diabetes [8]. Several studies emphasized the importance of high glycemic control as a risk factor for attachment loss [2, 9, 10] and importance of the periodontal therapy to ameliorate metabolic control of diabetes [11-13].
Health care providers should have the knowledge and awareness of the bi-directional relationship between diabetes and PD and discuss it with their diabetic patients. According to a survey conducted by Bahammam [14], it was reported that majority of the respondents (94.8%) of the total 454 adults diabetic population in Saudi Arabia have never received advice on oral hygiene in relation to diabetes from their health professional. Despite systematic evidences available to acknowledge the relationship between both, medical practitioners fail to recognize the importance of periodontal examination as a preliminary screening for diabetes [15-17]. In support of this view, a recent study by Asa′ad et al. [18] had evaluated the knowledge and orientation of medical interns towards PD but not on its relationship to diabetes. The present study aimed to investigate the knowledge and awareness of the relationship between periodontitis and diabetes among internal medicine residents in Saudi Arabia.
Materials and Methods
This study was a cross sectional and descriptive survey conducted among two hundred Saudi internal medicine residents from September to November 2017. The participants were randomly chosen from various universities and hospitals located in different cities in Saudi Arabia. To evaluate the knowledge, attitude and clinical behavior about periodontal disease and its association with diabetes, a structured closed-ended questionnaire was developed based on in-depth literature reviews andreferring to the specific study by Quijano et al. [19, 20]. Questionnaire included four true/false knowledge items and seven Likert-scale questions. Demographic information such as age and sex were obtained from each participant. The questionnaire was pilot tested among 10% of the total sample to assess the logical flow, time consumption and readability. Based on the feedback, the questionnaire was restructured especially terminology corrections were carried out. The internal medicine residents email addresses were collected through the websites of various universities and hospitals in different cities in Saudi Arabia. The main questionnaire along with a cover letter highlighting the objective of the study and participation confidentiality was sent via email obtained from their institution websites. It was emphasized that answering the questionnaire was optional and each participant was briefed on estimated time to complete the questionnaire as ~10 minutes. Out of total 200 questionnaires sent and after three email follow-ups, only 131 responded the survey with a response rate of 60.5%.
The final data were processed and coded for further analysis. The collected data were imported and analyzed using the Statistical Package for Social Sciences version 21 (IBM SPSS Statistics, Version 21.0. Armonk, NY; IBM Corp). Descriptive Statistics such as frequency and percentage analysis was conducted and data were presented in the form of mean and standard deviation (SD). Independent sample t test and One-way Analysis of Variance (ANOVA) were conducted to compare the mean knowledge, clinical and attitude scores between gender, age group and designation. The significance level was set at p<0.05.
Results
Out of 200 internal medicine residents, 131 responded included for the final analyses. Of the 131 respondents, 64.1% were male, while 35.9% belongs to female. The questionnaire was administered to the residents aged greater than equal to ≥24 years. Majority of the respondents were senior residents (75.6%).
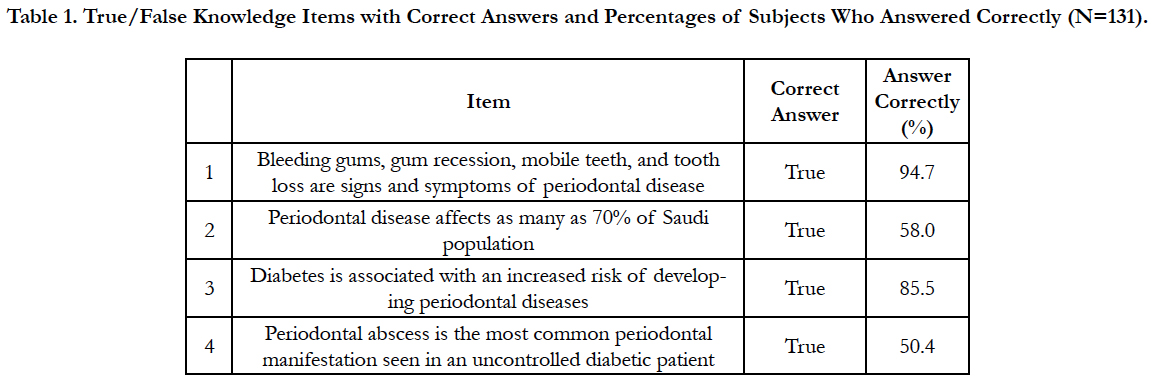
From Table 1, we infer that about 72% of the residents correctly answered all four true/false general knowledge questions which ranged from 50.4% to 94.7%. Although most residents demonstrated knowledge regarding the signs of periodontal disease and its association with diabetes, nearly half did not know about periodontal abscess is the most common periodontal manifestation seen in an uncontrolled diabetic patient.
Table 1. True/False Knowledge Items with Correct Answers and Percentages of Subjects Who Answered Correctly (N=131).
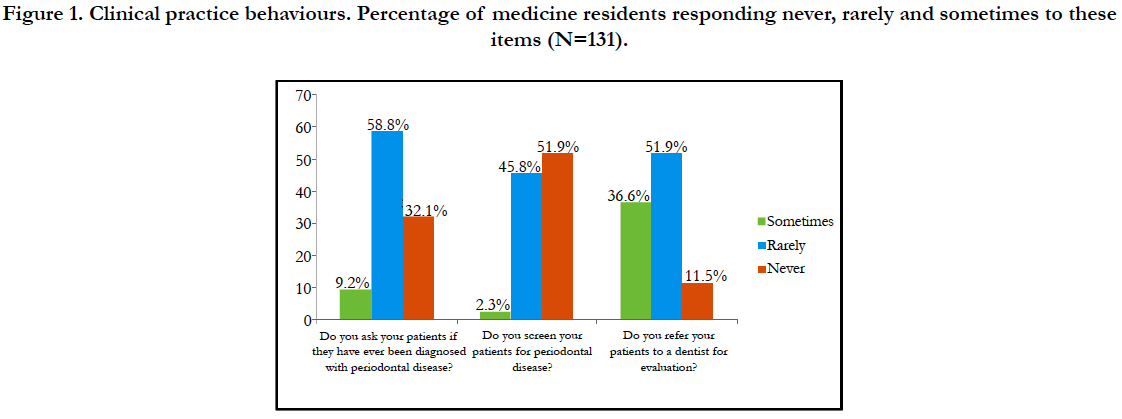
Figure 1 shows half of the respondents (51.9%) reported that they rarely referred their patients to dentists for oral evaluation and the same percentage of respondents reported that they never screened their patients for periodontal disease. Moreover, the majority (58.8%) of the respondents reported that they rarely asked their patients if they have ever been diagnosed with periodontal disease.
Figure 1. Clinical practice behaviours. Percentage of medicine residents responding never, rarely and sometimes to these items (N=131).
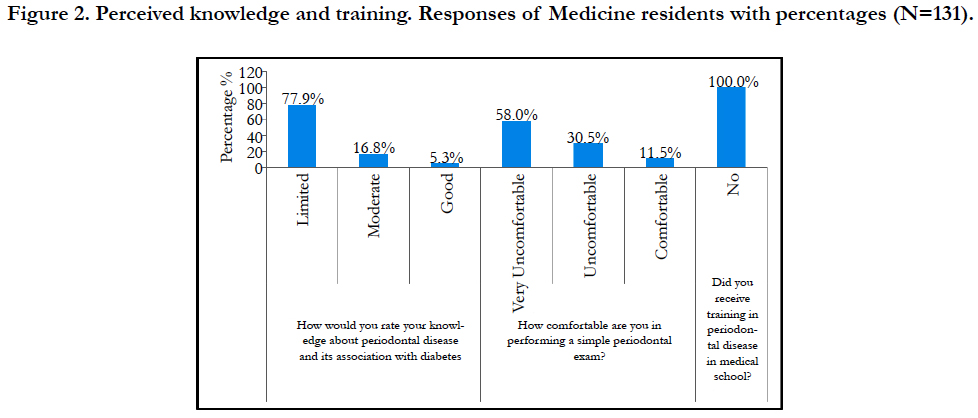
From Figure 2 we infer that 100% of the respondents have not received any training about the periodontal disease at the medical school level. Majority of the respondents (58%) reported that they feel very uncomfortable performing a simple periodontal examination and only 5.3% of the total 131 respondents reported good knowledge about the periodontal disease and its association with diabetes.
Figure 2. Perceived knowledge and training. Responses of Medicine residents with percentages (N=131).
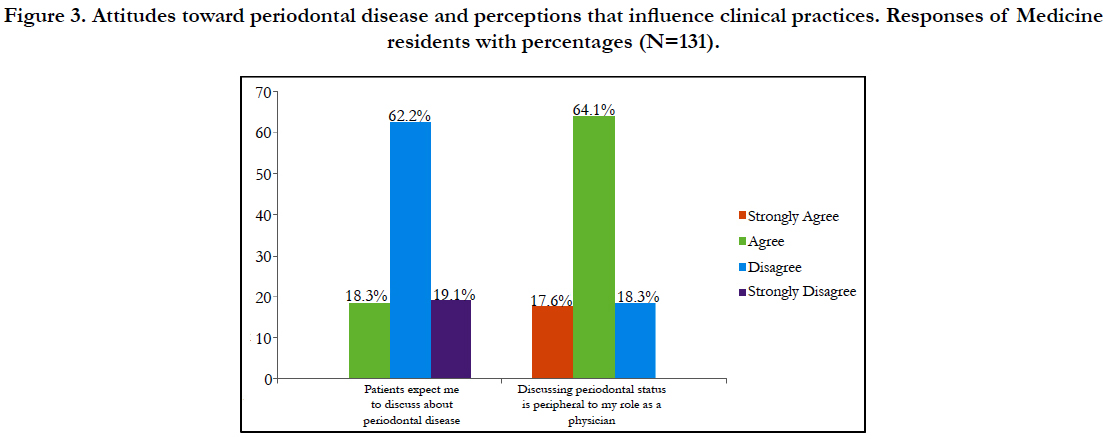
About 64.1% agreed to the statement that they felt discussing or evaluating the periodontal status of their patients was peripheral to their role as physicians but only 18.3% agreed that their patients expect them to discuss the periodontal disease. There was a significant association between patient’s expectation and doctor’s view on periodontal disease discussion (p<0.001) (Figure 3).
Figure 3. Attitudes toward periodontal disease and perceptions that influence clinical practices. Responses of Medicine residents with percentages (N=131).
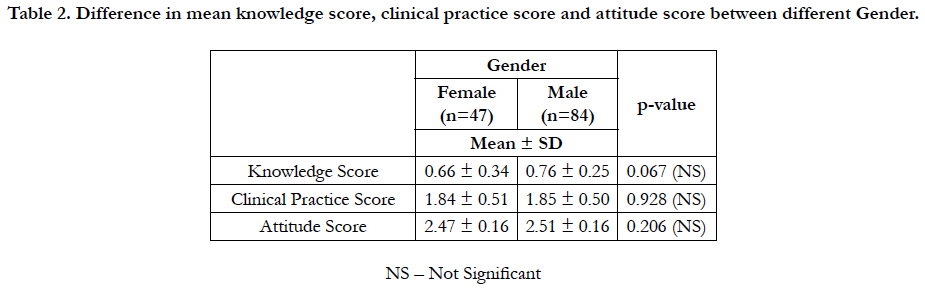
As shown in Table 2, there was no significant difference in overall mean knowledge score (p=0.067), clinical practice score (p=0.928), and attitude score (p=0.206) between male and female internal medical residents irrespective of their seniority.
Table 2. Difference in mean knowledge score, clinical practice score and attitude score between different Gender.
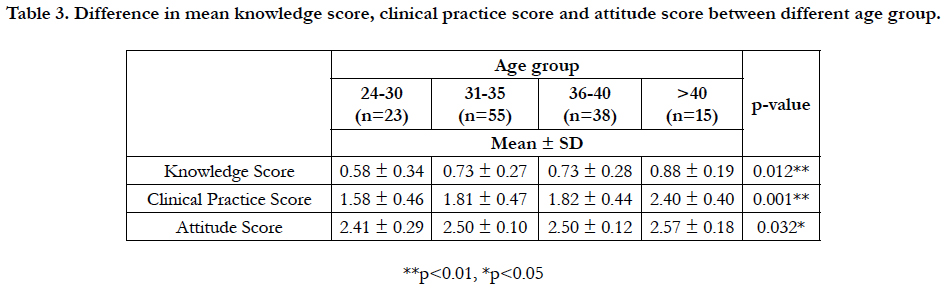
From Table 3, there was a significant difference in knowledge (p=0.012), clinical practice (p=0.001) and attitude score (p=0.032) among different age groups. In knowledge, clinical practice and attitude score for age group ≥40 years were predominances with 0.88 ± 0.19, 2.40 ± 0.40 and 2.57 ± 0.18 respectively when compared to other age groups.
Table 3. Difference in mean knowledge score, clinical practice score and attitude score between different age group.
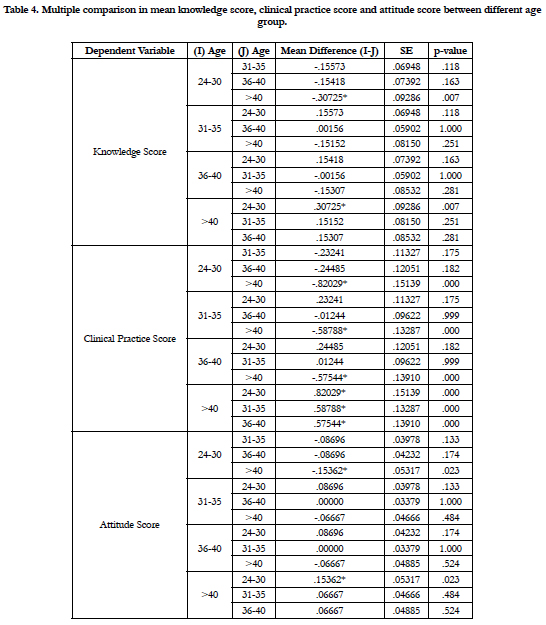
Table 4 provides the multiple comparisons of mean knowledge, clinical practice and attitude score within age groups of internal medicine residents in Saudi Arabia. In knowledge score, there was significant difference was observed between 24-30 and > 40 years Mean Difference (M.D = -0.30725, p=0.007). Similarly, in clinical practice score, there was significant difference was observed between 24-30 and > 40 years (M.D = -0.82029, p<0.001), 31-35 and >40 years (MD= -0.58788, p<0.001) and 36-40 and >40 years (M. D= -0.57544, p<0.001). In attitude score there was significant difference observed between 24-30 and > 40 years (M.D = -0.15362, p=0.023).
Table 4. Multiple comparison in mean knowledge score, clinical practice score and attitude score between different age group.
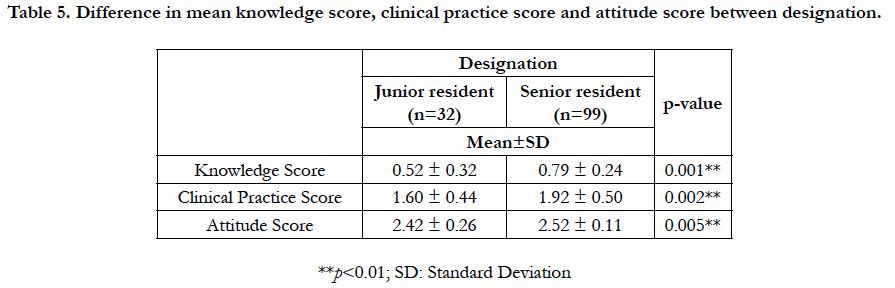
Table 5 shows clear that senior residents were better in terms of knowledge score (p=0.001), clinical practice (p=0.002) and attitude score (p=0.005) when compared to the junior resident. The overall mean knowledge score (0.79 ± 0.24), clinical practice (1.92 ± 0.50) and attitude score (2.52 ± 0.11) was high in senior residents when compared to junior residents.
Table 5. Difference in mean knowledge score, clinical practice score and attitude score between designation.
Discussion
Several recent studies have acknowledged the link between periodontal disease and diabetes [2, 9, 20] and proper understanding of its association is vital for effective diagnosis, evaluation, treatment and management of both disease conditions. As primary medical practitioners are the first to the point of contact for diabetic patients presenting withoral or dental disease, it is essential to educate general medical practitioners on the significance of oral hygiene to ameliorate chronic systemic illnesses such as diabetes [15, 21, 22]. Hence, the present study aims to assess the knowledge of internal medicine residents on periodontal disease and its relationship with diabetes in Saudi Arabia.
Our study includes randomly chosen mixed internal medicine residents of different age groups, gender and seniority. About 72% of the residents correctly answered all four true/false general knowledge questions and this percentage was less than Asa’adet al (81.9%) [18]. This difference may be due to the sample size and their responses. In our study majority of the respondents (94.7%) correctly answered a question which assesses their knowledge ofsigns and symptoms of periodontal disease. This was comparable to similar studies with similar question set up [21,23]. However, when questioned about its manifestation in diabetic patient only half of the respondents answered it correctly.
In our study, only 5.3% of the internal medicine residents stated that they are aware of the relationship between periodontal disease and diabetes. Yet, this percent was low in comparison to similar studies which had a minimum of 13.8% [24] to a maximum of 66.8% [25]. It is difficult to interpret this outcome as each due to the methodological variations as each study have stratified answers based on their respondent’s level of knowledge. However, lower knowledge rates about the association between PD and diabetes may be due to heterogenic distribution (junior and senior residents) of respondents in our study. It was surprising to note that 100% of our respondents have reported that they have not received any training about PD at the medical school level and these findings are in contradictory to the findings of Asa′ad et al. [18]. It may be evident that medical schools in Saudi Arabia do not emphasize the importance of periodontal-systematic disease connection into the didactic and clinical aspects of the curriculum. Majority of the respondents (58%) reported that they feel uncomfortable performing a simple periodontal examination which was more when compared to the findings ofAsa′ad et al. [18]. It was observed from similar studies, that medical practitioners are less interested in educating their patients on periodontal disease and its association with diabetes [14]. In our study, 11.5% residents stated that they never referred their patients to dentists for oral evaluation. When compared to previous studies which investigated the referral rate by medical practitioners, 56.5% [25], 57.5% [18], 58.5% [23], the present study has comparable findings of 51.9%. However, studies by Nagarakanti et al. [21] and Umeizudike et al. [24] showed maximum referral rate of 86.1% and 90.9% respectively of which the former study reported that only 10.1% of respondents referred to thedentist without patient asking for the same. The majority (58.8%) of the respondents reported that they rarely asked their patients if they have ever been diagnosed with PD which was comparable to findings of Asa′ad et al. [18] (49.8%).
Our study reported no significant difference in overall mean knowledge score, clinical practice score and attitude score between male and female internal medical residents irrespective of their seniority. However, there was a significant difference in knowledge, clinical practice and attitude score among different age groups and seniority. This could be due to awareness through medical journals, institutional training, a number of years in clinical practices, attending conferences/symposiums etc. where current issues are debated [24, 25].
Our findings suggest the need to collaborate dental and general medical practitioners to improve patients’ outcome in terms of both chronic disease conditions. It is important not to overlook the presentation of severe periodontitis among diabetic patients as it might compromise their systemic immunity. It is important to refer these patients to dental practitioners for better management of dental disease and diabetes. Our findings also suggest interdisciplinary training to solve the problem. Therefore, a better curriculum at medical school level is essential and has to be mandated. One of the main limitations of this study is the use of a self-reported questionnaire that in turn might be biased in answering questions. Nevertheless, this limitation was attempted to minimize through options given to the residents. Although the study applied random sampling method to ensure the representative of residents across Saudi hospitals/practice and universitybased clinic settings, the study did not specifically analyze the knowledge and attitude in a variety of locations and practices which in turn would enable to understand the level of intervention required. The results presented indicate the opinions of small sample of medical interns in Saudi Arabia. This study does not enable broad generalizations regarding the potential impact of these findings. Caution must be taken in interpreting the applicability of the current data until these findings can be confirmed by larger, prospective investigations.
Conclusion
The study demonstrated that Saudi internal medicine residents had meager knowledge and awareness of PD and its association with diabetes. This could be due to no prior training or awareness courses instructed at the medical school level. Besides, experienced internal medical interns had better knowledge of PD and relations to diabetes than those from lower levels. Given that, Saudi ranks highest among diabetes prevalence and majority of diabetic population visits primary health professionals for their treatment, it is important to include oral health as a part of medical curriculum, so the patients can be well diagnosed/evaluated and made aware of oral hygiene and its significance in ameliorating metabolic control of diabetes.
References
- Page RC, Offenbacher S, Schroeder HE, Seymour GJ, Kornman KS. Advances in the pathogenesis of periodontitis: summary of developments, clinical implications and future directions. Periodontol 2000. 1997 Jun 1;14(1):216-48.
- Preshaw PM, Alba AL, Herrera D, et al. Periodontitis and diabetes: a twoway relationship. Diabetologia. 2012 Jan 1;55(1):21-31.
- Chang PC, Lim LP. Interrelationships of periodontitis and diabetes: A review of the current literature. J Dent Sci. 2012 Sep 1;7(3):272-82.
- Löe H. Periodontal disease. The sixth complication of diabetes mellitus. Diabetes Care. 1993 Jan 1;16(1):329-34.
- International Diabetes Federation (2018) Across the Globe. In: IDF Diabetes Atlas.
- International Diabetic Federation (2018) IDF MENA Members.
- Al Dawish MA, Robert AA, Braham R, et al. Diabetes Mellitus in Saudi Arabia: A Review of the Recent Literature. Curr Diabetes Rev. 2016 Dec 1;12(4):359-68. PubMed PMID: 26206092.
- Kim J, Amar S. Periodontal disease and systemic conditions: a bidirectional relationship. Odontology. 2006 Sep;94(1):10-21. PubMed PMID: 16998613.
- Southerland JH, Taylor GW, Offenbacher S. Diabetes and Periodontal Infection: Making the Connection. Clin Diabetes. 2005 Oct 1;23(4):171-8.
- Mealey BL, Oates TW. Diabetes Mellitus and Periodontal Diseases. J Periodontol. 2006 Aug;77(8):1289-303.
- Vergnes JN. Treating periodontal disease may improve metabolic control in diabetics. Evid Based Dent. 2010 Sep;11(3):73. PubMed PMID: 20938470.
- Wang TF, Jen IA, Chou C, Lei Y-P. Effects of Periodontal Therapy on Metabolic Control in Patients With Type 2 Diabetes Mellitus and Periodontal Disease. Medicine (Baltimore). 2014 Dec;93(28):e292. PubMed PMID: 25526470.
- Murgod S, Reddy SS, Kripal K, et al. Effect of Periodontal Intervention on Metabolic Control of Diabetes Mellitus. EC Dental Science 1.S2: S29-S37.
- Bahammam M. Periodontal health and diabetes awareness among Saudi diabetes patients. Patient Prefer Adherence. 2015 Feb 2;9:225-33. doi: 10.2147/PPA.S79543. eCollection 2015. PubMed PMID: 25673974.
- Elangovan S, Hertzman-Miller R, Karimbux N, Giddon D. A Framework for Physician-Dentist Collaboration in Diabetes and Periodontitis. Clin Diabetes. 2014 Oct;32(4):188-92. PubMed PMID: 25646947.
- Pumerantz AS, Bissett SM, Dong F, et al. Standardized screening for periodontitis as an integral part of multidisciplinary management of adults with type 2 diabetes: an observational cross-sectional study of cohorts in the USA and UK. BMJ Open Diabetes Res Care. 2017 Jul 1;5(1):e000413.
- Shetty N, Shankarapillai R, Mathur L, et al. Gingival crevicular blood: As a non-invasive screening tool for diabetes mellitus in dental clinics. J Indian Soc Periodontol. 2013 Jul;17(4):472-7. PubMed PMID: 24174727.
- Asa′ad F, Asaad L, Al-Maflehi N, et al. Knowledge and orientations of medical interns toward periodontal disease in Saudi Arabia. Saudi J Oral Sci. 2014 Jul 1;1(2):98.
- Quijano A, Shah AJ, Schwarcz AI, et al. Knowledge and Orientations of Internal Medicine Trainees Toward Periodontal Disease. J Periodontol. 2010 Mar;81(3):359-63. PubMed PMID: 24174727.
- Dina CA, Iancau M, Moţa M, et al. The relationship between periodontal disease and diabetes mellitus. Rom J Diabetes. 2012 Jun 1;19(2):181-8.
- Nagarakanti S, Epari V, Athuluru D. Knowledge, attitude, and practice of medical doctors towards periodontal disease. J Indian Soc Periodontol. 2013 Jan;17(1):137-9. PubMed PMID: 23633790.
- Mehrotra V, Garg K, Sharma P, et al. A Study Based on Dental Awareness, Knowledge and Attitudes among the Medical Practitioners in and Around Kanpur City (India). J Interdiscip Med Dent Sci. 2015;3(183):2.
- Anandakumar A, Sankari R. Awareness about Periodontal Disease and its Association with Systemic Disease among Medical Practitioners: A Pilot Study. J Contemp Dent. 6(2):104–107.
- Umeizudike KA, Iwuala SO, Ozoh OB, et al. Association between periodontal diseases and systemic illnesses: A survey among internal medicine residents in Nigeria. Saudi Dent J. 2016 Jan;28(1):24-30. PubMed PMID: 26792966.
- Tasdemir Z, Alkan BA. Knowledge of medical doctors in Turkey about the relationship between periodontal disease and systemic health. Braz Oral Res. 2015;29:55. PubMed PMID: 25885023.