Annulare Centrifugal Erythema Erupted by P. Mirabilis Infection , that Mimics an Allergic Drug Reaction
Hoxha M, Kryeziu EZ*
Service of Allergology and Clinical Immunology, University Hospital Center "Mother Theresa" Tirana, Albania.
*Corresponding Author
Enkeleida Zekthi Kryeziu,
Service of Allergology and Clinical Immunology,
University Hospital Center "Mother Theresa" Tirana, Albania.
Email: enkeleida_zekthi@yahoo.com
Recieved: July 06, 2017; Accepted: November 10, 2017; Published: November 13, 2017
Citation: Hoxha M, Kryeziu EZ. Annulare Centrifugal Erythema Erupted by P. Mirabilis Infection , that Mimics an Allergic Drug Reaction. Int J Microbiol Adv Immunol. 2017;05(2):82-85. doi: http://dx.doi.org/10.19070/2329-9967-1700016
Copyright: Kryeziu EZ© 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
The classification of annular centrifugal erythemas can be confusing and has always been one of the most discussed issues in medicine. We report a case of 58 years old woman who had a 3 –days post vaginal-plastic surgery. The patient presented non- pruritic annular skin eruptions on the abdomen and extremities, spreading gradually and forming large rings. She was treated during this period at the gynecologist department and later was admitted to a tertiary care hospital with the diagnosis "enoxaparin-sodium drug" reaction. The skin lesion was not associated with the drug allergy reaction. Urino–culture grew Proteus Mirabilis, Vulgaris. Presence of Proteus mirabilis and annular centrifugal erythema eruption lesions, suggests a pathogenetic effect of the gram-negative bacterium on the skin lesion. Considering the anamnesis and the clinical manifestation, the patient was treated with antibiotic therapy, corticosteroid therapy, anti-histaminic and local corticosteroid cream. To our knowledge, no other case of EAC associated with Proteus mirabilis infection has been published.
2.Introduction
3.Patient History
4.Conclusion
5.References
Keywords
Erythema Annulare Centrifugum; Proteus Mirabilis; Enoxaparin - Sodium.
Introduction
Erythema annular centrifugum (EAC) is an inflammatory dermatosis with typical clinical and histological demonstrations. It can affect either sex and can occur at any age, including neonates. [2].
Typical presentations are erythematous annular lesions with peripheral enlargement and central demolition. Based on clinical and histological data, it is usually classified as superficial, deep infiltrated lymphohistiocytic and normal epidermis [10].
The etiology is unclear but is assumed an association with infection, medication, malignancy, and stress [2, 3, 11].
Rare associations include autoimmune disorders such as Graves disease, Hypereosinophilic syndrome and progesterone dermatitis [5, 13].
The pathogenesis of the EAC is not clearly understood while bacterial, fungal and viral antigens, drugs, neoplasm, and autoimmune diseases have been described as possible causative factors [18]. In this article, we report the case of adult women who presented EAC associated with urinary tract infection (UTIs) from Proteus Mirabilis, Vulgaris.
Patient History
A 58 years old woman were referred to the Allergy and Clinical Immunology Department with the diagnosis "enoxaparin-sodium drug reaction" with abdominal discomfort, fatigue, a light pruritis, strong and frequent urge to urinate, strong smelling urine, muscle aches and abdominal pains. In the first day, five hours later that the patient had the enoxi-parin sodium sub cutaneous injection, the patient had non-pruritic annular skin eruptions on the abdomen and both two legs, spreading gradually forming large rings and mild central hyperpigmentation (Figure 1).
She was treated during this period by the gynecologist department for pelvic prolapse (anteroposterior vaginoplasty). The skin eruption appeared 5 (five) hours later after she had the first subcutaneous enoxaparin injection as post-intervention anticoagulant therapy ((Enoxaparin sodium (Lovenox) Injection is an anticoagulant (blood thinner) used to prevent blood clots). There was no earlier history of drug allergy, no other family history of skin, connective tissue, or autoimmune disease.
The patient skin eruption mimics an EAC, for these reasons a full packet of the examination was conducted to exclude all hidden disorders.
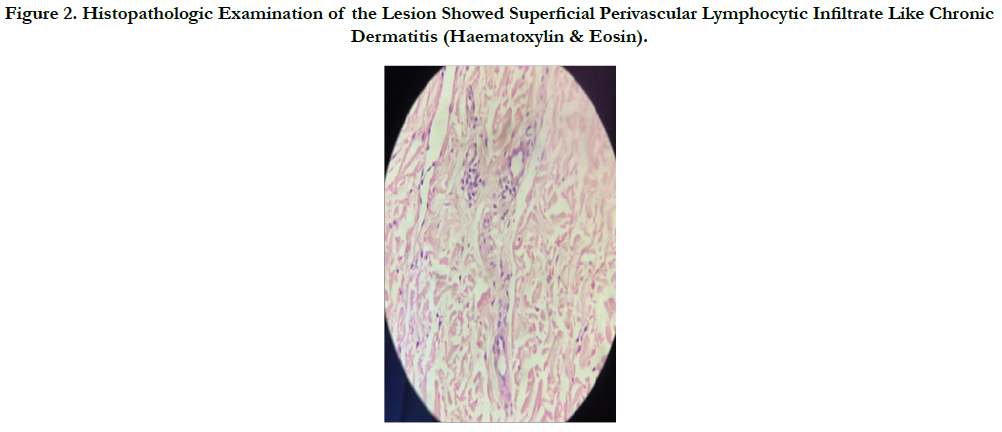
Laboratory tests showed that serum aminotransferases (ALT, 12 IU/L; AST, 21 IU/L), bilirubin levels (total, 0.8 mg/dl; direct, 1mg/ dl) and alkaline phosphatase (ALP, 82 IU/L) were normal. Serum prothrombin time was 348mg/dl, tryglicerid 55mg/dl, cholesterol 206mg./dl. Her complete blood count revealed a hemoglobin of 10.7g/dL, a hematocrit level of 29.2%, a white blood cell count of 7.4×103/mcL, with 87.5 % neutrophils, 4% bands, 2.8% monocytes, and 9.7% lymphocytes. Thyroid ultrasound revealed the normal structure and homogeneous echotexture, normal isthmus. Abdominal ultrasound revealed normal liver size with normal echotexture with no evidence of portal hypertension, normal spleen, kidneys, and retroperitoneum. Serum ferritin, ceruloplasmin levels were normal. Immunoserology markers, antinuclear antibodies (ANA) was positive (+++) C3 114 mg/dl, C4 24.9 mg/dl, ASO 25 IU/ml. PCR 67.8 mg/L (very high). Protein electrophoresis, albumin 57.6%, α1 globulin 3.6 %, α2 globulin 15.8% β globulin 12.4%, μ globulin 10.6 %, Anti borrelia IgG 6.2 U/ml, anti Borrelia IgM 2.2 (normal). Anti - dsDNA Screen 4.1 U/ml, Anti TPO 40.6 U/ml, FT 4 1.42mg/dl. Negative code and eosinophil sputum culture, urine culture grew Proteus Mirabilis 100.000 bacterium [CFUs]/mL), vaginal culture test were normal. CT scanning of the head is normal, CT pulmonary angiogram was normal, Abdominal and pelvic CT recent hysterectomy. Skin biopsy revealed with a light superficial perivascular lymphocytic infiltrate like chronic dermatitis (superficial variant) (Figure 2).
Figure 1. Erythema Annular Centrifuge. Spreading Gradually to Form Large Rings a Mild Central Hyperpigmentation.
Figure 2. Histopathologic Examination of the Lesion Showed Superficial Perivascular Lymphocytic Infiltrate Like Chronic Dermatitis (Haematoxylin & Eosin).
After five weeks our patient reported that the lesions began to appear every day and regressed spontaneously. The skin eruption has the same clinical characteristics of the first time (Figure 3,4). No other factors were recognized. We conduct a complete routine laboratory investigation for urinary-tract infection. Her Pap-test result was negative, urine culture grew Proteus Mirabilis Vulgaris 1.000.000 bacterium/ml, vaginal culture test showed bacterial vaginosis.
Figure 3. Erythema Annular Centrifuge. Spreading Gradually to Form Large Rings a Mild Central Hyperpigmentation (Right Leg).
Figure 4. Erythema Annular Centrifuge. Spreading Gradually to Form Large Rings A Mild Central Hyperpigmentation (Left Leg).
Erythema annular centrifugal (EAC) was first described by Darier in 1916 and classified in 1978 by Ackerman into a superficial and a deep type [2, 8]. It is believed that EAC represents a cutaneous manifestation to different causes and underlying systemic diseases, drug reactions (finasteride, chloroquine, hydroxychloroquine, hydrochlorothiazide, piroxicam, etizolam, cimetidine, penicillin, salicylates, spironolactone, gold sodium thiomalate, amitriptyline, ustekinumab, rituximab), endocrine and immunological disorders (menstrual cycle, Graves disease, Hashimoto thyroiditis, Sjögren syndrome, autoimmune progesterone dermatitis), hematological and other neoplastic disorders (Hodgkin lymphoma, non- Hodgkin lymphoma, acute leukemia, histiocytosis, multiple myeloma, nasopharyngeal carcinoma, prostatic adenocarcinoma, breast carcinoma, ovarian carcinoma, food allergy, arthropod bites [1, 4, 9, 11, 15].
Bacterial infections, dermatophytosis, and Candida have been associated with the causal factors of eythema annular centrifugal EAC.
The suspected risk factors for the development of sensitization o enoxaparin are prolonged intake of the drug [14]. Applying the differential diagnosis for all figurate annular erythemas eruption, includes tinea, eczematous and dermatitic conditions connective tissue disease and cutaneous T-cell lymphoma.
The tumor screen was negative. Even though she lives in an apartment we did her the examination to Borrelia as we know the linkage between Borrelia and urticaria. The Borrelia antibodies, IgG, IgM was negative, skin biopsy excluded all the above diseases (without epidermal involvement).
The total body tomography was normal (excluding all the possible malignancy). Examination with all allergy skin tests including skin prick tests, native prick by prick tests, patch test, provocation tests for enoxaparin, IDR, were all negative. Serum protein electrophoresis, complement levels, tests for antinuclear antibodies, human immunodeficiency virus, hepatitis B and C viruses were all negative too. Chest X-ray, total body CT, and abdominal ultrasonography results were also normal. A positive urine-culture for Proteus Mirabilis Vulgaris 100.000 bacterium [CFUs]/mL) (as the patient was hospitalized in the gynecology department for 5(five) days, known as a potent nosocomial pathogen).
Proteus mirabilis is a Gram-negative bacterium which is wellknown as responsible for complicated urinary tract infections (UTIs) isolated from patients with underlying diseases or compromised immune systems Clinically, this organism is most frequently a pathogen of the urinary tract, particularly in patients undergoing long-term catheterization, abnormalities of the urinary tract, urethral instrumentation [7]. We used topical and systemic glucocorticoids as initial treatment for EAC. The response was usually discouraging and recurrence was the rule in many cases, treated with ciprofloxacin 400mg/200ml x2 for 14 days corticosteroid and antihistaminics, After five week patient was admitted to our hospital with the same clinic, the same skin eruption, the same histopathological characteristics of the first time (Figure 3,4). Our patient had described that the lesions were intensely itchy, urine culture grew Proteus Mirabilis 1.000.000 bacterium [CFUs]/mL). She was treated with levofloxacin 500 mg X2 for 14 days, corticosteroid and antihistamines. The skin eruption regressed spontaneously 2 weeks after beginning.
In inclusion to urinary tract infection, this pathogen can also cause infection in the eye, ear, nose, respiratory tract, skin, throat, burns, and wounds and has been implicated in neonatal meningoencephalitis [7, 12].
Conclusion
Erythema Annulare Centrifugal in adult patients is a large group of diseases whose differentiation is difficult and only delicate variations in the laboratory and clinicopathologic features allow the right diagnosis. In this report, we presented a case of P. mirabilis infection associated with polycyclic skin lesion diagnosed as EAC, a variant of EAC characterized by a chronic persistent course during Proteus Mirabilis colonization episodes and by a complete resolution of the lesions after the bacteria eradication. The coexistence of the significant ascend and drop of Proteus mirabilis bacterial counts of colony-forming units [CFUs]/mL) with the clinical appearance of skin eruption of erythema annular centrifugal dynamically suggests a pathogenetic effect of the gram-negative bacteria on the skin lesions.
References
- Bottoni U, Innocenzi D, Bonaccorsic P, Carlesimo M, Faina P, Richetta A, et al. Erythema annulare centrifugum: report of a case with neonatal onset. J Eur Acad Dermatol Venereol. 2002 Sep;16(5):500-503. PubMed PMID: 12428847.
- Weyers W, Diaz-Cascajo C, Weyers I. Erythema annulare centrifugum: Results of a clinicopathologic study of 73 patients. Am J Dermatopathol. 2003 Dec;25(6):451–62. PubMed PMID: 14631185.
- Ibrahim SF, Pryor J, Tausk FA. Stress-induced erythema annulare centrifugum. Dermatol Online J. 2009 Apr 15;15(4):15. PubMed PMID: 19450408.
- Chou WT, Tsai TF. Recurrent erythema annulare centrifugum during ustekinumab treatment in a psoriatic patient. Acta Derm Venereol. 2013 Mar 27;93(2):208-209. PubMed PMID: 22983014.
- Shelley WB, Shelley ED. Erythema annulare centrifugum as the presenting sign of the hypereosinophilic syndrome: Observations on therapy. Cutis. 1985 Jan;35(1):53-55. PubMed PMID: 3967515.
- Halevy S, Cohen AD, Lunenfeld E, Grossman N. Autoimmune progesterone dermatitis manifested as erythema annulare centrifugum: Confirmation of progesterone sensitivity by in vitro interferon-gamma release. J Am Acad Dermatol. 2002 Aug;47(2):311-313. PubMed PMID: 12140482.
- O'Hara CM, Brenner FW, Miller JM. Classification, identification, and clinical significance of Proteus, Providencia, and Morganella. Clin Microbiol Rev. 2000 Oct;13(4):534-546. PubMed PMID: 11023955.
- Roxburgh AC. Annular Centrifugal (“Erytheme Annulaire Centrifuge,” Darier, 1916). Proc R Soc Med. 1931 Oct;24(12):1645-1646. PubMed Central PMCID: PMC2182479.
- Mahood JM. Erythema annulare centrifugum: a review of 24 cases with special reference to its association with underlying disease. Clin Exp Dermatol. 1983 Jul;8(4):383-387.
- Espana A. Figurate erythemas in dermatology. In: Bolognia JL, Jorizzo JL, Rapini RP, editors. Dematology. 2 nd ed. Spain: Mosby Elsevier; 2008. 277- 86.
- Kim KJ CS, Chang SE, Choi JH, Sung KJ, Moon KC, Koh JK. Clinicopathologic analysis of 66 cases of erythema annulare centrifugum. J Dermatol. 2002 Feb;29(2):61-67. PubMed PMID: 11890297.
- Matthews SJ, Lancaster JW. Urinary tract infections in the elderly population. Am J Geriatr Pharmacother. 2011 Oct;9(5):286-309. PubMed PMID: 21840265.
- Minni A, Sarro R. Novel therapeutic approach to erythema annulare centrifugum. J Am Acad Dermatol. 2006 Mar;54(3 Suppl 2):S134-5. PubMed Central PMCID: PMC2182479.
- Nguyen HV, Antony AM. Hypersensitivity skin reaction to enoxaparin. Aust Prescr. 2011 Oct 1; 34(5):1-2.
- Lazar P. Cancer, erythema annulare centrifugum, autoimmunity. Arch Dermatol. 1963;87(2):246-251.
- Schaffer JN, Pearson MM. Proteus mirabilis and Urinary Tract Infections. Microbiol Spectr. 2015 Oct; 3(5):10. PubMed Central PMCID: PMC4638163.
- Rosina P. Erythcema annulare centrifugum and pregnancy. Int J Dermatol. 2002 Mar;41(8):516-517.
- Burgdorf HC. Erythema annulare centrifugum and other figurate erythemas. 8th ed. In: Freedberg IM, Eisen AZ, Wolff K, Katz SI, Goldsmith LA, Austen KF, et al. editors. Fitzpatrick’s Dermatologyin general medicine.