Factors Influencing the Success of Treatment in Anisometropic Amblyopia
Sedarous F1, Musewe T2, Mao AJ2, Makar I2*
1 University of Toronto, Toronto, Canada.
2 Ivey Eye Institute, University of Western Ontario, London, Canada.
*Corresponding Author
Dr. Inas Makar,
Ivey Eye Institute, University of Western Ontario,
London, Ontario, Canada, N6A 4V2.
Tel: 1-519-685-8281
Fax: 1-519-646-6149
E-mail: Inas.Makar@lhsc.on.ca
Received:August 08, 2017; Accepted: September 04, 2017; Published: September 05, 2017
Citation: Sedarous F, Musewe T, Mao AJ, Makar I. Factors Influencing the Success of Treatment in Anisometropic Amblyopia. Int J Ophthalmol Eye Res. 2017;5(7):329-333. doi: dx.doi.org/10.19070/2332-290X-1700067
Copyright: Makar I© 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Purpose: To examine factors influencing successful resolution of amblyopia in children with hyperopic and astigmatic anisometropia presenting to a pediatric ophthalmology practice in London, Ontario.
Methods: A retrospective chart review was conducted to identify children treated for hyperopic and astigmatic anisometropia from 2008-2016. 39 children ages 12 years and under with hyperopic and astigmatic anisometropia were included. Information regarding referral pattern, presenting findings and outcomes was collected. Presenting degree of anisometropia, compliance, age at presentation and initial visual acuity (VA) were all statistically analyzed to determine effect on final VA.
Results: The mean age at referral to pediatric ophthalmology was 5.2 years. 47% presented with dense amblyopia, with the poorer eye having a VA of 6/30 or worse. 51% of children were successfully treated, with a final VA of 6/9 or better in the worse eye, and 5% of children had residual dense amblyopia. Presenting magnitude of anisometropia was the only factor found to have a significant effect on successful treatment, as for every one diopter decrease in magnitude of anisometropia, there was a 40% higher odds of achieving a final VA of 6/9 or better (point estimate 0.62, 95% CI 0.39-0.97, p=0.03). Age at presentation, presenting VA and compliance to treatment all had no significant outcome on treatment success.
Conclusions: Magnitude of anisometropia was found to be the only significant factor that influences the final visual acuity of children, confirming the necessity for early detection of amblyogenic refractive errors.
2.Introduction
3.Methods
4.Results
5.Discussion
6.Conclusion
7.References
Keywords
Anisometropia; Amblyopia; Hypermetropia; Astigmatism; Pediatric.
Introduction
Amblyopia is a developmental disorder that degrades spatial vision and stereopsis. It is believed to follow abnormal binocular interaction or visual deprivation during early life, and is the most common cause of visual morbidity in childhood [1, 2]. A specific subtype, anisometropic amblyopia, develops when the image on the retina of one of the eyes is chronically de-focused caused by unequal refractive errors in both eyes. Mild degrees of hyperopic or astigmatic anisometropia (1.00-2.00 D) can cause amblyopia, whereas higher levels of refractive error are usually required by myopic anisometropes to develop severe amblyopia [2]. Anisometropic amblyopia tends to be detected and consequently treated later than other forms of amblyopia as some children with anisometropia have no noticeable ocular misalignment. Consequently, these children may develop irreversible visual loss due to delayed diagnosis.
Data regarding the prevalence of anisometropia as well as other ocular diseases among children in Canada is scarce. A few studies conducted in three cities across Newfoundland, New Brunswick and Ontario found the prevalence of pediatric anisometropia to range between 1.4 and 3.6%, which is similar to what has been reported among other developed nations (0.9-3.1%) [3-5].
Without treatment, children are at risk for deterioration of existing amblyopia [6]. Various factors influence the outcome of visual acuity following amblyopia treatment in this group of children. Patching regimens, initial visual acuity, the age of the subject at the start of treatment, level of compliance with treatment, the presence of significant astigmatism, and binocular vision status have all been shown to have significant influence on final visual acuity following treatment [7-10].
There is limited literature investigating visual outcomes for children with anisometropia in Canada. The purpose of this study was to examine factors affecting final visual outcome following the treatment of children diagnosed with hyperopic and astigmatic anisometropia, presenting without apparent strabismus to a single surgeon’s pediatric ophthalmology practice in London, Ontario.
Methods
A retrospective chart review was performed. The research protocol was approved by the Research Ethics Board of the University of Western Ontario. A computer search of the patient database of one pediatric ophthalmologist (IM) at the Ivey Eye Institute, University of Western Ontario, was performed to identify the records of all children ages 12 and under who presented with anisometropia upon referral from 2008-2016. We included all children who presented with anisometropia, defined as a spherical equivalent of ≥ 1.00 D between both eyes and/or ≥ 1.50 D difference in cylinder [11]. We excluded all patients older than 12 years at admission, those with inadequate follow up, any other pathology that could influence vision (e.g. ptosis, deprivation amblyopia) and/or those with a corrected manifest deviation greater than 10 prism diopters. A total of 57 patients were identified with anisometropia. 53 of them had anisometropic hyperopia/astigmatim and 4 had anisometropic myopia. We have complete data on 39 children presenting with hyperopic and astigmatic anisometropia that we included in our analysis.
The following data was recorded: age at initial admission, reason for presentation to referring doctor, present prescription and history of past managements. We documented the presence of family history of amblyopia and/or strabismus, the presenting and final: visual acuity, cycloplegic refractions and ocular alignment. We also documented compliance with treatment and final sensory testing including worth 4-dot test for distance and near as well as stereoacuity.
Presence of amblyopia was defined as ≥ 2 lines difference of visual acuity between both eyes as measured by any test used in the clinic including Allen pictures singles, Snellen's singles or Snellen's linear depending on the child's age and cooperation [12]. Dense amblyopia was defined as visual acuity of 6/30 or worse. The magnitude of anisometropia was calculated based on the difference in spherical equivalence between both eyes.
Compliance with the prescribed treatment regimen was graded as good-to-fair when instructions were followed at least 50% of the time or if good compliance was documented in the patient's chart by the treating physician or the orthoptists. Compliance was deemed poor when instructions were followed less than 50% of the time or if it was documented as such by the treating physician or the orthoptists. Final visual acuity of 6/9 or better was defined as a successful treatment outcome, whereas final vision worse than 6/9 was chosen to represent a failed treatment outcome. A multivariate logistic regression analysis was performed on four factors to assess their effect on final visual acuity following treatment, with a p-value of ≤ 0.05 being considered statiscally significant. Visual acuity values were converted to logMAR values for statistical purpose.
Statistical analysis was performed using the SAS 9.1 software package (SAS Institute, Cary, NC). Univariate correlation between four potential predictors of interest and treatment success was analyzed using a Fisher exact test for categorical variables and T-test for continuous variables. Multivariate logistic regression analyses using a backward elimination algorithm were used to identify the independent clinical factors that would be associated with successful treatment with a cutoff P ≤ 0.05.
Results
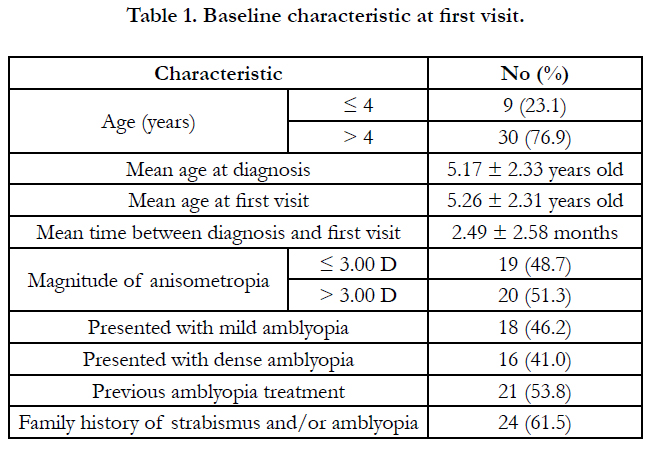
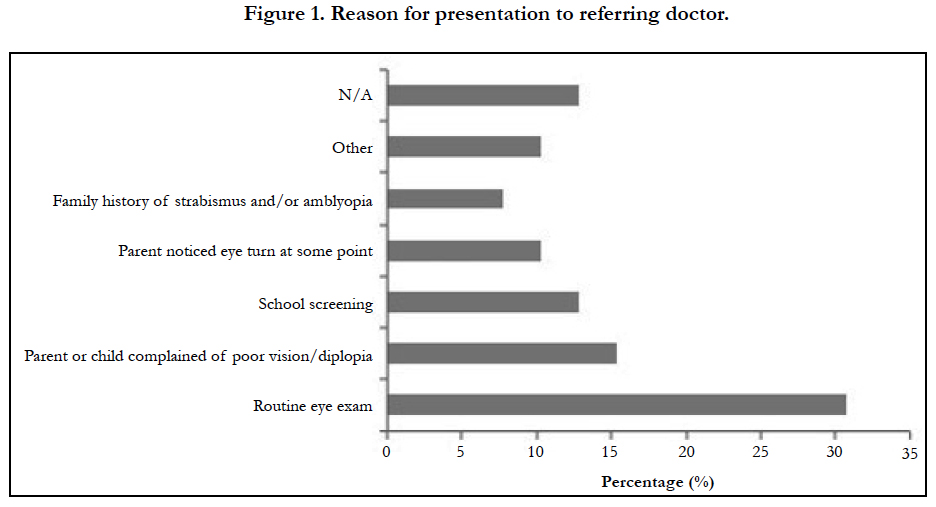
Data from the 39 patients who had adequate follow up was used for statistical analysis and to determine baseline characteristics. Baseline characteristics are presented in Table 1. 27 patients (69.2%) were referred by optometrists and 12 (30.8%) were referred by physicians (family physician, pediatrician or ophthalmologist). Reasons for presentation to the referring doctor are portrayed in Figure 1. No significant correlation was found between presenting degree of anisometropia and presenting visual acuity. 16 children (47.1%) presented with dense amblyopia (6/30 or worse). Of those 16 children, 75% had > 3.00 diopters of anisometropia and 63% had previously attempted patching prior to referral and 94% presented to our clinic older than 4 years of age.
All 39 subjects were prescribed glasses as part of their treatment regimen, 2 (5.1%) had glasses as their sole treatment. 36 (92.3%) underwent a patching regimen and 5 underwent atropine penalization as part of their treatment as well. One child had a skin disease hindering the use of patching and was treated successfully with atropine penalization. 33 (84.6%) subjects were noted to have good-to-fair compliance, while 6 (15.4%) had poor compliance.
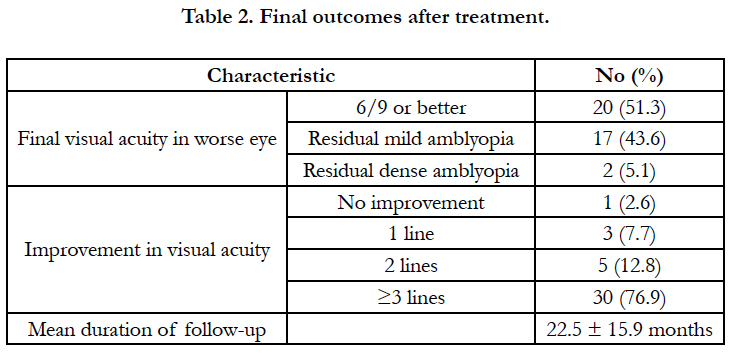
Final outcomes after treatmentare portrayed in Table 2. Overall, 20 (51%) children were successfully treated, with a final visual acuity of 6/9 or better in the worse eye. 8 (40%) of them presentedto the clinicless than4 years old, 13 (65%) presented with a magnitude of anisometropia ≤ 3.00 D. All were noted to have good-to-fair compliance and only 4 (20%) of those 20 childrenhad dense amblyopia at their first visit.
17 (44%) children were found to have residual mild amblyopia worse than 6/9 but better than 6/30 at their final follow up visit. All but one of the 17 children were older than 4 years at presentation, 6 (35%) presented with a magnitude of anisometropia of ≤ 3.00 D, 10 (59%) had presented with dense amblyopia at their first visit and 4 (24%) were noted to have poor compliance with the offered treatment.
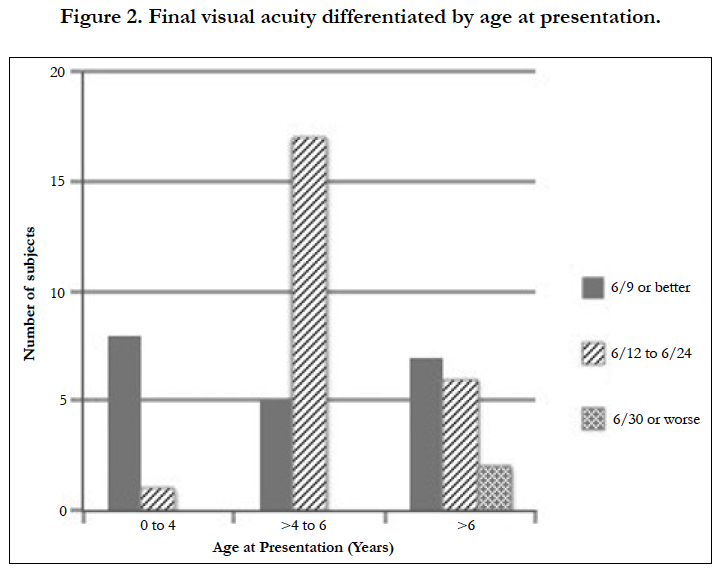
2 children (5%) had residual dense amblyopia at their final follow up visit, both children initially presented above the age of 7, presented with a magnitude of anisometropia > 3.00 D and were noted to have poor compliance with the offered treatment. These 2 children had no evidence of fusion or stereopsis at their final visit. Final visual acuity distributed by age of presentation is portrayed in Figure 2.
At the final visit, 7 (17.9%) children showed a stereopsis of 60 seconds of arc or better and 9 (23.1%) had no evidence of stereopsis. Of these 9 children, 8 presented above the age of 4 years and presented with dense amblyopia. Following treatment, 6 of these 9 children had residual mild amblyopia and 3 children hadresidual dense amblyopia.
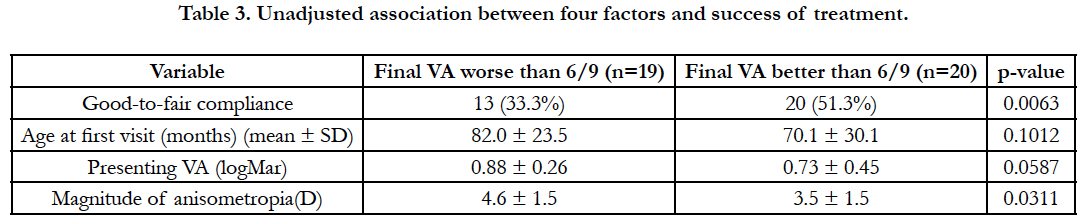
Presenting degree of anisometropia, compliance, age at presentation and initial visual acuity were all statistically analyzed to determine effect on final visual acuity. Table 3 portrays the unadjusted association between these four factors and success of treatment. Upon univariate analysis, presenting degree of anisometropia (P = 0.0311) and compliance with treatment (P = 0.0063) were both initially found to be statistically significant in regards to success of treatment. However, once the confounding effect was adjusted by multivariate regression analysis, the adjusted association of compliance on the success of treatment was no longer statistically significant. Multivariate logistic regression analyses identified magnitude of anisometropia at presentation as the only factor found to have significant effect on successful treatment. For every one diopter decrease in magnitude of anisometropia, there was an approximately 40% higher odds of achieving a final VA of 6/9 or better, while adjusting for all other factors including compliance with treatment, presenting visual acuities and age at first visit (point estimate 0.62, 95% CI 0.39-0.97, P =0.039).
Discussion
The results from this study demonstrate that magnitude of anisometropia has a significant influence on the final visual acuity of children diagnosed with hyperopic and astigmatic anisometropia, while presenting age, presenting visual acuity, and compliance to treatment regimen do not.
The literature currently remains contradictory regarding the major factors that influence final visual outcome in children with anisometropia. These factors include the effect of age at presentation and initiation of treatment, and the influence of degree of anisometropia on treatment success. Hussein et al., demonstrated an increased risk of treatment failure if treatment was started after the age of 6 years old [8]. However, Cobb et al., and Chen et al., found no correlation between age and treatment success [13, 14]. Our data demonstrated that age had no significant impact on the success of treatment.
A statistically significant positive trend exists in our data among children presenting with lower degrees of anisometropia and successful treatment. This finding is consistent with the findings of Lee et al., and Cobb et al., who have demonstrated a positive influence of smaller refractive errors on treatment success, while Hussein et al., demonstrated no effect of the amount of difference in refraction between both eyes on treatment success [8, 14, 15]. Our data differs from several other studies with regards to the effect of compliance and presenting visual acuity on treatment success. Our study demonstrated that presenting with worse visual acuity had no significant correlation with success of treatment, which was inconsistent with the results of Hussein et al., and Chekitaan et al., [8, 16]. The age of participants in these two studies is 3 years and above, whereas our study included participants younger than 1 year of age [8, 16]. Visual acuity measurements in young children are more difficult and less accurate than in older children, resulting in a lack of standardized initial visual acuity in our study (Allen picture singles, Snellen’s singles or Snellen’s linear depending on cooperation) which might explain our findings. Furthermore, compliance had no significant effect on the success of treatment according to our data. These results are in contrast to several other studies, perhaps due to differing criteria used in defining compliance among studies [8, 13, 16].
Our study has several limitations, including a small study number reducing the power of statistical analysis. Our reduced numbers is due to the fact that we excluded all children with mixed amblyopia (strabismic and anisometropic) since we wanted to examine children who would not have any presenting sign and would have only been identified by screening program or by routine optometrist visit. Our study is a retrospective review; the method in which vision was measured was not standardized, but rather depended on the level of cooperation of the child. However, final visual acuity was measured using Snellen’s linear in 38 of the 39 children. This study was conducted in a tertiary care centre, hence referrals were mostly for children who were diagnosed with amblyopia or failed previous treatment. This may represent a group with unique treatment challenges in comparison to a community optometrist practice that treats many other children diagnosed with anisometropia and have good compliance without the need for referral to our unit.
Our study adds to the limited literature on anisometropia among Canadian children and demonstrates the importance of early screening for anisometropia to detect children with high magnitude of anisometropia who are at a higher risk for residual amblyopia. Unlike several other Canadian provinces, there is no universal screening program in Ontario to effectively detect amblyopia or anisometropia in children [17]. In our study school screening (13%) was the third most common reason for presentation to the referring doctor, following routine eye examinations (30.8%) and complaints of poor vision or double vision (15.4%). The relatively low rates of detection from school screening and following complaints of poor vision compared to coincidental discovery on routine eye examinations found in our study speak to the need of effective early screening as children are usually asymptomatic and the depth of amblyopia tends to increase with longer duration of undiagnosed amblyogenic refractive error [18].
Conclusion
Overall, our results demonstrate that the presenting degree of anisometropia has a significant influence on the final visual acuity of children diagnosed with anisometropic hyperopia and astigmatism confirming the necessity for early detection of significant amblyogenic refractive error. In contrast with the literature our study demonstrated that compliance with treatment, age at presentation and initial presenting visual acuity did not influence the final visual outcome in children presenting with anisometropic amblyopia.
References
- Levi DM, Knill DC, Bavelier D. Stereopsis and amblyopia: A mini-review. Vision Res. 2015 Sep;114:17-30.
- Raab EL. Basic and clinical science course (BCSC): Section 6: Pediatric Ophthalmology and Strabismus. 2011 Ed. American Academy of Ophthalmology, San Francisco, CA; 2011.
- Robinson B, Bobier WR, Martin E, Bryant L. Measurement of the validity of a preschool vision screening program. Am J Public Health. 1999 Feb;89(2):193–198.
- Woodruff ME. Vision and refractive status among Grade 1 children in the province of New Brunswick. Am J OptomPhysiol Opt. 1986 Jul;63(7):545– 552.
- Drover JR, Kean PG, Courage ML, Adams RJ. Prevalence of amblyopia and other vision disorders in young Newfoundland and Labrador children. Can J Ophthalmol. 2008 Feb;43(1):89-94.
- Simons K, Preslan M (1999) Natural history of amblyopia untreated owing to lack of compliance. Br J Ophthalmol. 1999 May;83(5):582-587.
- Stewart CE, Fielder AR, Stephens DA, Moseley MJ. Treatment of unilateral amblyopia: Factors influencing visual outcome. Invest Ophthalmol Vis Sci. 2005 Sep;46(9):3152-3160.
- Hussein MAW, Coats DK, Muthialu A, Cohen D, Paysse EA. Risk factors for treatment failure of anisometropic amblyopia. J AAPOS. 2004 Oct;8(5):429-434.
- Loudon SE, Polling J, Simonsz HJ. Electronically measured compliance with occlusion therapy for amblyopia is related to visual acuity increase. Graefe's Arch Clin Exp Ophthalmol. 2003 Mar;241(3):176-180.
- Flynn JT, Schiffman J, Feuer W, Corona A, Thompson JR, Corona A, et al. The therapy of amblyopia: An analysis comparing the results of amblyopia therapy utilizing two pooled data sets. Trans Am Ophthalmol Soc. 1999;97:373-390.
- Weakley DR. The association between anisometropia, amblyopia, and binocularity in the absence of strabismus. Trans Am Ophthalmol Soc. 1999;97:987-1021.
- Dobson V, Miller JM, Clifford-Donaldson CE, Harvey EM. Associations between anisometropia, amblyopia, and reduced stereoacuity in a schoolaged population with a high prevalence of astigmatism. Invest Ophthal Vis Sci. 2008 Oct. l49(10):4427-4436.
- Chen PL, Chen JT, Tai MC, Fu JJ, Chang CC, Lu DW. Anisometropic amblyopia treated with spectacle correction alone: Possible factors predicting success and time to start patching. Am J Ophthalmol. 2007 Jan;143(1):54-60.
- Cobb CJ, Russell K, Cox A, MacEwen CJ. Factors influencing visual outcome in anisometropicamblyopes. Br J Ophthalmol. 2002 Nov;86(11):1278- 1281.
- Lee CE, Lee YC, Lee S. Factors influencing the prevalence of amblyopia in children with anisometropia. Korean J Ophthalmol. 2010 Aug;24(4):225- 229.
- Chekitaan, Karthikeyan B, Meenakshi S. The results of treatment of anisomyopic and anisohypermetropic amblyopia. Int Ophthalmol. 2009 Aug;29(4):231-37.
- Mema SC, McIntyre L, Musto R. Childhood vision screening in Canada: Public health evidence and practice. Can J Public Health. 2012 Feb;103(1):40-45.
- Donahue SP. The Relationship between anisometropia, patient age, and the development of amblyopia. Trans Am J Ophthalmol. 2005 Dec;142(1): 132-141.