The Affect Of Religious Cognitive-Behavior Therapy On Quality Of Life Obsessive –Compulsive Disorder
Sh Akuchekian, L Nader Nabi, V Emranifard, M Najafi, A Almasi*
Behavioral Sciences Research Center, Isfahan University of medical sciences, Isfahan, Iran.
*Corresponding Author
Asiyeh Almasi,
Behavioral Sciences Research Center,
Isfahan University of medical sciences,
Isfahan, Iran.
E-mail: as8psyco@gmail.com
Received: December 04, 2014; Accepted: January 27, 2015; Published: January 28, 2015
Citation: Sh Akuchekian, L Nader Nabi, V Emranifard, M Najafi, A Almasi (2015) The Affect of Religious Cognitive-Behavior Therapy on Quality of Life Obsessive –Compulsive Disorder. Int J Behav Res Psychol, 3(1), 71-74. doi: dx.doi.org/10.19070/2332-3000-1500013
Copyright: A Almasi© 2015. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Obsessive –compulsive disorder is one the most common psychiatric disorder and strong to treatment that affect on patients quality of life. It is widely supposed that religious is one of the most background in OCD. The aim of this study was evaluated the affect religious cognitive behavior therapy on OCD patients with religious contents. 39 OCD patients were initially recruited. The patients were assed with Y-BOCS and WHO QOL_brife before and after treatment. Norm values were driven from general population to characterized by randomize into 2 sample as well as a recently enlisted psychiatric and control sample, that analyzed by Wilcoxon test and Pierson correlation. The results show significant differences Y_BOCS and WHO QOL scores before and after treatment P < .001. On the basis of the above data, it's possible to predict that religious cognitive behavior therapy can be effective to reduce OCD severity symptoms and enhance QOL in obsessive- compulsive disorder.
2.Background
3.Methodology
4.Assessment
4.1.Yale-Brown Obsessive - Compulsive scale
4.2.WHO-QOL-Brief
5.Result
6.Discussion
7.References
Keywords
Obsessive Compulsive Disorder (OCD); Religious cognitive Behavioral Therapy (RCBT); quality of life.
Background
Obsessive-compulsive disorder (OCD) is represented by a various group of symptoms that include intrusive thoughts, rituals, preoccupations, and compulsions. These recurrent obsessions or compulsions cause severe distress to the person. OCD patients attempt to prevent hurt or correct mistakes and most of the time they are superfluity in front of real threat. The obsessions or compulsions are time-consuming and interfere significantly with the person's normal routine, occupational functioning, usual social activities, or relationships. A patient with OCD may have an obsession, a compulsion, or both [1]. The World Health Organization has reported that OCD accounts for 2.5% of global years lost due to disability [2]. Given the high rates of disability and impairment associated with OCD and comorbid conditions, it is not surprising that quality of life (QoL) will be negatively affected by the presence of OCD. Evidence indicate, OCD patients report general impairment in their functioning and report poor quality of life (QoL) [3,4], also they suffer from disability in several areas, specially in marital, position, emotional and social functioning [5]. more severe OCD symptoms were related to general impairment in functioning [6]. they can develop any thought, feeling, fear or image and there fore can be present on daily expression of art, love, science and religion [7]. The families of OCD patients report considerable burden Couseillness and decrease their social activities, directing their family into increase feeling of isolation and distress [8]. They also report poor QoL in the domains of physical, psychological wellbeing and social relationships [9]. The main goal of this study was the affect of religious cognitive –behavior therapy on quality of OCD patients.
Methodology
39 subject were recruited using randomize clinical trails in Noor hospital, Esfahan, Iran, with principle diagnosis of OCD, according the diagnostic manual of mental disorder - fourth edition [10]. Participant were chosen by special criteria.
- OCD diagnosed based on DSM-IV criteria
- no history of head trauma, neurological disorder or mental convention?
- no diagnose of schizophrenia psychotic disorder or abusing any drug and depend on any
- the patients in both group should were been under drug therapy at least for 6 month before CBT. Fulfilled Y_BOCS and WHO QOL before and after treatment.
Data were analyzed by Wilcoxon test and Pearson correlation methods. Demographic traits such as status of marriage, education and job were noted. Also letter of permission was requested from patients by ethic medical committee. Data management and analyses was performed by spss 15
This rater-administered 10-items scale with specific probes and anchors assesses severity of 5 domains for obsessive and compulsive. These domains include time, distress, interference, resistance, and control. This scale, which established reliability and validity, is widely accepted as the major outcome measure for OCD [11]. The symptom checklist, which is included in the Yale-brown obsessive-compulsive scale (Y-BOCS). Y-BOCS developed by Goodman et al. (1989) to assess the type and severity of obsessive-compulsive symptoms. The questioner, was given on two occasions to the patients once at the beginning of the section therapy (step1), and second time on the end of the section therapy (step2), the scale is administered by an interviewer and is composed of 19 questions, but only the first 10 questions (expect for 10, 1b and 6b) are used to calculate the total score. The score for each answer ranges between 0 and 4. The scale also has a symptom Check list for the evaluation of symptom distribution. Patient insight is assessed by question 11.
Used the World Health Organization (WHO) - Quality of Life (QoL) (brief version), to assess global function, quality of life and disability. The WHO - QoL is a 26-item self-administered questionnaire, which emphasizes to the subjective patient’s responses rather than their objective life conditions. The psychometric property is comparable to that of the full version of WHO-QoL [12-13].
This scale asses 4 original health domain: mental health, social relationship, environment or condition and life status. α= 0.92 in psychiatric patients and α= 0.86 in other society [14].
Result
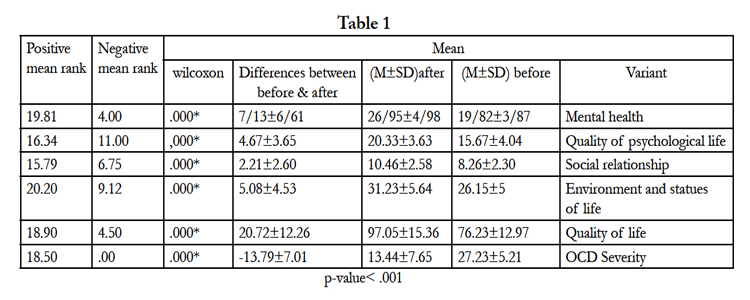
Data shows mean and SD variants wilcoxon, the lowest mean is about QOL in social function domain (beforetreatment means 8.26± 2.30, after treatment 10.46± 2.58). In psychological domain (before treatment 15.67± 4.06, after treatment 20.23± 3.63), quality of life scoresbefore treatment 76.33± 12.97, after treatment 97.05± 15.36.Y-BOCS mean score before treatment 27.23± 5±21, after treatment 13.44± 7.65.
Discussion
Totally quality of life scores have significant differences before and after treatment P-value < 0.01 before treatment was 76.33 ± 12.97 and after treatment 97.05± 15.36.Between total scores mean an all domain of QOL (general health, psychological, functional, social relationship, life status and condition)has significant differences between before and after treatment P-value<.001. Y-BOCS mean score had significant difference P-value < .001 before treatment 27.23± 5±21 and after treatment 13.44± 7.65. Rodrigues in this study report, the mean QOL OCD patients were remarkable low in comparison normal population and delay for treatment Couse to worse. The most striking observation to emerge from the data is that there was negative correlation between Y_BOCS and QOL scorers before treatment(r = 0.398 P = .001) and after treatment (r = .73, p = 0.001). The wilcoxon test in this study showed significant differences between before and after treatment in quality of life and OCD severity (p-value < .001), also in all domain of quality of life showed significant differences, negative mean rank in before and after treatment Y-BOCS test were higher and this show reduce OCD severity (p-value <.001). Positive rank in quality of life is equal with 18.90 that its show higher quality of life after treatment and other domain of quality of life show improve after treatment, Mental health (N.Mean. R=4.00) (P.Mean.R=19.81). Quality of psychological life (N.Mean. R=11.00) (P.Mean.R=16.34). Social relationship (N.Mean.R=6.75) (P.Mean.R=15.79). Environment and statues of life(N.Mean. R=9.12) (P.Mean.R=20.20). These result show, that cognitive behavior therapy based on religious on OCD patients with religious content could be effective on reduce OCD severity and improve quality of life in these patients, because this kind of treatment could be design based on culture and religious patients, and it work on their cognitive and behavior patients. Data in this paper could be confirmation on this claim.
The current study show QOL in OCD patients is low. Assessing the QOL in four domain that contain health, psychological, relationship, social function and condition, that data indicate OCD patients suffer from low relationship, social function and psychological domain, that is correlate with Coran bob and Morise, of course should mention psychological score domain in OCD patients were reasonable to psyzophernia patients. OCD patients have distress about their thoughts, or obsession, because they interpret them as warning of events that are dangerous and likely to occur. Cognitive- behavior therapy was design to help patients identify these automatic unrealistic thoughts and change their interpretation of the meaning of thoughts, resulting in decreased anxiety and compulsion. CBT aim is helping the individual to assemble and experience a new and less threating model of their experience thought developing and aware them how the problems maybe work and then testing out thoughts. Predictors of decreased QOL in obsessive-compulsive disorder (OCD) patients and to explore which aspects of QoL are most affected in OCD. In line with prior research, it was expected that low QoL in OCD patients would be most pronounced for the emotional and social aspects of the construct. Studies looking specifically at QoL in OCD have shown that increases in OCD symptom severity and number of symptoms correlate with greater QoL impairment across all domains [15-3]. Interestingly, some studies have found that QoL impairment is more highly associated with the severity or number of obsessions [15], whereas others have found QOL impairment to be more highly associated with the severity or number of compulsions [3]. Study results have shown that the Y-BOCS compulsion subscale has no relationship to QoL impairment whereas the Y-BOCS obsession subscale contributes significantly to the relationship between QoL impairment in social and occupational functioning and OCD [15]. A study in India compared, family burden across various anxiety disorders, study reported, degree of burden was essentially comparable across all the groups [16]. We hypothesized that patients suffering from severe OCD may have comparable level of global functioning, family burden, QoL and disability with patients suffering from schizophrenia. Knowing that resistance to symptoms plays a protective role in social functioning QoL is important to clinical practice; CBT can be tailored to improve social functioning QoL by incorporating homework’s involving increased social interactions. Motivational interviewing may be useful in enhancing exposure and response prevention techniques by encouraging resistance to symptoms during anxiety-provoking situations [17-18]. Ultimately, treatment for OCD must focus on both symptom reduction through the use of psychotherapeutic techniques and/or psychopharmacology (in severe cases; Foa, 2010) and on the improvement of QoL and daily functioning through psychosocial rehabilitation and the maintenance of symptom attenuation or eradication [19].
Psychopharmacological therapy with various SRIs and psychotherapeutic treatments utilizing CBT are widely used for the treatment of OCD [20]. Attenuation of obsessive-compulsive symptoms with these treatments is often directly related to improvements in verity domains of QoL [21-22]. However, despite the efficacy of both psychopharmacology and CBT attenuating obsessive-compulsive symptoms and improving QoL, there is more work that needs to be done to attain a more complete QoL. Treatments specifically aimed at improving daily functioning for the long-term must be incorporated into psychotherapy with the goal of significantly enhancing QoL [23]. A two-tiered approach, outlined by Bystritsky 2001 suggests that initial treatments must aim to reduce obsessive-compulsive symptoms as they impede QoL and hinder the person’s ability to excel in psychosocial functioning. Subsequently, this treatment must be followed by psychosocial rehabilitation which strives to increase.
QoL by improving social functioning, enhancing coping techniques and aiding with practical goals such as finding appropriate employment. The mediating role of interference of symptoms and resistance to symptomshelps better our understanding of what exactly impacts QoL in persons with OCD. In addition to including psychosocial rehabilitation, psychotherapeutic practice for the treatment of OCD must carefully incorporate CBT techniques (including psych education, cognitive restructuring and exposure and response prevention) that target the reduction of interference and increase efforts to resist symptoms. Knowing that resistance to symptoms plays a protective role in social functioning QoL is important to clinical practice; CBT can be tailored to improve social functioning QoL by incorporating homework’s involving increased social interactions. Motivational interviewing may be useful in enhancing exposure and response prevention techniques. By encouraging resistance to symptoms during anxiety-provoking situations [17].
The conclusions of this study showed well design treatment program concerting the religious cognitive-behavior therapy technics can affect improve quality of life in OCD patients. Some investigates that could corroborate our findings are: Moritz et al (2005), in a study found, Correlations with QoL were most pronounced for depression severity and number of OCD symptoms, QoL was significantly improved in therapy responders relative to nonresponses. Eisen, et al (2006), found Quality of life significantly for all domains evaluated, impaired inverse with published community norms with large effect sizes. The correlations (r) between all domain QOL measures and YBOCS score were significant, ranging from 0.40 to 0.77. Severity of obsessions and depressive symptoms, as well as marital status, was significant predictors to QOL impairment. These findings show that all aspects of QOL are significantly affected by individuals with OCD and are associated with OCD severity (particularly obsessive severity) and depression severity. Exploratory results suggest that QOL and psychosocial functioning significantly affected on YBOCS scores higher than 20. This score might be considerable as a threshold criteria for OCD in Diagnostic and Statistical Manual of Mental Disorders. Eric, et al (2011), the result shows, symptom severity on both the Y-BOCS and the CGI-Severity was negatively correlated with emotional health, social functioning and general health. But there was no significant relationship between obsessive-compulsive symptom severity and physical health QOL. There are number of limitation in this study, first, the sample contain of female and there were no any men in thisstudy, which limit generalize ability, second, didn’t have follow-up test for more validity, and the end, this study done in OCD Clinic in Noor hospital and we can't generalize to other OCD patients. To sum up, our results showthat religious cognitive-behavior therapy can play a considerable role in severity OCD symptoms among religious OCD patients. These training programs should be considerable more as an important component comprehensiveTreatment program for religious OCD patients.
References
- Sadock, Benjamin James; Sadock, Virgimia Alkott, Synopsis of Psychiatry: Behavioral science/ Clinical psychiatry, 10th, 2007.
- World Health Organization (1988) WHO Psychiatric disability assessment schedule (WHO/DAS) with a guide to its use. World Health Organization: Geneva.
- Moritz S, Rufer M, Fricke S, Karow A, Morfeld M, et al (2005). Quality of life in obsessive-compulsive disorder before and after treatment. Compare Psychiatry 46:453-9.
- Masellis M, Rector NA, Richter MA (2001) Quality of life in OCD: Differential impact of obsessions, compulsions and depression comorbidity. Can J Psychiatry, 48:72-7.
- Bystritsky A, Liberman RP, Hwang S, Wallace CJ, Vapnik T, et al (2001). Social functioning and quality of life comparisons between obsessive compulsive and schizophrenic disorders. Depress Anxiety 14:214-8.
- Kim SW, Dysken MW, Kuskowski M. (1990) The Yale-brown obsessive-compulsive scale: A reliability and validity study. Psychiatry Res 34:99-106.
- Eric A Storch, R.Geffken, Tanyak Murphy (2007) Child and Adolescent Obsessive-Compulsive Disorder,universityFlorida, London, Mahwan New Jersey 07430.
- Stengler-Wenzke K, Trosbach J, Dietrich S, Angermeyer MC (2004) Subjective burden and coping strategies of relatives of patients with OCD. J Adv. Nurs 48:35-42.
- Stengler-Wenzke K, Kroll M, Matschinger H, Anger Meyer MC (2006) Quality of life of relatives of patients with obsessive-compulsive disorder. Compr Psychiatry 47:523-7.
- American Psychiatric Association. (2000) Diagnostic criteria from DSM-IV. American Psychiatric Association: Washington (DC).
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado PL, et al. (1989) The Yale-Brown Obsessive Compulsive Scale: I, Validity. Arch Gen Psychiatry a 46:1012-6.
- WHOQOL Group. (1998) Development of the World Health Organization WHOQOL-BREF Quality of life assessment. Psyche Med 28:551-8.
- World Health Organization. (1988) WHO Psychiatric disability assessment schedule (WHO/DAS) with a guide to its use. World Health Organization: Geneva.
- Williams I (2000) Reflection on assessing quality of life and the WHO-QOL-Brief: S.J clui epidemiology 53: 13-17.
- Eisen JL, Mancebo MA, Pinto A, Coles ME, Pagano ME, et al (2006). Impact of obsessive-compulsive disorder on quality of life Department of Psychiatry and Human Behavior, Brown University, Providence, RI 02906, USAJul-Aug 47(4):270-5.
- Chakrabarti S, Kithara P, Vera SK (1993) The pattern of burden in families of neurotic patients. Soc Psychiatry psychiatric Epidemiology 28:172-7.
- Simpson HB, Huppert JD, Petkova E, Foa EB, Liebowitz MR (2006) Response versus remission in obsessive-compulsive disorder J Clin Psychiatry 67(2):269–276.
- Storch EA, Abramowitz JS, Keeley M (2009) Correlates and mediators of functional disability in obsessive-compulsive disorder. Depress Anxiety 26(9):806–813.
- Foa EB, Coles M, Huppert JD, Pasupuleti RV, Franklin ME, et al (2010). Development and validation of a child version of the obsessive compulsive inventory. BehaveThere 41(1):121–132.
- Eric Storch, Ph.D. Vicky Phares, Ph.D. Joseph Vandello, Ph.D. Kevin Thompson, Ph.D (2011) "Quality of Life in Adult Obsessive-Compulsive Disorder: The Role of Moderating and Mediating Variables. Department of Psychology College of Arts and Sciences University of South Florida. Associations between QoL, Symptom Severity and Symptom Dimensions.
- Hollander E, Stein DJ, Fineberg NA, Marteau F, Legault M (2010) Quality of life outcomes in patients with obsessive-compulsive disorder: relationship to treatment response and symptom Relapse. J Clin Psychiatry 71(6):784–792.
- Koran LM, Bromberg D, Hornfeldt CS, Shepski JC, Wang S,et al (2010) Extended-release fluvoxamine and improvements in quality of life in patients with obsessive-compulsive Disorder. Compr Psychiatry 51(4):373–379.
- Bystritsky, A. Liberman, R.P. Hwang, S.Wallace, C.J.Vapnik, et al, (2000) Social Functioning and Quality of Life Comparison between Obsessive-Compulsive and Schizophrenic Disorder. Depression & Anxiety 14:214-218