Early and Long Term Outcomes of Aortic Valve Surgery Combined or Not With CABG Surgery
Selman Dumani1, Elizana Petrela1, Ermal Likaj1, Endri Harja2, Gentian Vyshka3*, Ali Refatllari1
1 University Hospital Center “Mother Theresa”, Cardiac Surgery Service, Tirana, Albania.
2 German Hospital, Tirana, Albania.
3 Faculty of Medicine, University of Medicine in Tirana, Albania.
*Corresponding Author
Gentian Vyshka
Faculty of Medicine,
University of Medicine in Tirana,
Albania.
E-mail: gvyshka@gmail.com
Accepted: February 27, 2014 Published: February 28, 2014
Citation: Vyshka G, et al. (2014) Early and Long Term Outcomes of Aortic Valve Surgery Combined or Not With Cabg Surgery. Int J Clin Ther Diagn. 2(1), 32-38. doi: dx.doi.org/10.19070/2332-2926-140007
Copyright: Vyshka G© 2014. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: The number of patients doing aortic valve surgery with or without CABG(Coronary Artery Bypass Graft) is increasing continuously in our country. The goal of this study is to evaluate the early and long-term results of aortic valve surgery alone or combined with CABG surgery.
Methods: This is a retrospective and prospective study. We included the patients underwent aortic valve surgery (replacement or another procedure) with or without CABG from January 2007 to January 2013 . The population of 330 patients is divided into two groups: Group I included 81 patients combined surgery; Group II included 249 patients with isolated aortic valve surgery. In the early results we referred hospital mortality and perioperative complications. The follow-up time is from 2 to 73 months for 303 cases that were discharged from hospital. The long-term results were evaluated in terms of mean survival ,quality of life and prostheticrelated complications.
Results: The hospital mortality was 3.6 % in general. The hospital mortality: group I is 4. 9% and group II is 3.2 %. The difference is not statistically significant. Low cardiac output, conduction disturbances, stroke, pulmonary complications, renal complications, bleeding, atrial fibrillation, wound infections, ventricular arrhythmias are respectively14. 8% vs. 9. 6%, 3. 7% vs. 6. 9%, 3. 7% vs. 0. 4%, 9. 9 % vs. 2. 8%, 3. 7% vs. 1. 2%, 6. 3% vs. 2.0%, 14. 8 % vs. 19.7%, 11. 3% vs. 1. 6 %, 6. 2% vs. 5. 6 % respectively for the group I and II. The differences were statistically significant only for low cardiac output, stroke, pulmonary and wound complications. The longterm outcomes: overall mortality 3. 9%, bleeding 1. 9%, prosthetic endocarditis and thrombosis 1.3%. Endocarditis and thrombosis are more frequent in group I. During the follow-up survival was 93% and 96% respectively for group I and II, with no significant difference between groups.
Conclusion: Simultaneous coronary artery by-pass with aortic valve increases slightly the operative mortality and perioperative complications. CABG surgery does not influence long–term results of aortic valve surgery.
2.Materials and Methods
1.Patients
2.Surgical technique
3.Statistical analysis
3.Results
1.Operative results
2.Hospital mortality and post-operative morbidity
3.Long-term results
4.Discussion
1.Early results
2.Long-term results
5.Conclusions
6.References
Introduction
Surgery of aortic valve began since the years ‘80 of the last century treating initially the rheumatic and infectious pathology of aortic valve continuing later with degenerative one in our country. It has been seen a trend of change of nature of aortic valve pathology toward atherosclerotic etiology in the last two decades with the change of life style, increase of mean age of population and progression of surgical management of old age patients.
Ischemic heart disease is the most frequent pathology that accompanies the pathology of aortic valve and especially aortic valve stenosis [1, 2] and the most frequent intervention coupled with surgical correction of aortic valve pathology is coronary artery by-pass grafting. We tried to expose our experience in surgical treatment of aortic valve pathology combined or not with CABG surgery in this contest.
Materials and Methods
This is a retrospective and prospective study. All patients included in this study, underwent intervention in two cardiac surgical centers, the first one is public and the other one a private cardiac surgical center in Tirana. The data were collected from hospital records and registers of hospital statistics. Follow-up of patients in long-term is obtained through clinical visits and telephone interviews with patients and/or their family. All survivors underwent a questionnaire regarding the overall health status compared with the time before the operation, current quality of life based on NYHA-s classification, the use of anticoagulants; re-hospitalization and specific complications have been throughout the period after intervention.
Preoperative evaluation of risk of intervention is made according to EUROSCORE [3]. Surgical indication for aortic valve and revascularization surgery are decided according to ESC and AHA/ACC guidelines. [2, 4, 5].
Perioperative mortality and major complications like myocardial infarction, cerebral accidents, pulmonary problems, renal problems, infections and late mortality, complications after early period of surgery as re-hospitalizations, hemorrhage, thromboembolism, thrombus on the prosthesis, endocarditis etc. are considered end-points for the evaluation respectively of early and late results of surgery of aortic valve alone or combined with by-pass surgery.
In this study are included 330 patients that underwent surgery of aortic valve alone or in combination with by-pass surgery from January 2007 to January 2013. The population is divided in two groups. Group I the patients with combined surgery 81 pt. Group II the patients with isolated aortic valve surgery 249 pt.
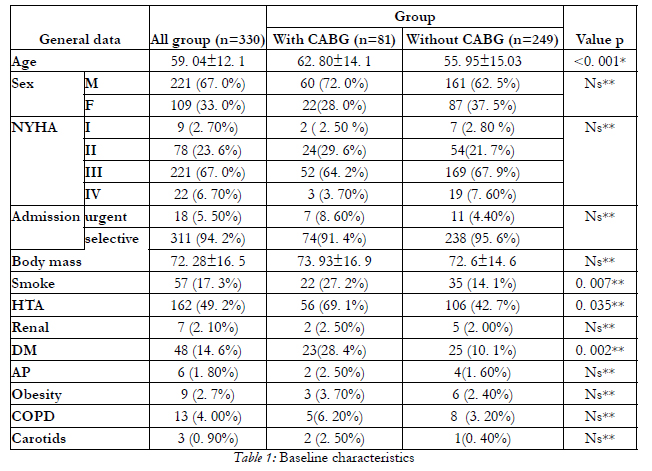
The general demographic and clinical data are presented in Table 1. As we can see in the table below mean age of all population in study is 59. 04± 12.1 years with a higher mean age in group I; there are 221 males and 109 females; there are not significant differences between groups about the comorbidities except diabetes, hypertension and smokers that are more present in group I.
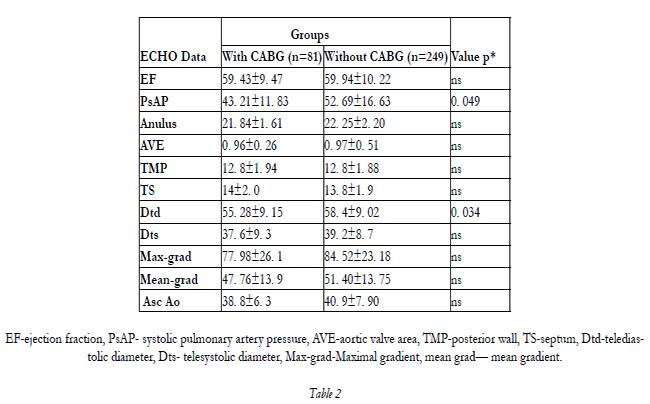
Transthoracic echocardiography was the main diagnostic tool. We see that there were 202 patients with pure aortic stenosis from the echocardiographic data; 73 patients with aortic insufficiency and the rest of patients had mixed pathology of aortic valve (55 pt). Angiography was performed according the guidelines ESC/AHA/ACC [2,4]. The CAD was the primary diagnosis in group 1 in 10 patients. Echocardiographic data are presented in Table 2.
EF-ejection fraction, PsAP- systolic pulmonary artery pressure, AVE-aortic valve area, TMP-posterior wall, TS-septum, Dtd-telediastolic diameter, Dts- telesystolic diameter, Max-grad-Maximal gradient, mean grad— mean gradient.
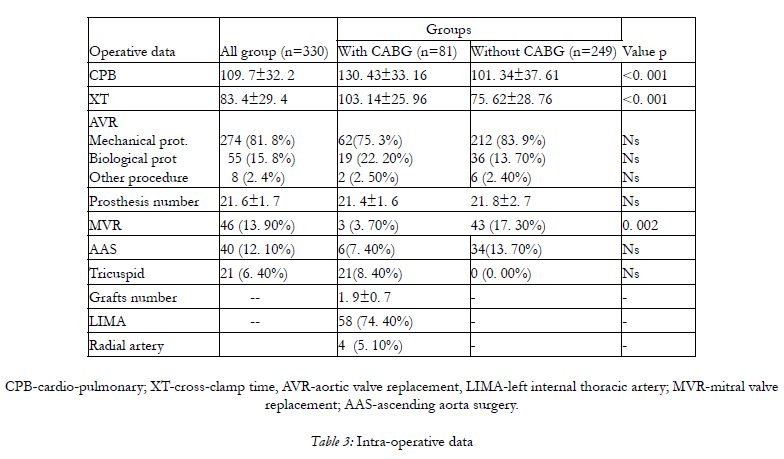
CPB-cardio-pulmonary; XT-cross-clamp time, AVR-aortic valve replacement, LIMA-left internal thoracic artery; MVR-mitral valve replacement; AAS-ascending aorta surgery.
There are not differences between two groups in terms of ejection fraction, gradients, aortic valve opening surface etc. except Dtd.
Standard cardiac surgery monitoring was used. The operation was performed through a complete median sternotomy. Before the institution of cardiopulmonary by-pass the grafts were harvested in group I. The left internal mammary was harvested in the hemiskeletonized fashion. The saphenous vein was harvested in the standard fashion or using the skin bridge technique.
After heparin administration cardiopulmonary by-pass was instituted, aortic cross clamping ante grade cardioplegia was done.
In group I venous coronary artery by-pass was performed first following with the aortic procedure finishing with LIMA grafting. The aortic procedure was performed directly in group II normally.
We made always transverse aortotomy. The leaflets were removed and meticulous decalcification was made. Separated suture technique was performed to implant the aortic prosthesis. Sutures Ticron 2/0 with pledged in the aortic face in most cases and in ventricular face in the rest were used. The heart was de-aired and the aortic clamp removed after the closure of the aorta. At the end of the operation the cannulas were removed and protamine was given. Temporary pacemaker (PM) wires and mediastinal and pleural drains were placed before chest closure.
Continuous variables were presented as mean and standard deviation.
Categorical variables were presented in absolute value and percentages. Student t-test for two independent samples was used to analyze the differences between two continuous variables and χ2-test was used to analyze the differences for categorical variables.
A p-value less than 0. 05 was considered to be statistically significant.
SPSS (Statistical Package for Social Science) 19. 0 was used to analyze data.
Results
As it is expected we have a longer cardiopulmonaryby- pass and ischemic time in the group with combined surgery figured by the table. The difference is statistically significant. There are used 274 mechanical prosthesis, 55 biological prosthesis and in 8 cases we have done procedures such as in 1 case aortic valve repair, in 7 patients we have done aortic annulus enlargement (Manouguain technique). The mean number of grafts is 1.9 +/- 0.7 in the population with combined surgery and the LIMA is used in 58 patients. We can see from a general view of database that it is an increasing trend of biological prosthesis use.
The results about operative mortality and morbidity that are the primary and secondary respectively endpoints of early results are presented in the table 4.
The overall hospital mortality was 3. 6% (12/330). The hospital mortality for Groups I and II was 4.9% (4/81) and 3. 2% (8/249), respectively, with no statistical difference (P = 0. 471). Mortality in the group with combined surgery is higher but without reaching statistical significance. The overall length of ICU and hospital stay is importantly longer in group I than in group II respectively 102. 41±147. 81 hours, 13. 99±14. 20 days versus 65. 17±78. 78 hours, 10. 41±6. 34 days.
About the complications low cardiac output, conduction disturbances, stroke, pulmonary complications, renal complications, bleeding, atrial fibrillation, wound infections, ventricular arrhythmias about the complications are 14. 8% vs. 9. 6%,3. 7% vs. 6. 9%, 3. 7% vs. 0.4%, 9. 9 % vs. 2. 8%, 3. 7% vs. 1. 2%, 6. 3% vs. 2. 0%, 14. 8 % vs. 19. 7%,11. 3% vs. 1. 6 %, 6. 2% vs. 5. 6 % respectively for the group I and II. If we see carefully the results in general we have a greater incidence of complications in group where surgery of aortic valve is accompanied with CABG surgery but only for low cardiac output, stroke, pulmonary, and wound complications, the difference reaches significance.
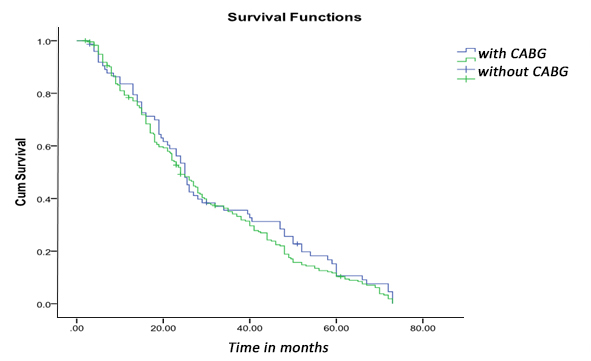
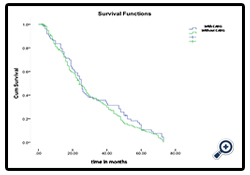
From 318 patients that were discharged from the hospital follow-up is obtained for 95% of them. 15 patients are considered lost. Follow-up time is from 2 to 73 months. During this period 12 patients have died of which 5 patients in group I and 7 patients in group II. The survival statistical analysis for each group noted that for group I mean survival is 31 ± 20. 7 months while for group II 29 ± 19. 6 months (P = 0. 472). Kaplan-Meier curve comparing survival between the two groups shows no significant difference.
Regarding valve prothesis-related complications is noted that at a slightly higher frequency encountered thrombosis and endocarditis of prostheses in the combined surgery. These complications data are presented in the following table (Table 5).
NYHA-class, before and after surgery demonstrates a very important improvement of quality of life for the entire population in the study group. Following the presentation appears that over 90% of patients are independent of cardiac problems.
NYHA-class, before and after surgery
Discussion
Aortic valve surgery occupies an important part in surgical activity in different cardiac surgical centers all over the world. The significant increase of the average age of the population in developed countries, but also in our country, has made this pathology significantly associated with coronary heart disease. Simultaneous surgical correction of aortic valve pathology and performing Coronary Bypass certainly, increase the complexity of the operation and influence the early and late results of intervention. Performing coronary by-pass surgery accompanying gesture of aortic valve surgery has attracted the attention of renowned authors to assess the impact of this gesture in aortic valve surgery. In this context, our study has as priority to report the early and late results of aortic valve surgery isolated or simultaneous with CABG.
From 318 patients that were discharged from the hospital follow-up is obtained for 95% of them. 15 patients are considered lost. Follow-up time is from 2 to 73 months. During this period 12 patients have died of which 5 patients in group I and 7 patients in group II. The survival statistical analysis for each group noted that for group I mean survival is 31 ± 20. 7 months while for group II 29 ± 19. 6 months (P = 0. 472). Kaplan-Meier curve comparing survival between the two groups shows no significant difference.
Regarding valve prothesis-related complications is noted that at a slightly higher frequency encountered thrombosis and endocarditis of prostheses in the combined surgery. These complications data are presented in the following table (Table 5).
NYHA-class, before and after surgery demonstrates a very important improvement of quality of life for the entire population in the study group. Following the presentation appears that over 90% of patients are independent of cardiac problems.
Impact of CABG in long-term results of aortic valve surgery that is treated in numerous papers. [14-16,21-29]. In this group of works is referred that coronary surgery affects adversely survival but without reaching to be independent risk factor in the late results in patients with combined surgery. Brenan et al [21] from a study which has involved 1,026 cardiac surgical centers, reported median survival 12.8 years , 9.2 years , 6.2 years for the group with isolated aortic valve surgery and 10.4 years , 8.2 years and 5.9 years for the group with combined surgery for age groups 65-69 years respectively from 70 to 79 years old and over 80 years old respectively. We can see that combined surgery group has worse prognosis but as independent risk factors are age, renal and pulmonary disease. Folkman et al [14] refer one year post-operative mortality is higher for the combined surgery group 20 % versus 16.2 % for the surgery group with isolated aortic surgery. Also quality of life is reported to be better in a year follow-up for the group with isolated surgery but in both cases there is no statistical significance.
Another group of authors go beyond the fact that CABG affects negatively the results aortic valve surgery. They refer coronary surgery as an independent risk factor [31-36]. Cohen G et al [31] report that survival in the group with combined surgery is significant lower compared with the group with isolated valve surgery that aorta (p < 0. 0001), regardless of age under or over 65 year. In 12 years, survival analyzed in the Kaplan Meier was 65 ± 4 % for the isolated surgery group and 35 ± 8 % for the combined surgery group. Akins et al [32] emphasize that coronary disease and combination with aortic valve surgery significantly reduce survival as much as for the patients with combined surgery the age of implanting biological prostheses may be lower compared with the group with isolated aortic valve surgery. Jones et al [36] refer that adverse influence is significant only in the group with aortic valve replacement is associated with venous graft to the LAD and the number of grafts is not an independent risk factor. In results of our study have no survival difference between the two groups which are 93 % and 96 % respectively for group I and II ( p = 0. 472).
In addition to these facts mentioned above there are also studies with totally different results than discussed above: Kolh et al [16] report hospital mortality 13% in total, 9% for isolated aorta and 24% mortality for combined surgery. CABG emerges as an independent risk factor. In the other side Melby et al [17] report lower mortality in combined surgery 6% vs.10% for isolated aortic valve surgery presented CABG no as risk factor but totally on the other hand as a protector. While in long-term, correcting of aortic valve pathology in combination with coronary bypass, significantly improves survival [37].
Another aspect to discuss was about the use of biological prostheses in relation to mechanical prostheses. Now time, it is confirmed a growing trend to use biological prosthesis in accordance with the indications in the developed world [18-20]. It’s noticed a line with such a trend, even in our experience despite small numbers.
Conclusions
Isolated aortic valve surgery or combined with surgery of coronary arteries in our country achieved very good early and late results comparable to those of developed countries. CABG increases mortality when superimposed aortic surgery compared with the latter isolated, without reaching statistical significance. By-pass coronary surgery does not affect long-term performance of aortic valve surgery. The use of biological prostheses is increasing in aortic valve surgery.
References
- Le Boutillier M, DiSesa JV, Cohn LH. (2008) Cardiac surgery in the adult. Third edition, 1177-1181.
- Bonow RO, Carabello BA, Chatterjee K, De Leon AC Jr, Faxon DP et al (2008). 2008 Focused Update Incorporated Into the ACC/AHA 2006 Guidelines for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease) Endorsed by the Society of Cardiovascular anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J. Am. Coll. Cardiol. 52:e1-e142.
- Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S et al. (1999) European system for cardiac operative risk evaluation (Euro SCORE). Eur J Cardiothoracic Surg 16:9–13.
- Vahanian A, Baumgartner H, Bax J, Butchart E, Dion R et al. (2007). Guidelines on the management of valvular heart disease; The Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology. European Heart Journal 28:230–268
- Hillis D, Smith PK, Anderson JL, Bittl JA, Bridges CR et al. (2011) ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery : A Report of the American College of Cardiology Foundation/ American Heart Association Task Force on Practice Guidelines . Circulation. 124:000–000.
- Bridgewater B, Kinsman R, Walton P, Gummert J, Kappetein AP. (2011) The 4thEuropean Association for Cardio-Thoracic Surgery adult cardiac surgery database report. Inter act Cardiovasc Thorac Surg 12:4-5.
- Wijns W, Kolh P, Danchin N, Di Mario C, Falk V et al. (2010) The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Developed with the special contribution of the European Association for Percutaneous Cardiovascular Interventions. European Heart Journal 31: 2501–2555.
- Zapolanski A, Mak AWC, Ferrari G, Johnson C, Shawa RA et al. (2012) Impact of New York Heart Association classification, advanced ageand patient-prosthesis mismatch on outcomes in aortic valve replacement surgery. Interactive Cardio-Vascular and Thoracic Surgery 0: 1–6.
- Mølstad P, Veel T, Rynning S. (2012) Long-term survival after aortic valve replacement in octogenarians and high-risk subgroups. European Journal of Cardio-Thoracic Surgery0:1–7.
- Kobayashi KJ, Williams JA, Nwakanma L, Gott VL, Baumgartner WA et al. (2007) Aortic Valve Replacement and Concomitant Coronary Artery Bypass: Assessing the Impact of Multiple Grafts. Ann Thorac Surg 83:969-978.
- Sareyyupoglu B, Sundt TM III, Schaff HV, Enriquez-Sarano M, Greason KL et al. (2009) Management of Mild Aortic Stenosis at the Time of Coronary Artery Bypass Surgery: Should the Valve Be Replaced?Ann Thorac Surg 88:1224-1231.
- Hannan EL, Samadashvili Z, Lahey SJ, Smith CR, Culliford AT et al. (2009) Aortic Valve Replacement for Patients With Severe Aortic Stenosis: Risk Factors and Their Impact on 30-Month Mortality. Ann Thorac Surg 87:1741-1749.
- Yilmaz A, Sjatskiga J, Van Boven WJ, Waanders FG, Kelder JC et al. (2010) Combined coronary artery bypass grafting and aortic valve replacement with minimal extracorporeal closed circuit circulation versus standard cardiopulmonary bypass. Interactive CardioVascular and Thoracic Surgery 11:754–757.
- Folkmann S, Gorlitzer M, Weiss G, Harrer M, Thalmann M et al. (2010) Quality-of-life in octogenarians one year after aortic valvereplacement with or without coronary artery bypass surgery.Interactive CardioVascular and Thoracic Surgery 11: 750–753.
- Dell’Amore A, Aquino TM, Pagliaro M, Lamarra M, Zusaa C. (2012) Aortic valve replacement with and without combined coronary bypass grafts in very elderly patients: early and long-term results. European Journal of Cardio-Thoracic Surgery 41: 491–498.
- Kolh P, Kerzmann A, Honore C, Comte L, Limet R. (2007) Aortic valve surgery in octogenarians: predictive factors for operativeand long-term results. European Journal of Cardio-thoracic Surgery 31:600—606.
- Melby SJ, Zierer A, Kaiser SP, Guthrie TJ, Keune JD et al. (2007) Aortic Valve Replacement in Octogenarians: Risk Factors for Early and Late Mortality. Ann Thorac Surg 83:1651-1657.
- Barnett SD, Ad N. (2009) Surgery for aortic and mitral valve disease in the United States: A trend of change in surgical practice between 1998 and 2005. J Thorac CardiovascSurg 137:1422-1429.
- McClure RS, Narayanasamy N, Wiegerinck E, Lipsitz S, Maloney A et al. (2010) Late Outcomes for Aortic Valve Replacement With the Carpentier-Edwards Pericardial Bioprosthesis: Up to 17-Year Follow-Up in 1,000 Patients. Ann Thorac Surg 89:1410-1416.
- Brown JM, O’Brien SM, Wu C, Sikora JAH et al. (2009) Isolated aortic valve replacement in North America comprising 108,687 patients in 10 years: Changes in risks, valve types, and outcomes in the Society of Thoracic Surgeons National Database. J Thorac Cardiovasc Surg 137:82-90
- Brennan MJ, Fred H. Edwards FH, Zhao Y, O’Brien MS et al. (2012) Long-Term Survival After Aortic Valve Replacement Among High-Risk Elderly Patients in the United States: Insights From the Society of Thoracic Surgeons Adult Cardiac Surgery Database, 1991 to 2007. Circulation 126:1621-1629.
- Iung B. (2000) VALVE DISEASE. Interface between valve disease and ischaemic heart disease. Heart 84:347–352.
- He GW, Grunkemeier GL, Starr A. (1996) Aortic Valve Replacement in Elderly Patients: Influence of Concomitant Coronary Grafting on Late Survival Ann Thorac Surg 61:1746-1751.
- Ashikhmina EA, Schaff HV, Dearani JA, Sundt III TM, Suri RM et al. (2011) Aortic Valve Replacement in the Elderly : Determinants of Late Outcome. Circulation 124:1070-1078.
- Desai ND, Merin O, Cohen GN, Herman J, Mobilos S et al. (2004) Long-Term Results of Aortic Valve Replacement With the St. Jude Toronto Stentless Porcine Valve. Ann Thorac Surg 78:2076–83.
- Silberman S, Oren A, Dotan M, et al. (2008) Aortic valve replacement: choice between mechanical valves and bioprostheses. J Card Surg 23:299-306.
- Likosky DS, Sorensen MJ, Dacey LJ, Baribeau YR, Leavitt BJ et al. (2009) Long-Term Survival of the Very Elderly Undergoing Aortic Valve Surgery. Circulation 120:S127-S133.
- Alsoufi B, Karamlou T, Slater M, Shen I, Ungerleider R et al. (2006) Results of Concomitant Aortic Valve Replacement and Coronary Artery Bypass Grafting in the VA Population. The Journal of Heart Valve Disease 15:12-19.
- Mullany CJ, Elveback LR, Frye RL, Pluth JR, Edwards WD et al. (1987) Coronary Artery Disease and Its Management: Influence on Survival in Patients Undergoing Aortic Valve Replacement. J Am Coll Cardiol 10:66-72.
- Cohen G, David TE, Ivanov J, Armstrong S Feindel ChM. (1999) The impact of age, coronary artery disease, and cardiac comorbidity on late survival after bioprosthetic aortic valve replacement. J Thorac Cardiovasc Surg 117:273-284.
- Akins CW, Hilgenberg AD, Vlahakes GJ, MacGillivray ThE, David F et al. (2002) Results of Bioprosthetic Versus Mechanical Aortic Valve Replacement Performed With Concomitant Coronary Artery Bypass Grafting. Ann Thorac Surg 74:1098 –106.
- Jones EL, Weintraub WS, Craver JM. Guyton RA, Shen Y. (1994) Interaction of Age and Coronary Disease After Valve Replacement: Implications for Valve Selection. Ann Thorac Surg 58:378-85.
- Flameng WJ, Herijgers P, Szécsi J, Sergeant PT, Daenen WJ et al. (1996) Determinants of Early and Late Results of Combined Valve Operations and Coronary Artery Bypass Grafting. Ann Thorac Surg 61:621-628.
- Lytle BW, Cosgrove DM, Loop FD , Taylor PC, Gill CC et al. (1983) Replacement of aortic valve combined with myocardial revascularization: determinants of earlyand late risk for 500 patients,1967-1981.Circulation 68:1149-1162,.
- Jones JM, Lovell D, Cranb GW, MacGoana SW. (2006) Impact of coronary artery bypass grafting on survival after aortic valve replacement. Interactive CardioVascular and Thoracic Surgery5:327–330.
- Kurlansky PA, Williams DB, Traad EA, Carrillo RG, Schor JS et al. (2004) The influence of coronary artery disease on quality of life after mechanical valve replacement. J Heart Valve Dis 13:260-71.