Maxillofacial and Cervical Spine Injuries - A Cross Sectional Study on Prevalence and Association of the Both in Maxillofacial Trauma Patients
Rajesh P1, Semmia Mathivanan2, Vaishali V3*
1 Professor and Head, Department of Oral and Maxillofacial Surgery, Chettinad Dental College and Research Institute, Tamil Nadu, India.
2 Associate Professor, Department of Oral and Maxillofacial Surgery, Chettinad Dental College and Research Institute, Tamil Nadu, India.
2 Post Graduate, Department of Oral and Maxillofacial Surgery, Chettinad Dental College and Research Institute, Tamil Nadu, India.
*Corresponding Author
Dr. Vaishali V,
Department of Oral and Maxillofacial Surgery, Chettinad Dental College and Research Institute, Kelambakkam, Chennai- 603103, India.
Tel: 8056379290, 8838017051
E-mail: vaish712.venkat@gmail.com
Received: July 27, 2020; Accepted: November 05, 2020; Published: November 10, 2020
Citation:Rajesh P, Semmia Mathivanan, Vaishali V. Maxillofacial and Cervical Spine Injuries - A Cross Sectional Study on Prevalence and Association of the Both in Maxillofacial Trauma Patients. Int J Dentistry Oral Sci. 2020;7(11):1003-1006. doi: dx.doi.org/10.19070/2377-8075-20000199
Copyright: Vaishali V©2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Aim: To assess the prevalence, and association of maxillofacial and cervical spine injuries in patients sustaining maxillofacial
trauma.
Background: The severity of maxillofacial injuries in a trauma might divert the surgeons’ attention from other concomitant injuries
that could be potentially life threatening if neglected [1]. This study aims to highlight the importance of cervical spine injuries that are often overlooked during maxillofacial examination.
Methods: A cross sectional retrospective analysis of trauma patients reported to the emergency department of a tertiary care
centre in Tamil Nadu during March 2015-March 2020 was done. A detailed review of the maxillofacial trauma cases was done.
Details related to the demography, trauma, injury sustained, primary and secondary survey, records pertaining to the diagnosis of
cervical spine injuries were studied, recorded and subjected to statistical analysis.
Result: 888 out of 6350 patients sustained maxillofacial injuries. Majority of them belonged to the age range of 20-39 years and
the population was predominantly male. 61% of them presented with soft tissue injuries. Among the hard tissue injuries, mandibular
fractures were highest followed by isolated zygomatico-maxillary complex fractures. Cervical spine injuries existed concurrently
in 5.63% of the total number of patients. Prevalence was found higher in combined mandibular and middle third of face fractures
(1.35%) followed by pan facial fractures (1.12%).
Conclusion: Though reported incidence is low, underestimation of these injuries could lead to significant morbid states as
management of the facial fractures essentially involves manipulation of neck that might increase the chances of worsening the
situation further.
2.Introduction
3.Material and Methods
4.Results
5.Discussion
6.Conclusion
7.Refereces
Keywords
Maxillofacial Trauma; Cervical Spine; Fractures; C-Spine Injury.
Introduction
Maxillofacial trauma generally occurs with concomitant injuries
to other systems of the body and adequate expertise and sound
knowledge is expected of every maxillofacial surgeon in the frontline
of trauma care to avoid unnecessary catastrophe. Stephans et
al reported that every 13th polytrauma patient sustained cervical
spine injury with or without neurological symptoms and German
trauma society highlighted the prevalence of 25% of the maxillofacial
injuries in a poly-trauma patient. Rogers et al., [3] reported
that 10% of patients developed neurologic symptoms or their exacerbation
post-emergency care due to failure of recognition or
inadequate immobilization. The Advanced Trauma Life Support
emphasises suspecting cervical spine injury during the management
of patients with injury above the clavicle [4]. All the maxillofacial
trauma cases are thus bound to such an assumption during
the primary and secondary survey. This study aims to assess the
prevalence of cervical spine injury and its association with maxillofacial
trauma.
Materials and Methods
A retrospective cross-sectional unicenter analysis was done on patients
who reported post trauma to the emergency department of
our institution during the period of March 15 to March 2020. Out
of a total of 6350 patients, patients who had sustained maxillofacial
trauma were included in the study and their medical records were studied in detail. Clinical records from the emergency department,
maxillofacial surgical treatment data, interdepartmental
management if present, radiological data including computed
tomography were reviewed. Data including age, gender, type
of injury, frequency of various types of maxillofacial fractures,
prevalence of cervical spine injuries and their frequency and association
with these fractures were analysed. In cases of unavailability
of any of the data pertaining to the information required
for analysis, they were excluded from the study population. All the
data was recorded and subjected to statistical analysis.
Statistical Analysis
The collected data were analysed with IBM.SPSS statistics software
23.0 Version. To describe about the data descriptive statistics
frequency analysis, percentage analysis were used for categorical
variables. Chi square test was applied and Pearson’s correlation
was used to find significance between the variables. In all the
above statistical tools the probability value 0.05 is considered as
significant level.
Results
There were 888 patients with maxillofacial injuries out of 6350
reported trauma cases. Of these 888 patients, 683(75.8%) were males and 215 (24.2%) were females. About 529 (59.6%) of
the study population belonged to the age group of 20-39 years,
while (194) 21.5% were between 40-60 years, (134) 15.1% were
less than 20 years and 31 (3.5%) above 60 years. 545(61.4%) of
them sustained soft tissue maxillofacial injuries and 343 (38.6%)
of them hard tissue injuries. Out of these 343 hard tissue injuries,
148 (16.7%) sustained mandibular fractures, 77 (8.7%) zygomatico-
maxillary complex fractures, 67 (7.5%) combined fracture
of mandibular and middle third of face, 37 (4.2%) maxillary and
finally 17 (1.9%) with pan facial fractures. Cervical spine injuries
associated with maxillofacial injuries was observed in 50 (5.6%)
of the study population. No significant association was found between
the prevalence of cervical spine injuries and the gender. A
significant positive correlation (p<0.000) was found between the
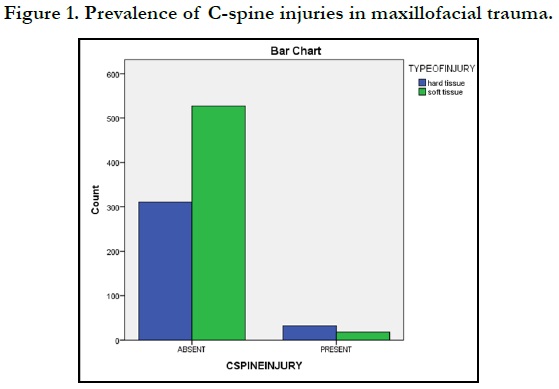
age and prevalence of the injuries. Figure 1 depicts the frequency
of cervical spine injuries observed in soft and hard tissue maxillofacial
injuries. The frequency of existence of c-spine injuries in
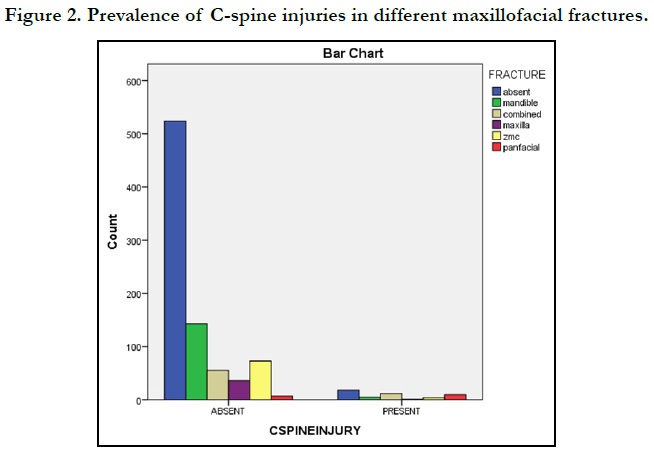
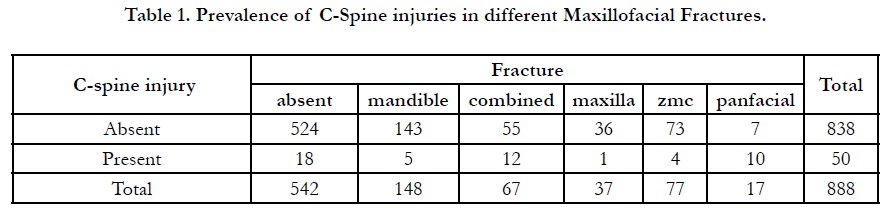
various maxillofacial fractures is given in Table 1 and Figure 2.
Patient with combined fractures of mandibular and middle third
of the face (n=12, 1.3%) has the highest prevalence of c-spine
fractures, followed by pan facial fractures (n=10, 1.1%), isolated
mandibular, zygomatico-maxillary complex and maxillary fractures.
The prevalence of cervical spine injuries among the facial
fractures bore a statistical significance with p<0.000.
Discussion
The association of maxillofacial fractures and the cervical spine
injuries has been reported to range between 1 to 6%. Also such
injuries especially if minor and asymptomatic are missed during
the initial assessment by both the trauma surgeon and the maxillofacial
surgeon due to the narrowed focus on larger life threatening
injuries. But it is important to rule out the occurrence of cervical
spine injuries so as to proceed with the maxillofacial treatment
plan and to avoid any delayed, debilitating exacerbation resulting
from the injury. This is especially crucial when the maxillofacial
fracture is indicated for open reduction and internal fixation,
where active mobilization of cervical spine is done during the
anaesthetic procedures. Such active motions can worse the missed
cervical spine injury that can lead to devastating neurologic consequences.
In our study, out of 889 patients with maxillofacial injuries, 50 of
them had concomitant cervical spine injuries. This forms about
5.6% of the total sample. Previous studies by Follmer et al reported
a prevalence rate of 13%,Alvi et al reported 7.3%, Rocci
et al 0.8% [1]. Also they reported a positive correlation of cervical
spine injury with motor vehicle accident and attributed to the
greater impact force to the face that is eventually transmitted to
the neck or a direct force to the neck. This can be explained by
the unfavourable hyper-flexion or hyperextension of the neck in
such sudden trauma that can potentially cause a cervical spine
injury [13]. This is supported by Robertson et al, as they reported
the higher prevalence of these injuries in motor vehicle accidents
than the others and thoracic or lumbar spine was involved more
next to cervical spine. Patients at risk for cervical spine injuries included
those sustaining blunt craniofacial trauma or multisystem
trauma, fall from heights or high impact injury to clavicle. Patients
may or may not be symptomatic. Though the association is much
lesser in proportion, any case of maxillofacial trauma should be
suspected to have concomitant cervical spine injury unless proven
otherwise. In case the patient presents with symptoms, it is wise to
rule out the presence of injury before proceeding to the secondary
survey of maxillofacial injury.
Hackl et al., reported that the risk to sustain additional cervical
spine injuries in facial trauma increases every year by 1.7%5. Also
a threefold increase in the risk of sustaining these injuries was
inferred in road traffic accidents than other aetiologies of trauma.
Again if there occurs a concomitant traumatic brain injury due to
the trauma, the risk still rises by two fold. Hence it is expected of
a maxillofacial surgeon to be aware of such emergency conditions
and the importance of the timely catch because unlike facial trauma
that presents with obvious symptoms, cervical spine injuries
don’t display any pathognomonic signs. A higher chance of missing
it is evident especially if injuries to other systems dominate. A
significant correlation was observed with the prevalence of cervical
spine injuries and the type of maxillofacial fractures. 3.6% of
the total 5.6% prevalence of c-spine injuries was associated with
hard tissue injuries of the maxillofacial region. Patients sustaining
fractures to the facial skeleton were found to have significant
concomitant cervical spine injuries (p<0.000), when compared to
the soft tissue injuries though there was prevalence of c-spine
injuries in the latter also. This could be attributed to the transfer
of the higher magnitude of forces causing the fractures of facial
skeleton, type of the fractures, and mechanism of trauma which
is more complex in hard tissue injuries than the soft tissue injuries.
When the spectrum of prevalence was studied in the hard
tissue injuries, it was found that about 9.3% of the population
sustaining maxillofacial fractures had added c-spine injuries which
were statistically significant (p<0.000). A positive correlation was
found between the increasing complexity of facial fractures and
the associated c-spine injuries in our study. 2% of association was
found with pan facial fractures, 3.4% with combined multiple
mandibular and mid-third of face fractures, 1.4% with isolated
mandibular fractures, 1.1% with ZMC fractures and 0.2% with
isolated maxillary fractures. Similar spectrum of association and
prevalence was reported by Reich et al., in their study. But there
exists controversy regarding the correlation of c-pine injuries to
that of the type of fracture. While Merrit et al, Hackl et al, Bayles
[6] et al., reported a positive correlation with mandibular fractures,
Babcock et al reported it to be middle third of face fractures
[7]. Interestingly Bonanthaya [8] et al., reported a model of
association, where they reported that mandibular fractures were
associated with upper cervical spine injuries while middle third of
face fractures were associated with lower cervical spine fractures.
In our study there was no significant association observed with
the type of fracture and c-spine injuries.
In patients with suspected cervical spine injury, mobilization of
the neck should not be attempted during the maxillofacial examination
[10]. Meticulous examination should be done to identify
the presence of local pain, ecchymosis overlying the fracture, contour
deformity, oedema, and spasm of the neck muscles. Patients
who are asymptomatic, alert and present no sensorimotor deficits
on examination of the c-spine should be cleared with routine xray
depicting all the seven cervical vertebrae. In patients with any
of the symptoms and suspected to have sustained injury to the
spine, a Computed Tomography of the region is preferred. But
when associated with maxillofacial injuries, this poses a challenge
during the procedure. Immobilization with cervical collar should
be done prior to imaging. Magnetic Resonance Imaging (MRI) is
preferred if disco ligamentous lesions or sensorimotor deficits are
suspected [2].
Thus the maxillofacial surgeons should be aware of the risks of
underestimating blunt cervical injuries during their initial assessment
of patients sustaining maxillofacial trauma. Knowledge of
these associated injuries provides useful strategies for patient care and prevention of further complications. This also calls for multidisciplinary
interdepartmental approach in managing a patient
sustaining maxillofacial trauma than considering it an isolated entity.
Conclusionn
Proper guidelines should be followed during the primary and secondary
survey of maxillofacial region post trauma, to rule out the
prevalence of associated cervical spine injuries. Though reported
incidence is low, underestimation of these injuries could lead to
significant morbid states as management of the facial fractures
essentially involves manipulation of neck that might increase the
chances of worsening the situation further. Proper immobilization
of the neck especially in unconscious patients should be done
until the spine is cleared of injuries. A collaborated approach by
team of emergency physicians, maxillofacial surgeons, neurosurgeons,
anaesthesiologists and orthopaedic surgeons should be followed
in managing a polytrauma patient.
References
- Roccia F, Cassarino E, Boccaletti R, Stura G. Cervical spine fractures associated with maxillofacial trauma. J. Craniofac. Surg. 2007 Nov 1;18(6):1259- 63.
- Reich W, Surov A, Eckert AW. Maxillofacial trauma - Underestimation of cervical spine injury. J Craniomaxillofac Surg. 2016 Sep;44(9):1469-78. Pubmed PMID: 27527678.
- Rogers WA. Fractures and dislocations of the cervical spine. J Bone Joint Surg Am 1957;39:341-376.
- Advanced Trauma Life Support Course for Physicians Student Manual. Chicago, IL: American College of Surgeons, 1997
- Hackl W, Hausberger K, Sailer R, Ulmer H, Gassner R. Prevalence of cervical spine injuries in patients with facial trauma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001 Oct 1;92(4):370-6.
- Bayles SW, Abramson PJ, McMahon SJ, et al. Mandibular fracture and associated cervical spine fracture, a rare and predictable injury. Arch Otolaryngol Head Neck Surg 1997; 123:1304Y1307.
- Babcock JL. Cervical spine injuries: diagnosis and classification. Arch. Surg. 1976 Jun 1;111(6):646-51.
- Lalani Z, Bonanthaya KM. Cervical spine injury in maxillofacial trauma. Br J Oral Maxillofac Surg. 1997 Aug 1;35(4):243-5.
- Fama F, Cicciu M, Sindoni A, Nastro-Siniscalchi E, Falzea R, Cervino G, et al. Maxillofacial and concomitant serious injuries: An eight-year single center experience. Chin J Traumatol. 2017 Feb;20(1):4-8.Pubmed PMID: 28209449.
- Delcourt T, Bégué T, Saintyves G, Mebtouche N, Cottin P. Management of upper cervical spine fractures in elderly patients: current trends and outcomes. Injury. 2015 Jan;46 Suppl 1:S24-7.Pubmed PMID: 26528937.
- Mukherjee S, Abhinav K, Revington PJ. A review of cervical spine injury associated with maxillofacial trauma at a UK tertiary referral centre. Ann R Coll Surg Engl. 2015 Jan;97(1):66-72.Pubmed PMID: 25519271.
- Mulligan RP, Mahabir RC. The prevalence of cervical spine injury, head injury, or both with isolated and multiple craniomaxillofacial fractures. PlastReconstrSurg. 2010 Nov 1;126(5):1647-51.
- McGoldrick DM, Fragoso-Iñiguez M, Lawrence T, McMillan K. Maxillofacial injuries in patients with major trauma. Br J Oral Maxillofac Surg. 2018 Jul 1;56(6):496-500.
- Patil SG, Munnangi A, Joshi U, Thakur N, Allurkar S, Patil BS. Associated Injuries in Maxillofacial Trauma: A Study in a Tertiary Hospital in South India. J Maxillofac Oral Surg. 2018 Dec;17(4):410-416.Pubmed PMID: 30344378.