Rapidly Progressive Multicentric Castleman’s Disease in Patient with Acute Retroviral Syndrome:A Case Report
Hassan A*, Carroll C, Espina T
Advocate Illinois Masonic Medical center, Chicago, USA.
*Corresponding Author
Abdalla Hassan, MD,
Internal Medicine Resident,
Internal Medicine Department, 7th floor
Advocate Illinois Masonic Medical Center, 836 W Wellington Ave,
Chicago, IL 60657, USA.
Tel: +1-347-873-2073
E-mail: abdalla.hassan@advocatehealth.com
Received: April 06, 2015; Accepted: April 29, 2015; Published: May 05, 2015
Citation: Hassan A, Carroll C, Espina T (2015) Rapidly Progressive Multicentric Castleman’s Disease in Patient with Acute Retroviral Syndrome: A Case Report. Int J AIDS Res. 02(4), 34-36. doi: dx.doi.org/10.19070/2379-1586-150007.
Copyright: Hassan A© 2015. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Multicentric Castleman’s Disease (MCD) is a lymphoproliferative disorder that happens more in Human Herpes Virus-8 (HHV-8) positive HIV patients. We are reporting a unique case of rapidly progressive Multicenteric Castleman’s disease in patient with acute retroviral syndrome. We are presenting a 40 year old male presented with fevers, chills and syncope. He was recently diagnosed with HIV. On presentation he was febrile. Physical examination demonstrated cervical lymphadenopathy with hepatosplenomegaly. His labs were significant for pancytopenia and hyponatremia. A working diagnosis of acute retroviral syndrome was made, although the anemia was too severe to be due to HIV only. He received blood transfusion, but the hemoglobin showed minimal improvement. CTAbdomen/pelvis was done and showed hepatosplenomegaly with enlarged lymph nodes. Lymph node biopsy was consistent with HHV-8 associated MCD. Accordingly, he was started on Anti-Retroviral Therapy for HIV and Gancyclovir and Rituxamab for MCD. Two days later, he continued to deteriorate and his blood counts dropped requiring multiple units of transfusion. Consequently, he developed severe respiratory distress, ventilated, and then he expired. In conclusion, we believe that occurrence of Castleman’s disease in acute HIV patients before ART initiation is a poor prognostic sign and physicians should be aware of such entity.
2.Introduction
3.Case Presentation
5.Discussion
6.Conclusion
7.References
Keywords
Multicentric Castleman’s Disease; Acute Retroviral Syndrome; Anti-Retroviral Therapy.
Introduction
Multicenteric Castleman’s Disease (MCD) or angiofollicular dysplasia is a lymphoproliferative disorder that happens with increased frequency in Human Herpes Virus-8 (HHV-8) positive HIV patients. HHV-8 also causes Kaposi sarcoma and primary effusion lymphoma, and it is responsible for around 50% of MCD cases. We present a very unique case of rapidly progressive Multicenteric Castleman’s Disease in newly diagnosed HIV positive male with acute retroviral syndrome before the initiation of Anti- Retroviral Therapy (ART).
Case Presentation
A 40 year old homosexual male presented to our institution with fevers, chills and a syncopal episode. He has a past medical history of hypertension and illicit drug use. He was originally seen at an outside clinic for anal pain and was diagnosed with HIV five days prior to his admission. Two weeks prior to his admission he had also experienced an episode of syncope, followed by 5 days of fever and chills and diffuse body aches. He also reported having a negative HIV test 2 months earlier. On presentation to emergency department he was not in acute distress, febrile with a temperature of 101ºF (38.3 ºC), tachycardic (max HR= 110) and normotensive.Physical examination demonstrated right sided non tender cervical lymphadenopathy with hepatosplenomegaly. His labs were significant for pancytopenia (WBC of 4.1 thousand/mcL; HgB 6.1gm/dL; MCV82fL; Platelet 78 thousand/mcL), hyponatremia (131mmol/L), and elevated creatinine (1.5mg/dL). Chest X-Ray was not impressive.
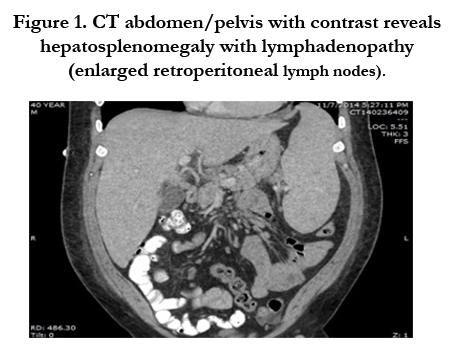
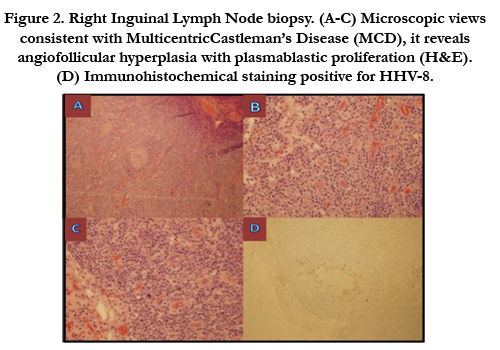
At that time the working diagnosis was acute retroviral syndrome given his symptoms and lab findings, although the anemia was too severe to be due to HIV only. Immediately he was transfused 2 units of Packed Red Blood Cells. His repeat Hemoglobin showed minimal improvement despite transfusion and this was very unusual in case of acute retroviral syndrome. Haptogoblin and bilirubin were normal. Peripheral blood smear showed spherocytosis and iron studies were significant for anemia of chronic disease. Later that day Computed Tomography of Abdomen and Pelvis was done and it was significant for hepatosplenomegaly with multiple enlarged retroperitoneal lymph nodes in the abdomen and pelvis (Figure 1). Based on these findings and the overall clinical picture, lymph node biopsy was obtained and it was consistent with HHV-8 associated Multicentric Castleman’s disease (MCD) (Figure 2). At that stage he was started on Anti-Retroviral Therapy for HIV with Gancyclovir and Rituxamab for MCD.
Figure 1. CT abdomen/pelvis with contrast reveals hepatosplenomegaly with lymphadenopathy (enlarged retroperitoneal lymph nodes).
Figure 2. Right Inguinal Lymph Node biopsy. (A-C) Microscopic views consistent with MulticentricCastleman’s Disease (MCD), it reveals angiofollicular hyperplasia with plasmablastic proliferation (H&E). (D) Immunohistochemical staining positive for HHV-8.
Two days later, he continued to deteriorate and his hemoglobin continued to drop requiring multiple units of blood transfusion. His platelets continued to drop, and three days after that developed severe respiratory distress resulting in transfer to Medical Intensive Care Unit (MICU). On the second day in the MICU, patient platelet count dropped to less than 10 and transfused multiple units of platelets. Next day he was ventilated due to severe Acute Respiratory Distress Syndrome, and one day after that he expired.
Discussion
Castleman's disease is a benign disorder first described by Dr. Benjamin Castleman in 1956. Castleman's disease is also referred to as angiofollicular hyperplasia, and is non-clonal disease of the lymphnodes. The usual presentation is with lymphadenopathy and systemic symptoms including fever, night sweats, and weight loss. The disease commonly involves spleen, liver, lymph nodes (abdominal and peripheral) [1]. In individuals infected with HIV, Multicentric Castleman’s Disease (MCD) is almost exclusively caused by infection with a HHV-8 {which is also known as Kaposi sarcoma-associated herpesvirus (KSHV)}. This may be considered a separate entity from the non-HHV8 related or idiopathic form of multicentric Castleman’s disease and from unicentric forms of Castleman’s disease.
Several case reports have associated the development of MCD with the initiation of Anti-Retroviral Therapy (ART) [2]. The exact pathophysiology of MCD is still controversial, with IL-6 playing a major role in immune disruption and hypergammaglobulinemia [3]. It is postulated that it arises from immune dysregulation secondary to immune reconstitution syndrome and intrinsic properties of HHV-8 which allows for virally-encoded secretion of IL-6 [4]. Thus, though rare, the historical incidence has since been noted to be on the rise as more patients are started on ART [5].
The case that has been presented above is a deviation from usual natural history of the development of MCD. An observational study done by Katchanov et al. has described that the temporal relationship has been described to occur within the 12 months of ART initiation [6]. Our patient presented was noted to have inguinal lymphadenopathy with hepatosplenomegaly on admission before the initiation of antiretroviral therapy. He was not started on HAART before the lymph node biopsy was done. He was subsequently started on HAART, but continued to have more progressive symptoms and eventually succumbed to his disease.
Rapidly progressive MCD has been historically associated to the initiation of antiretroviral therapy. Our case suggests that other pathological pathways exist in the development of MCD. There are no case reports to date that demonstrated such a presentation of rapidly progressive Multicentric Castleman’s Disease in acute retroviral syndrome.
Conclusion
In conclusion, we believe that the occurrence of Castleman’s disease in patients with acute HIV before the initiation of ART is a very poor prognostic sign and physicians should be aware about such entity.
References
- Roberto N. Miranda MD, Joseph D. Khoury MD, L. Jeffrey Medeiros MD (2013) Multicentric Castleman Disease. Atlas of Anatomic Pathology 111-113.
- Zietz C, Bogner JR, Goebel FD, Löhrs U (1999 ) An unusual cluster of cases of Castleman's disease during highly active antiretroviral therapy for AIDS. N Engl J Med 340(24): 1923-4.
- Al-Maghrabi JA (2011) Castleman's disease. Update on pathogenesis. Saudi Med J 32(5): 451-8.
- Staskus KA, Sun R, Miller G, Racz P, Jaslowski A, et al. (1999) Cellular tropism and viral interleukin-6 expression distinguish humanherpesvirus 8 involvement in Kaposi's sarcoma, primary effusion lymphoma, andmulticentricCastleman's disease. J Virol 73(5): 4181-7.
- Casper C (2005) The aetiology and management of Castleman disease at 50 years:translating pathophysiology to patient care. Br J Haematol 129(1):3-17.
- Katchanov J, Zimmermann U, Branding G, Arastéh K, Müller M (2014) HIV-associatedmulticentricCastleman's disease after initiation of antiretroviral therapy:experience of a European centre. Infection 42(4): 791-3.