Anaesthesia and Analgesia Methods Applied in Thoracic Surgery
Onur Karaca, Semih Başkan, Gülçin Alay, Dilşen Örnek*, Vildan Taşpınar, Bayazit Dikmen
Department of Anesthesia and Reanimation, Ankara Numune Education and Research Hospital, Ankara, Turkey.
*Corresponding Author
Dilsen Ornek,
Department of Anesthesia and Reanimation,
Ankara Numune Education and Research Hospital,
Ankara, Turkey.
Tel: 05057373828
E-mail: dilsenpinar@yahoo.com
Received: November 29, 2016; Accepted: December 15, 2016; Published: December 17, 2016
Citation: Onur Karaca, Semih Başkan, Gülçin Alay, Dilşen Örnek, Vildan Taşpınar, Bayazit Dikmen (2015) Anaesthesia and Analgesia Methods Applied in Thoracic Surgery. Int J Anesth Res. 4(12), 368-372. doi: http://dx.doi.org/10.19070/2332-2780-1600076
Copyright: Dilşen Örnek© 2016. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Aim: To determine the anaesthesia and analgesia methods applied in thoracic surgery in our clinic and to evaluate these with current literature.
Method: A retrospective evaluation was made of patients who underwent surgery in the Chest Surgery Clinic of Ankara Numune Training and Research Hospital in the period January 2011-2014. The demographic data of patients, the operation applied, the anaesthetic and analgesic agents used, monitorisation and complications which occurred perioperatively were obtained from anaesthesia notes and computer records and were recorded on scanning forms with many variables.
Results: Following the scanning of the study, the data of 210 patients were accesssed. No statistical difference was determined in respect of the demographic data of the patients. The most frequent operations were found to be thoracotomy (n=103) and bronchoscopy (n=85). Benzodiazepine was used in all groups and patients. In almost all groups, propofol was found to be the most preferred agent for intravenous inducton. Vercuronium and rocuronium were the most frequently applied muscle relaxant agent, sevoflurane was generally selected as the inhalation agent and was applied with a mixture of air and oxygen. In addition to the application of standard monitorisation, in major operations such as thoracotomy where central and arterial entrance was made, contramal was used as postoperative analgesia and in thoracotomy operations, the selection of thoracic epidural route and patient-controlled analgesia was determined to be statistically significant. Postoperative complications developed in 8 patients, there was ventilator requirement in 13 patients and 53 patients were followed up in the intensive care unit in the postoperative period.
Conclusion: Although the number of patients admitted for thoracic surgery in our study was low, it can be said that it was attempted to reach current standards in the application of anaesthesia and analgesia. Taking the experience of each anaesthesia clinic in thoracic surgery and the standards of the centre into consideration, there is a need for a clinic-specific anaesthesia and analgesia strategy to be developed with the aid of scientific studies.
2.Introduction
3.Method
4.Results
5.Discussion
6.Conclusion
7.References
Keywords
Thoracic Surgery; Anaesthesia; Analgesia.
Introduction
The general heading of thoracic surgery encompasses bronchocopy, thorascopy, mediastinoscopy, lung resections, pleura, diaphragm and chest wall surgery, tracheo-bronchial surgery, mediastinal surgery (including thymectomy, myastenia gravis, retrosternal goitre), oesophagus surgery, pulmonary thromboembolectomy, aorta, heart surgery and lung transplantation [1-6]. In patients who are to undergo thoracic surgery, it is important that the pre-anaesthesia evaluation is applied thoroughly, that when necessary, invasive monitorisation is provided additional to noninvasive monitorisation, that the appropriate anaesthetic agent is selected, appropriate mechanical ventilation (MV) and fluid support is provided, one-lung ventilation (OLV) is applied when necessary and that sufficient postoperative analgesia is provided. In these cases, the primary responsibiliity of the anaesthetist is to define the pre-operative risks, provide the optimal conditions preoperatively and plan appropriate anaesthesia [1-6].
It must be determined whether or not the patient will be able to tolerate a planned lung resection before anaesthesia is applied. The majority of lung operations are performed in the lateral decubitus position and generally, while ventilation of the lower lung continues, it is necessary to apply OLV to the operated lung because of the possibility of collapse. The aims of OLV application are to provide sufficient oxygenation and CO2 elimination, while at the same time reducing the side-effects of mechanical ventilation on the airway and haemodynamics and to provide appropriate operation conditions [1-6]. Not providing sufficient postoperative analgesia causes postoperative atelectasis, limited expansion in inspiration in the thoracic cage and reduced patient comfort.
In the light of this knowledge, this study aimed to evaluate the anaesthetic and analgesic methods applied in thoracic surgery in our clinic.
Method
Approval for the study was granted by the Ethics Committee of Ankara Numune Training and Research Hospital. A retrospective examination was made of the records of patients who underwent surgery in the Chest Surgery Clinic between January 2011 and January 2014. The demographic data of the patients, concomitant diseases, ASA scores, medications used, anaesthesia and postoperative analgesia methods applied, duration of anaesthesia, and perioperative complications were evaluated. The data related to the patients were obtained from the pre-operative evaluation forms, anaesthesia observation notes and hospital computer records and were recorded on multi-variable scanning forms.
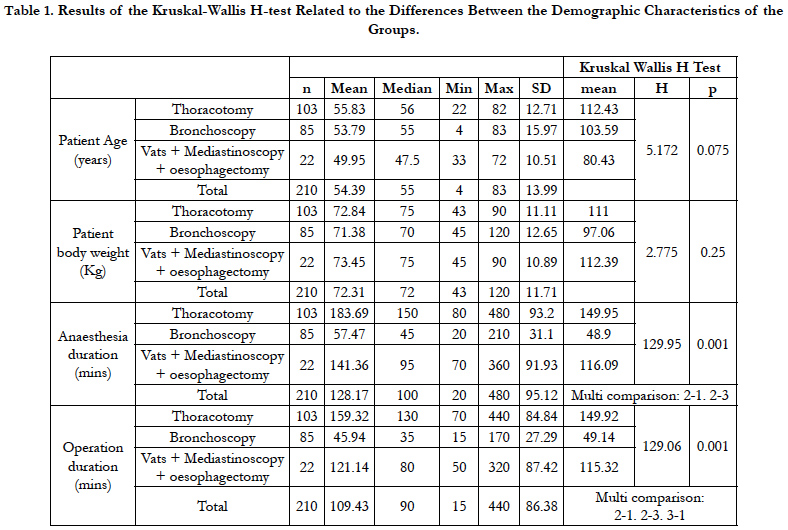
The data obtained in the study were analysed with SPSS v. 20 software. The Shapiro Wilks test was used because of the number of units when examining the normal distribution of the variables. In the examination of the differences between groups with normal distribution of the variables, the One-Way ANOVA test was applied and for those not with normal distribution, the Kruskal- Wallis H-test. When significant differences were determined with the Kruskal-Wallis H-test, the post-hoc multiple comparison test was applied to ascertain which groups were different. When the relationships between the groups of nominal variables were examined, Chi-square analysis was applied. Pearson Chi-square analysis was applied with Monte Carlo simulation in the RxC tables. A value of p < 0.05 was accepted as statistically significant.
Results
The data of 210 patients were accessed. No statistical difference was determined in respect of the demographic data of the patients (p > 0.05). The demographic data of the patients are shown in Table 1. The most frequent operations were found to be thoracotomy (n=103) and bronchoscopy (n=85). The mean operation time of thoracotomy was determined as 159.32 ± 84.84 mins, which was longer than for other operations.
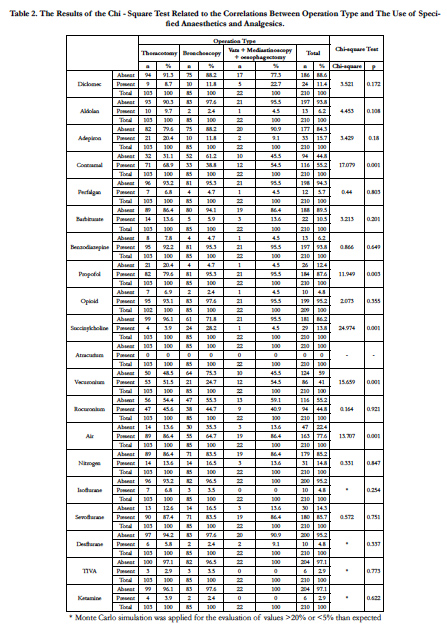
No relationship was determined between the Mallampati and ASA scores and the operation type. The ASA II group included 66.5% of patients and ASA III, 25.7%. Benzodiazepine was used in all groups and patients. In almost all groups, propofol was found to be the most preferred agent for intravenous induction. Vercuronium and rocuronium were the most frequently applied muscle relaxant agent, sevoflurane was generally selected as the inhalation agent and was applied with a mixture of air and oxygen. TIVA was determined to have been rarely applied. In addition to the application of standard monitorisation, in major operations such as thoracotomy where central catheterisation and invasive blood pressure monitoring was applied, contramal was used as postoperative analgesia and in thoracotomy operations, the selection of thoracic epidural route and patient-controlled analgesia was determined. In thoracotomy and oesophagectomy operations, intubation was provided with a double lumen tube and OLV could have been applied. Postoperative complications developed in 8 patients, there was ventilator requirement in 13 patients and 53 patients were followed up in the intensive care unit in the postoperative period Table 2.
A statistically significant relationship was determined between operation types and the use of contramal (p < 0.05). The use of contramal was seen in 68.9% of thoracotomy operations, in 38.8% of bronchoscopy operations and in 54.5% of Vats, mediastinoscopy and oesophagectomy operations.
A statistically significant relationship was determined between operation types and the use of propofol (p < 0.05). The use of propofol was seen in 79.6% of thoracotomy operations, in 95.3% of bronchoscopy operations and in 95.5% of Vats, mediastinoscopy and oesophagectomy operations.
A statistically significant relationship was determined between operation types and the use of succinylcholine (p < 0.05). The use of succinylcholine was seen in 3.9% of thoracotomy operations, in 28.2% of bronchoscopy operations and in 4.5% of Vats, mediastinoscopy and oesophagectomy operations.
A statistically significant relationship was determined between operation types and the use of vecuronium (p<0.05). The use of vecuronium was seen in 51.5% of thoracotomy operations, in 24.7% of bronchoscopy operations and in 54.5% of Vats, mediastinoscopy and oesophagectomy operations.
A statistically significant relationship was determined between operation types and the use of air (p < 0.05). The use of air was seen in 86.4% of thoracotomy operations, in 64.7% of bronchoscopy operations and in 86.4% of Vats, mediastinoscopy and oesophagectomy operations.
No analysis was made of the relationship between operation type and atracurium as there were no data.
No statistically significant relationship was determined between the use of other analgesics and anaesthetics and operation type (p > 0.05).
Discussion
In this study, the information of 210 patients was able to be accessed and evaluated. The findings of the study and the methods applied in our clinic can be considered to conform to current applications. Although the main reason for this is that our hospital is not a private hospital for thoracic surgery, that there were no difficulties in accessing data sources can also be included in the reasons.
Advances in anaesthesia methods and monitorisation methods, lung isolation techniques which have been developed and the intensive care services presented, have increased the success rates of surgery on patients who were previously accepted as inoperable. In addition, the possibility of operating on patients with severely impaired pulmonary function is higher compared to the past and therefore, a higher incidence of gas exchange abnorabnormalities can be expected [7, 8]. In current thoracic surgery applications, despite advances in anaesthesia, including the use of epidural anaesthesia, in surgical techniques and in perioperative care, pulmonary complications continue to be the leadng causes of morbidity and mortality [4, 5]. Major respiratory complications such as atelectasis, pneumonia and respiratory failure have been reported to develop in 15%-20% of patients and to be responsible for the majority of mortality at rates of 3%-4% [9].
Higher rates of postoperative mortality are seen together with the development of pulmonary complications. Similarly, postoperative pulmonary complications have been reported in 15%-40% of patients undergoing oesophagectomy. The reasons for this high risk in oesophagectomy patients are multi-factorial, including surgical entry into two separate body cavities, impaired bronchial innervation and lymphatic circulation, diaphragm dysfunction, and disruption to the swallowing co-ordination and insufficient protection of the airway because of recurrent laryngeal nerve damage [9].
Recent innovations and monitorisation possibilities allow onelung ventilation (OLV) to be applied under safer conditions and aid the reduction of complications. Several reasons (blood transfusion, elevated creatinine, low preoperative FEV1) for delayed postoperative extubation are difficult factors not taken into consideration, but are factors which can be modified by the application of thoracic epidural analgesia. These aplications have a noticeable value in reducing the requirement for post-thoracotomy- associated mechanical ventilator and intensive care [10]. Postoperative prophylactic CPAP (5-7 cm H2O) applied to patients who have undergone pulmonary surgery has been shown to increase the PaO2/FiO2 ratio [11].
In the current study, although postoperative complications developed in 8 patients, ventilator requirement in 13 patients and 53 patients were followed up in the intensive care unit in the postoperative period, generally the reasons for these were seen to be surgical bleeding and respiratory failure.
A significant level of irregularity in gas exchange is the reason for OLV and hypoxemia may develop due to increased intrapulmonary shunt. Postoperative pulmonary dysfunction following video-assisted thorascopic surgery (VATS) procedures has been seen to occur less frequently compared to the number of cases observed following thoracotomy. In a comparison made of lobectomy applied to patients with thoracotomy and lobectomy applied to patients with VATS, on both the 7th and the 14th day postoperatively, the postoperative PaO2, O2 saturation, peak flow rates, forced expiratory volume at 1 second (FEV1) and forced vital capacity (FVC) were seen to be better in the patients who had undergone the VATS procedure [12]. In addition to the type of operation, the application of anaesthesia is important and at the moment of transfer from denitrogenisation (use of oxygen and air mixture) of double lung ventilation in these operations to OLV, it has been determined that the surgical conditions improve [13]. In our hospital, lobectomy operations are generally applied with thoracotomy and O2/air mixture is used in anaesthesia.
The findings of recent studies have shown that OLV provides safer conditions. Recent studies have stated that for the application of high FiO2 and CPAP to a deflated lung, OLV is necessary and should be the frst treatment in desaturation. In our clinic, when destauration is observed, OLV is transferred to double lung ventilation, the tube is cleaned of secretions and the O2 concentration is increased [14].
In a prospective, randomised, controlled, clinical study of patients with OLV in thoracic surgery, it was shown that the postoperative complication rate decreased and the expressed inflammatory mediators were reduced by a noticeable level with the use of the volatile anaesthetic, sevoflurane [15]. In our clinic, it was determined that generally sevoflurane is used as the inhalation anaesthetic in thoracic surgery.
Postoperative analgesia is also of importance in these operations. This issue remains current and various studies are ongoing. Thoracic epidural analgesia (TEA) is still seen as the gold standard. As TEA has a positive effect on ventilation mechanics by strengthening the inspiratory respiratory muscle strength, it can be safely used on advanced stage COPD patients [16].
However, research into alternative analgesia methods is ongoing. In a previous study, a comparison was made of the effects on the efficacy of analgesia, complication rates and mortality of thoracic epidural catheter and paravertebral block in thoracic surgery. Although it could be said that the postoperative side-effects of paravertebral block were lower in the short-term, it was reported that the long-term effects on complications and mortality should be investigated [17].
In our clinic, the thoracic epidural analgesia method was preferred in thoracic surgery. When the application was not successful, intercostal block or intravenous patient-controlled analgesia methods were applied.
Conclusion
Although the number of patients admitted for thoracic surgery was low and therefore there was limited experience of our clinic in the applications of anaesthesia and analgesia, the protocols followed can be seen to be consistent with the knowledge in curent literature.
Thoracic surgery threatens or directly disrupts the natural structure of the respiratory and circulatory system both anatomically and physiologically, thus causing an increase in perioperative and postoperative morbidity and mortality. Therefore, there can be considered to be a need for anaesthesia and analgesia management strategies to be developed for anaesthesia clinics in this type of surgery, taking into consideration the experience and standards of the centre and the features of the applications of anaesthesia and analgesia.
References
- Datta D, Lahiri B (2003) Preoperative evaluation of patients undergoing lung resection surgery. Chest. 123: 2096-103.
- Brunelli A, Kim AW, Berger KI, Addrizzo-Harris DJ (2013) Physiologic evaluation of the patient with lung cancer being considered for resectional surgery: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 143(5): e166S-90S.
- Brodsky JB, Fitzmaurice B (2001) Modern Anesthetic Techniques for Thoracic Operations. World J Surg. 25: 162-6.
- Banki F (2010) Pulmonary assessment for general thoracic surgery. Surg Clin North Am 90(5): 969-84.
- Bernstein WK, Deshpande S (2008) Preoperative evaluation for thoracic surgery. Semin Cardiothorac Vasc Anesth. 12(2): 109-21.
- Stephan F, Boucheseiche S, Hollande J, Bonnet F, Cheffi A, et al., (2000) Pulmonary complications following lung resection: a comprehensive analysis of incidence and possible risk factors. Chest 118(5): 1263-70.
- Wilson WC, Benumof JL (2010) Anesthesia for thoracic surgery (Toraks Cerrahisinde Anestezi). Miller Anestezi, Miller RD, (6th Edn), (Çeviri editörü: Aydın D) baskı. İzmir: Güven Kitapevi. 1847-939.
- Morgan GE, Mikhail MS, Murray MJ (2000) Anestesia for thoracic surgery. Clinical Anesthesiology. (4th Edn), New York: Lange Medical Books / The McGraw-Hill. 525-51.
- Gockel I, Exner C, Junginger T (2005) Morbidity and mortality after esophagectomy for esophageal carcinoma: a risk analysis. World J Surg Oncol. 3: 37.
- Cywinski JB, Xu M, Sessler D, Mason D, Koch CG (2009) Predictors of prolonged postoperative endotracheal intubation in patients undergoing thoracotomy. J Cardiothorac Vasc Anesth. 23(6): 766-9.
- Garutti I, Puente-Maestu L, Laso J, Sevilla R, Frias I, et al., (2014) Comparison of gas exchange after lung resection with a Boussignac CPAP or Venturi mask. Br J Anaesth. 112: 929-35.
- Nakata M, Saeki H, Yokoyama N, kurita A, Takiyama W (2000) Pulmonary function after lobectomy: videoassisted thoracic surgery versus thoracotomy. Ann Thorac Surg. 70: 938-41.
- Ko R, McRae K, Darling G, Waddell TK, McGlade D, et al., (2009) The Use of Air in the Inspired Gas Mixture During Two-Lung Ventilation Delays Lung Collapse During One-Lung Ventilation. Anesth Analg. 108(4): 1092-6.
- Lumb A, Slinger P (2015) Hypoxic pulmonary vasoconstriction, physiology and anesthetic implications. Anesthesiology. 122: 932-46.
- De Conno E, Steurer MP, Wittlinger M, Urner M, Neff TA, et al., (2009) Anesthetic-induced improvement of the inflammatory response to one-lung ventilation. Anesthesiology. 110(6): 1316-26.
- Gruber EM, Tschernko EM, Kritzinger M, Deviatko E, Wisser W, et al., (2001) The effects of thoracic epidural analgesia with bupivacaine 0.25% on ventilatory mechanics in patients with severe chronic obstructive pulmonary disease. Anesth Analg. 92(4): 1015-9.
- Powell ES, Cook D, Pearce AC, Davies P, Gao F, et al., (2011) A prospective, multicenter, observational cohort study of analgesia and outcome after pneumonectomy. Br J Anaesth . 106(3): 364-70.