A Study Of Comparison Of 0.8mg Vs 1.4mg Of Intrathecal Nalbuphine In 3.5ml Of Inj. Bupivacaine Heavy 0.5% In Lower Abdominal And Lower Limb Surgeries
Mohan1, Shridhar Ekbote2*, Ramesh Babu2
1 Assistant Professor, Department of Anesthesia. Navodaya Medical College, Raichur. Karnataka, India.
2 Associate Professor, Department of Anesthesia. Navodaya Medical College, Raichur. Karnataka, India.
*Corresponding Author
Dr. Shridhar Ekbote,
Associate Professor, Department of Anesthesia,
Navodaya Medical College, Raichur. Karnataka, India.
Tel: 9900387878
E-mail: Sridhar.ekbote9@gmail.com
Received: March 18, 2018; Accepted: April 27, 2018; Published: April 30, 2018
Citation: Mohan, Shridhar Ekbote, Ramesh Babu. A Study Of Comparison Of 0.8mg Vs 1.4mg Of Intrathecal Nalbuphine In 3.5ml Of Inj. Bupivacaine Heavy 0.5% In Lower Abdominal And Lower Limb Surgeries. Int J Anesth Res. 2018;6(3):515-519. doi: dx.doi.org/10.19070/2332-2780-18000103
Copyright: Shridhar Ekbote© 2018. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Spinal anaesthesia is a commonly employed technique which provides safe, effective, low cost surgical anesthesia with good post-operative analgesia. Nalbuphine is a semi synthetic opioid with mixed antagonist and k agonist properties. In present study we have compared 0.8mg vs 1.4mg of Intrathecal inj. Nalbuphine with inj. bupivacaine heavy 0.5% 3.5cc to determine the most optimal dose for effective anaesthesia and maximum postoperative analgesia in lower abdominal surgeries. We also observed about the common side effects that occur with opioids like, pruritus, nausea, vomiting, sedation.
Material and Methods: Patients were randomly allocated into two groups of 30 participants each. They received either nalbuphine 0.8 mg (group A) or nalbuphine 1.4 mg (group B) diluted upto 0.5ml with normal saline, mixed with 17.5 mg of hyperbaric bupivacaine 0.5% (3.5 ml). The onset of sensory blockade, onset of motor blockage, duration of sensory blockade, two-segment regression time from highest level of sensory blockade and duration of motor blockade were recorded following procedure.
Results: In this study, we found that intrathecal injection Nalbuphine combined with intrathecal bupivacaine provides faster onset of sensory and motor blockage along with intraoperative hemodynamic stability. Addition of 1.4 mg intrathecal Nalbuphine in comparison with 0.8 mg provides better postoperative analgesia. The duration of sensory and motor blockade were increased without significantly increasing the incidence of side effects such as sedation, pruritus, nausea/vomiting and respiratory depression.
Conclusion: In conclusion, Intrathecal Nalbuphine (1.4mg) added to Intrathecal Bupivacaine 0.5% heavy (17.5mg) provides prolonged postoperative analgesia without increasing risk of side effects. Further studies are required to determine optimal dosage of intrathecal Nalbuphine.
2.Introduction
3.Materials and Methods
4.Results
5.Discussion
6.Conclusion
7.References
Keywords
Spinal Anaesthesia; Nalbuphine; Bupivacaine Analgesia.
Introduction
Spinal anaesthesia is a very commonly used anaesthesia technique for various lower abdominal and lower limb surgeries. This approach has various advantages like cost effectiveness, better performance, enhanced margin of safety, and also helps in providing good post-operative analgesia. The stress response associated with general anaesthesia and side effects of various drugs used for general anaesthesia were also blunted. Various adjuvants including opioids, have been used with local anaesthetics in spinal anaesthesia to reduce complications as well as to increase peri and postoperative analgesia. Nalbuphine is a semi synthetic opioid with mixed antagonist and k agonist properties [1, 2]. Previous studies have shown that Intrathecal administration of Nalbuphine produced a significant analgesia accompanied by minimal pruritis and respiratory depression. Various doses of Nalbuphine were tried but still there is a controversy about the most effective dose. In present study we have compared 0.8mg VS 1.4mg of Intrathecal inj. Nalbuphine with inj. bupivacaine heavy 0.5% 3.5cc to establish the most effective dose for maximum postoperative analgesia in lower abdominal and lower limb surgeries. We also observed the common side effects that occur with opioids like, pruritus, nausea, vomiting, sedation and respiratory depression.
Materials and Methods
The study was approved by the local institutional ethics committee and written informed consent was obtained from all patients before participation. Sixty patients with ASA physical status I or II, aged 20-60 years, weighing 40- 80 kgs, scheduled for elective lower abdominal and lower limb surgeries, of duration less than 2 hrs, under subarachnoid block, were included in the study. Patients were randomly allocated to one of two groups. They received either nalbuphine 0.8 mg (group A) or nalbuphine 1.4 mg (group B) diluted upto 0.5ml with normal saline, mixed with 17.5 mg of hyperbaric bupivacaine 0.5% (3.5 ml). After overnight fasting, all the participants were premedicated with inj. Rantac 50mg i.v. 1 hour before surgery. Patients basal vital parameters were recorded preoperatively using multiparameter monitor in the O.T. Spinal block was performed with 25G Quincke’s spinal needle at the level of L3-L4 or L4-L5 intervertebral space, in the left lateral position, maintaining aseptic precautions. Following free flow of CSF, drug was injected slowly over 10 seconds and patients were immediately placed in the supine position for surgery. I.V fluids were given intraoperatively as and when necessary. The onset of sensory blockade i.e. time taken from the end of injection to loss of pin prick sensation at L1 dermatome, onset of complete motor blockade i.e. time taken from the end of injection to development of grade II motor block (modified Bromage's criteria), two-segment regression time from highest level of sensory blockade, duration of complete analgesia i.e. time from the intrathecal injection to the first complain of pain, duration of motor blockade (time required for motor blockade to return to Bromage's grade 0 from the time of onset of motor blockade) were studied and recorded. The changes in pulse rate, systolic and diastolic blood pressure, oxygen saturation (SpO2) and respiratory rate were monitored and recorded at 0, 5,10, 20 and 30 min and thereafter at every 30-min intervals up to 120 min after subarachnoid Block. Any side effects in the form of intra or postoperative hypotension, bradycardia, sedation, respiratory depression, nausea and vomiting and pruritus were recorded and treated appropriately. Intensity of pain was assessed by visual analogue score at 0, 10, 15, 30 and 60 minutes and then at 30-min intervals till 300 min after injection or until the patient received a rescue analgesic. Patients reporting a visual analogue score 3 or more or demand analgesia, were given rescue analgesics in the form of injection Diclofenac 1.5mg/kg IM.
Results
The data obtained from the study were collected and subjected to statistical analysis.
The level of significance was 0.05.
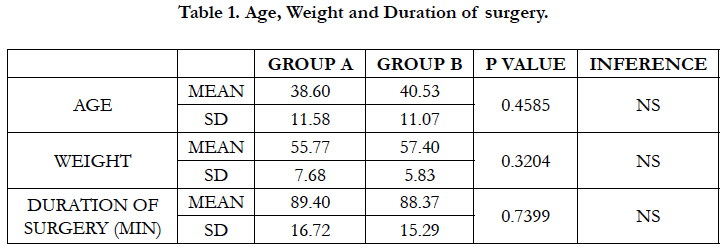
Table 1 shows that all participants in both groups were comparable with regard to age and weight distribution and duration of surgery. There was no significant difference in between them.
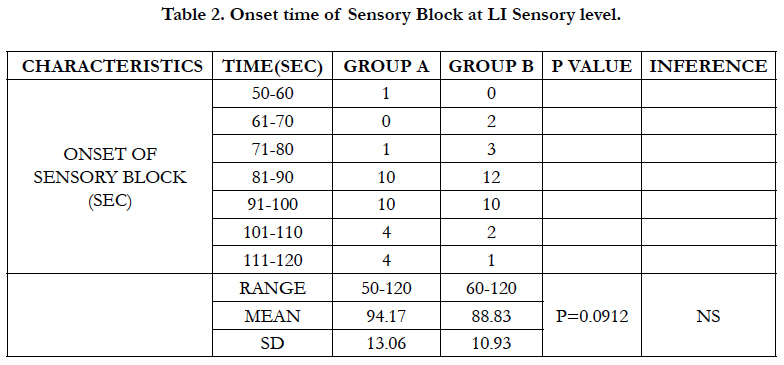
We can see from table no 2 that the onset time of sensory blockade in both the groups (Group A 94.17 ± 13.06, Group B 88.83 ± 10.93) were comparable and there is no significant difference with p value 0.0912.
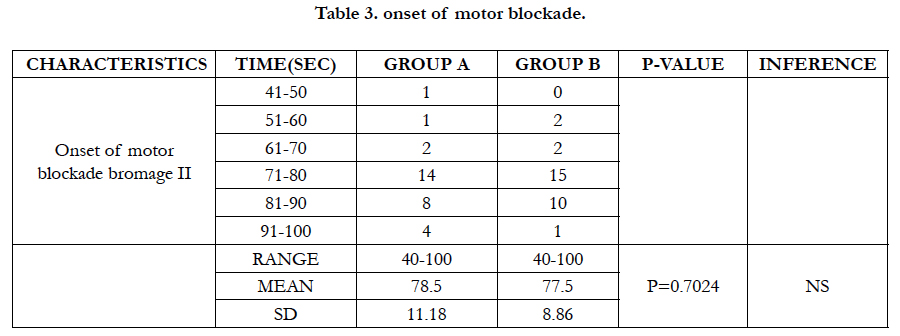
As shown in table 3, the onset time of Motor block in group A (78.5 ± 11.18) and in group B (77.5 ± 08.86) were comparable and there is no significant difference. (P = 0.7024).
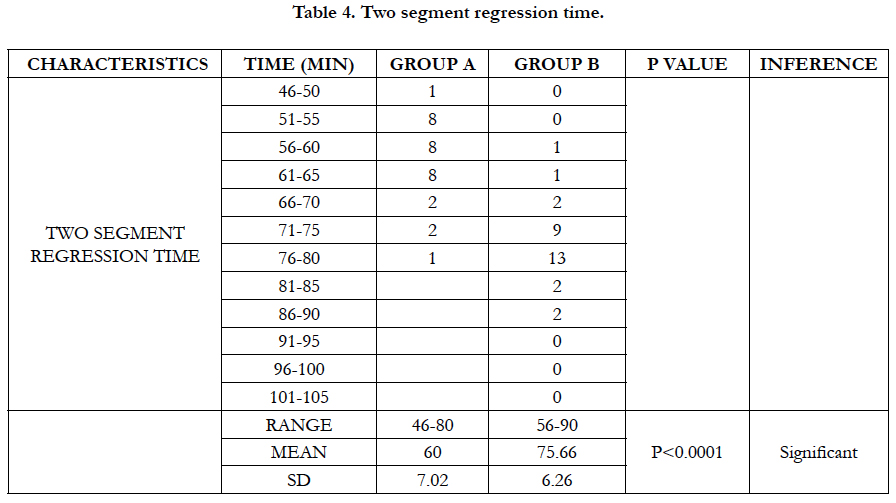
Table 4 is showing that Two segment regression time in group A (60 ± 7.02) is much shorter than group B (75.66 ± 6.26) minutes and the difference is highly significant (p < 0.0001).
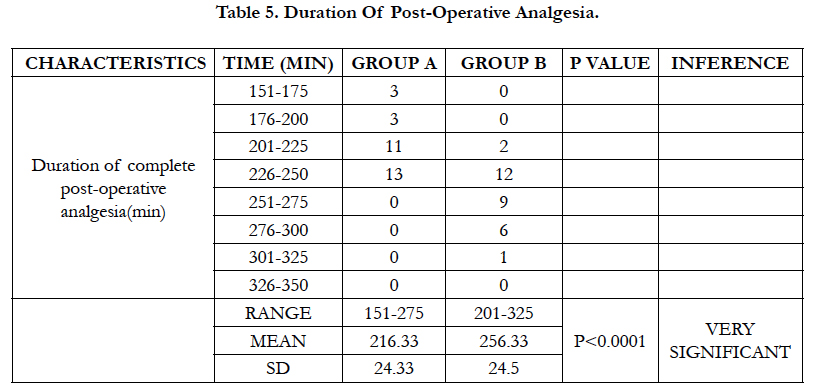
Table 5 is showing that duration of complete postoperative analgesia (in minutes) in group A (216.33 ± 24.33) is much shorter than group B (256.33 ± 24.50) and the difference is highly significant (p < 0.0001).
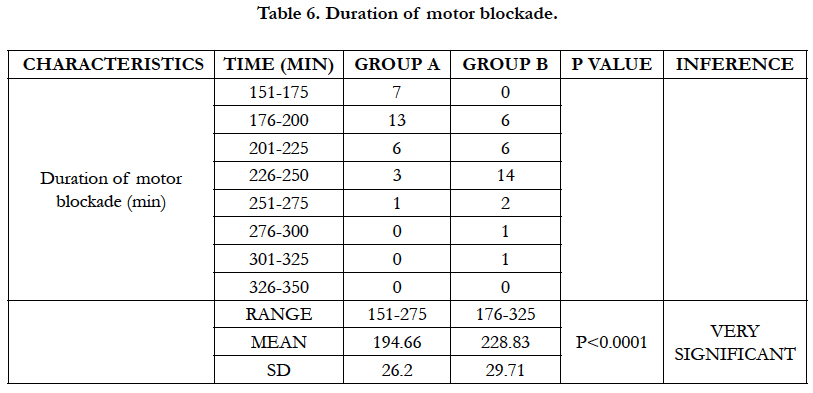
Table no 6 reveals duration of motor blockade in group A and group B as 194.66 ± 26.20 and 228.83 ± 29.71min respectively and the difference is significant with P < 0.0001.
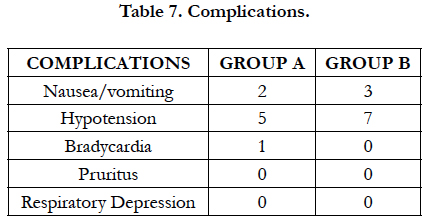
From table no 7, we can see that complication rate in both the groups are similar. While 2 patients in group A have developed vomiting, in group B, 3 patients have developed vomiting which were treated with inj. Ondansetron 4mg IV. Incidences of hypotension were similar in both the group. Episodes of hypotension were treated with IV Fluids and Vasopressor inj. Ephedrine. Transient bradycardia was seen in only 1 patient in group A which was treated with inj. Atropine. None of the patient developed either pruritus or respiratory depression which were typical of opioid related.
Discussion
Intrathecal opioids have been demonstrated to provide effective postoperative analgesia by acting on the opioid receptors in the spinal cord. Addition of opioids to local anaesthetics for intrathecal administration offers several advantages like faster onset, prolonged duration of action, reduced requirement of local anaesthetics along with decreased incidences of adverse effects. The combination has been shown to augment the sensory effect without affecting the duration of motor blockade.
In our study, the onset time of sensory block at LI sensory level (in seconds) in group A (94.17 ± 13.06) and group B (88.83 ± 10.93) were comparable and there was no significant difference (P = 0.912). And the onset time of Motor block (in seconds) in group A (78.5 ± 11.18), and group B (77.5 ± 08.88) were also comparable and there is no significant difference (P=0.7024). This is in contrast to the results obtained by Mukherjee A et al., [3]. In 2011 when they compared effect of different doses of nalbuphine as adjuvant to bupivacaine on sensory and motor blockade. They found that the onset time of sensory blockade following intrathecal injection of study solution containing 0.5 ml normal saline (NS) or 0.2, 0.4 and 0.8 mg Nalbuphine made up to 0.5 ml with NS added to 0.5% hyperbaric bupivacaine 12.5 mg (total volume 3 ml) to patients belonging to group A, group B, group C and group D were 1.75 ± 0.27, 1.69 ± 0.20, 1.63 ± 0.24, and 1.59 ± 0.18 minutes respectively. Similarly, onset time of motor blockade in group A, group B, group C and group D were 5.9 ± 0.57 5.8 ± 0.76, 5.7 ± 0.62 and 5.6 ± 0.53 minutes respectively. Among the groups, onset time of sensory and motor blockade were comparable and found to be statistically insignificant (P > 0.05) but when compared to our study, the early onset time in our study may be due to larger dose of inj. Nalbuphine and also use of different assessment criteria (for sensory blockade, use of L1 dermatome instead of T10 and for motor blockade, use of Bromage II instead of Bromage IV).
Tiwari A.K. et al., [4] in 2011, did a comparative study between two different doses of Intrathecal Nalbuphine admixed with 2.5ml of Bupivacaine. They randomly allocated 75 patients to 1 of 3 groups. Group A (n = 25) received 2.5 mL of 0.5% hyperbaric bupivacaine + 1ml sterile water Intrathecally; group B (n = 25) received 2.5ml of 0.5% hyperbaric bupivacaine + 1ml (200mcg) Nalbuphine Intrathecally and group C (n = 25) received 2.5ml of 0.5% hyperbaric bupivacaine + 1 mL (400 mcg) Nalbuphine Intrathecally. It was found from the study that, two segment regression time of sensory blockade as well as duration of analgesia were maximally prolonged in group C compared to group A and group B (P < 0.05). similar results were found in our study, the two-segment regression time (in minutes) in group A (60 ± 7.02) and group B (75.66 ± 6.26) were prolonged and the difference is significant (P=0.0001) and correlates with above mentioned study.
The analgesic as well as motor blocking effect of Nalbuphine appears to increase with increase in the dosage. Mostafa GM. et al., [5] found that 2mg of Nalbuphine when used intrathecally as an adjuvant to Bupivacaine, has produced comparatively prolonged analgesic and motor blocking effect lasting for 8.5 ± 3.67 hours and 5.9 ± 0.9 hours respectively. Mukherjee A et al., [3] in 2011, studied the effect of varying dose of intrathecal Nalbuphine (0.2mg vs. 0.4mg vs. 0.8mg) on duration of analgesia and motor blockade when used as an adjuvant to Bupivacaine. The duration of analgesia was progressively prolonged in groups 0.2mg, 0.4mg and 0.8mg with P < 0.05. 0.8mg recorded the longest duration of analgesia with a mean of 278.5 min compared with 237.3 min in 0.4mg. They recommend 0.4 mg as the optimal dose of Nalbuphine if used Intrathecally along with bupivacaine. The motor blockade was not altered significantly with change in the dosage of Nalbuphine.
In our study, the duration of sensory blockade (in minutes) in group A (216 ± 24.33) is much shorter than group B (256.00 ± 24.5) and the difference is highly significant (p < 0.0001). Similarly, duration of motor blockade in group A (194.66 ± 26.20) is much shorter than group B (228.83 ± 29.71) and the difference is found to be highly significant and also it does not correlate with above mentioned studies.
Several authors have compared the intrathecal Nalbuphine with intrathecal morphine and revealed varied results.
Lin ML [6] in 1992, compared the analgesic effect of subarachnoid administration of low dose morphine with that of Nalbuphine when administered as adjuvant with tetracaine for spinal anaesthesia and they didn’t find significant differences in duration of analgesia between the groups.
Fournier et al., [7] in 2000, compared Intrathecal morphine with Nalbuphine for postoperative pain relief after total hip replacement. They concluded that administration of Intrathecal Nalbuphine resulted in a shorter duration of analgesia than Intrathecal morphine.
Culebras X et al., [8] in 2000, compared effects of intrathecal morphine with that of Nalbuphine. They found that durations of complete and effective analgesia were significantly increased in morphine 0.2 mg (275 ± 228 min., 585 ± 446 min.) compared with Nalbuphine 0.2mg (108 ± 23 min., 136 ± 22 min.), Nalbuphine 0.8 mg (176 ± 62min., 212 ± 72min.), Nalbuphine 1.6 mg (148 ± 45min., 193 ± 77min) and further they found that increasing the Nalbuphine dose to 1.6 mg did not further improve analgesia.
Use of intrathecal opioids is associated with complications like pruritus, nausea/vomiting, sedation, hypotension, bradycardia and respiratory depression. Authors like Lin ML, have reported less side effects following Nalbuphine than with morphine.
Mukherjee A et al., reported dose dependent increase in incidence of complications in terms of hypotension, bradycardia, nausea/ vomiting and pruritus following Nalbuphine.
In our study, 2 patients from group A and 3 patients from group B developed vomiting and were treated with inj. Ondansetron 4mg IV. Significant hypotension was seen in 5 patients in group A and 7 patients in group B. They were given IV fluids and Vasopressors. Only one patient had developed bradycardia and was treated with inj. Atropine. None of the patients developed pruritus or respiratory depression.
Conclusion
Intrathecal Nalbuphine (1.4mg) added to Intrathecal Bupivacaine 0.5% heavy (17.5mg) provides prolonged postoperative analgesia without increasing risk of side effects. Further studies are required to determine optimal dosage of intrathecal Nalbuphine.
References
- Stoelting pharmacology and physiology. 4th edition. 2006. p.90-119.
- Millers anesthesia. 7th edition.
- Mukherjee A, Pal A, Agrawal J, Mehrotra A, Dawar N. Intrathecal nalbuphine as an adjuvant to subarachnoid block: What is the most effective dose?. Anesth Essays Res. 2011 Jul-Dec;5(2):171-5. PubMed PMID: 25885383.
- Tiwari AK, Tomar GS, Agrawal J. Intrathecal bupivacaine in comparison with a combination of nalbuphine and bupivacaine for subarachnoid block: A randomized prospective double-blind clinical study. Am J Ther. 2013 Nov-Dec;20(6):592-5. PubMed PMID: 21904194.
- Mostafa MG, Mohamad MF, Farrag WS. Which has greater analgesic effect: intrathecal nalbuphine or intrathecal tramadol. J Am Sci. 2011;7:480.
- Lin ML. The analgesic effect of subarachnoid administration of tetracaine combined with low dose of morphine or nalbuphine for spinal anaesthesia. Ma Zui Xue Za Zhi. 1992 Jun;30(2):101-5. PubMed PMID: 1528093.
- Fournier R, Van Gessel E, Macksay M, Gamulin Z. Onset and offset of intrathecal morphine versus nalbuphine for postoperative pain relief after total hip replacement. Acta Anaesthesiol Scand. 2000 Sep 1;44(8):940-5.
- Culebras X, Gaggero G, Zatloukal J, Kern C, Marti RA. Advantages of intrathecal Nalbuphine, compared with intrathecal morphine, After caesarean delivery: An Evaluation of Postoperative Analgesia and Adverse Effects; An evaluation of post-operative analgesia & adverse effects. Anesth Analg. 2000 Sep;91(3):601-5. PubMed PMID: 10960384.
- Moustafa MA, Saleh RS. Nalbuphine added to intrathecal morphine in total knee arthroplasty; effect on postoperative analgesic requirements and morphine related side effects. Bull Alexandria Fac. 2012 Jun 1;48(2):175-8.