Development Process of Sepsis Diagnosis
Kucuk AO, Senel H, Ozdemir A, Eroğlu A*
Department of Anesthesiology and Reanimation, Intensive Care Department, Karadeniz Technical University, Trabzon, Turkey.
*Corresponding Author
Ahmet Eroglu,
Department of Anesthesiology and Reanimation,
Intensive Care Department, Karadeniz Technical University,
Trabzon 61080, Turkey.
Tel: +904623775900
E-mail: aheroglu@hotmail.com
Received: July 05, 2018; Accepted: July 30, 2018; Published: July 31, 2018
Citation: Kucuk AO, Senel H, Ozdemir A, Eroğlu A. Development Process of Sepsis Diagnosis. Int J Anesth Res. 2018;6(6):526-531. doi: dx.doi.org/10.19070/2332-2780-18000106
Copyright: Eroğlu A© 2018. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Sepsis is a heterogeneous clinical condition that is most common in intensive care units, which is the cause of morbidity, mortality and increased cost. Diagnosis at the earliest stage in the clinical diversity that can progress from simple infection to sepsis and septic shock is the primary clinical goal. Clinical studies and consensus reports have been published and published over the years so that early diagnosis and resuscitation can be started quickly. In fact, it is easy to use in clinical practice and clinical criteria can be set to facilitate the work of the physician without complicated laboratory procedures. Thus, the treatment stage can be overcome to prevent this severe infectious process leading to organ dysfunction and increased mortality. In this review, consensus definitions used in the definition of sepsis, the latest consensus recommendation, and current developments in sepsis are summarized.
2.Abbreviations
3.Introduction
4.Sepsis Identification Methods
4.1 Sepsis-I
4.2 Sepsis-II
4.3 Why change was needed?
4.4 Sepsis-III
5.Current Developments in Sepsis
6.Conclusion
7.References
Keywords
Sepsis; Diagnosis; Development.
Abbreviations
qSOFA: Quick Sequential Organ Failure Assessment; ICON: Intensive Care Over Nations; ICU: Intensive Care Unit; CRP: C-Reactive Protein; PCT: Procalcitonin; SIRS: Systemic Inflammatory Response Syndrome; ACCP: American College of Chest Physicians; SCCM: Society of Critical Care Medicine; ESICM: European Society of Intensive Care Medicine.
Introduction
Infections are common throughout life at all ages. In most individuals, the host response is sufficient to cope with the potential threat and if bacterial, it can be treated with appropriate antibiotics. In some cases, however, the infection may be associated with an insufficient or inappropriate host response, which may progress to the development of organ dysfunction. At this point, the term "sepsis" is used [1-3].
Sepsis continues to be a serious public health problem worldwide. This serious, costly and high mortality rate among the most common causes of intensive care hospitalizations is unfortunately still present in many years of change and development and its treatment is difficult. The Islamist philosopher Ibn Sina as the tissue and blood putrefaction with fire [4] first described it. Although the clinical picture of sepsis has not changed much since the first day, the management of organ failure has changed and serious infections that have previously been fatal have begun to be managed more effectively nowadays.
The Intensive Care Over Nations (ICON) study provided global epidemiological data on 10,069 intensive care unit (ICU) patients and confirmed that 2,973 (29.5%) patients received sepsis at the time of admission or intensive care unit hospitalization [5]. Sepsis, on the other hand, has also been described as "the ultimate way of death from infection" in the process [6]. According to the Global Burden of Disease, more than 10 million people die from the infectious disease every year, and this number is higher than cancer-related deaths [7]. This condition, which has high mortality, may also result in mental and physical impairments leading to reduced long-term quality of life [8]. Sepsis mortality rates were 41% in Europe and 28.3% in the USA, and in the case of septic shock this rate could be up to 50% [9, 10]. Vincent et al., Found that intensive care unit mortality was 25.8% and hospital mortality was 35.3% in sepsis patients in 2014. These rates are significantly higher than the general intensive care unit population [5].
The diagnosis and care of patients with sepsis is quite complicated because of the influence of various organ systems. Infection is absolutely necessary for the diagnosis of sepsis. Some patients may have a sepsis-like condition without evidence of infection. Prognosis and treatment of these conditions are very different from true sepsis [3]. Over time, the need to develop standard baseline recommendations in the management of sepsis patients evaluated by different health professionals in different clinics has emerged. For this purpose; sepsis definitions were made at international conferences in 1991, later in 2001 and 2016 [1, 11, 12].
Sepsis Identification Methods
Infection is defined as "a pathological process in which pathogenic or potentially pathogenic microorganisms invade sterile tissue, fluid or body cavities" [12]. Sepsis; is defined as the presence of life-threatening organ dysfunction that occurs with a dysregulated host response to any infection [1-3]. Generally, three different conditions are identified and the presence of infection is suspected and confirmed.
1. The beginning of a host response and symptoms: Fever and shivering are the most typical clinical reactions. The biological response is monitored both in the number of white blood cells and in the concentrations of inflammatory markers (e.g. blood C-reactive protein (CRP) or procalcitonin (PCT))
2. Presence of infectious symptoms for suspect focus: for example, dizziness and scented urine; abnormal chest auscultation or typical radiographic chest infiltrates and respiratory symptoms; purulent injuries; meningitis indication.
3. Proof of invasion of microbiological agents in a sterile medium (detection of microorganism in peritoneal tissue in a cirrhotic patient) or detection of superinfection in non-sterile environment (gastrointestinal system).
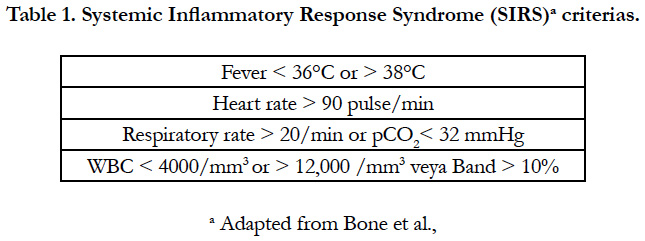
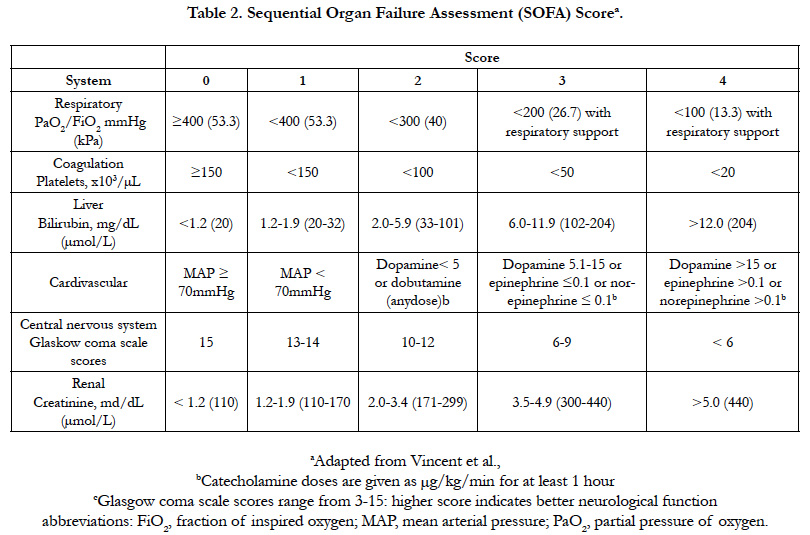
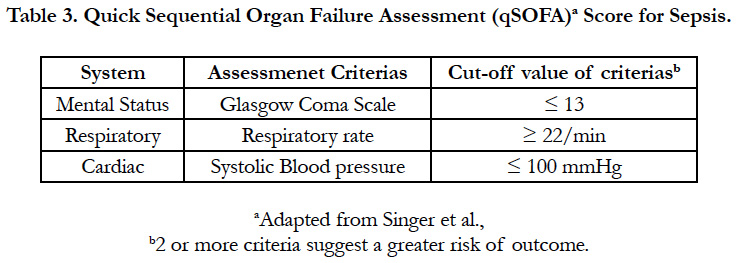
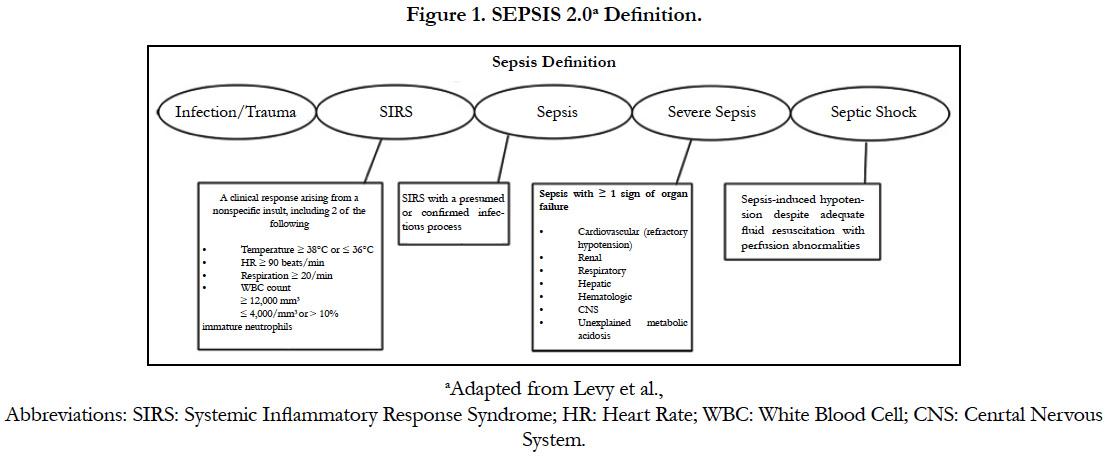
However, it is not always easy to diagnose sepsis for early treatment. Each patient in the course of realization of the same scenario is unlikely, for example, without fever in some patients, even patients with sepsis may be especially elderly patients presenting with hypothermia [13, 14]. The diagnosis of these patients is rather late and difficult. The main goal of many years of work is to be able to diagnose sepsis at the earliest, to prevent shock and multiple organ failure. With the recommendation of the 1992 North American consensus document, sepsis was defined as a combination of systemic inflammatory response syndrome (SIRS) and infection. SIRS criteria (especially fever, tachycardia and altered white blood cell count) reflect the typical characteristics of the infection (Table 1) [11]. Over the years, this approach has been shown to result in a significant increase in patients receiving a diagnosis of sepsis. However, these patients may actually have less serious illness, and deceptive reductions in mortality rates may have been reported [15, 16]. Over time, it has begun to be considered that the SIRS criteria are highly sensitive and not specific enough for this purpose. Sprung et al., reported that 93% of ICU patients provided at least two SIRS criteria at one point during their stay in ICU. Dulhunty et al., found this rate as 88.4% [17, 18]. The SOFA scoring system is a scoring system that is used to determine the prevalence and speed of sepsis-related organ dysfunction. It is used to calculate the level of organ dysfunction in six systems (respiratory, cardiovascular, liver, coagulation, renal, neurological) (Table 2). This scoring system is performed on admission to the patient's intensive care unit and is calculated every 24 hours [19]. A calculation based on average and worst outcomes in intensive care unit is calculated. According to the SOFA, mortality rates can only be valuable during the stay in intensive care. If the score is between 0 and 6, mortality should be expected to be <10%; for scores of 13-14, 50% mortality should be expected, and for scores above 15, mortality of 90% should be expected [17]. In the last consensus report, more radical changes were made and a quick SOFA (qSOFA) was placed in the first part of the diagnostic process [1]. When evaluating six components of the SOFA score, the need for laboratory analyzes and time required a new rapid assessment method. qSOFA is defined by three clinical contexts (hypotension, altered mental status, and tachypnea) that can be used at bedside to describe infected patients at risk of worsening of condition (Table 3) [1]. The presence of two or more of these early warning system components may prompt the clinician to better assess the presence of infection or organ dysfunction in the patient and to determine the need for early intensive care. However, although qSOFA is not part of the new sepsis definition. Vincent et al., emphasized that SIRS is part of the definition of sepsis. The SOFA criteria required for new sepsis definition are sufficient for organ dysfunction criteria. qSOFA is clinically valuable but not a perfect sepsis marker [20]. Currently, there is debate about the last Sepsis-3 definitions. The American College of Chest Physicians [21], the Infectious Disease Society of America, the Latin American Sepsis Institute [22], the American College of Emergency Physicians, and no emergency medical community has not approved it.
Sepsis in 1991; is defined as the presence of two or more SIRS criteria in addition to known or suspected infection. The American College of Chest Physicians (ACCP) and the Society of Critical Care Medicine (SCCM) refer to sepsis as an "ongoing process." The SIRS criterion set out above (Table 1) is the basis for the definition. In addition, according to clinical severity, a graded classification was made. In clinical practice, sepsis, severe sepsis, septic shock, and multiple organ dysfunction syndrome definitions have begun to be used [12]. Severe sepsis, hypotension with fluid and vasopressor resistance, and septic shock in the presence of hypo perfusion and hypo perfusion have been described in clinical manifestations, including hypotension, hypo perfusion, and organ dysfunction. However, after a while, the fact that some of the sepsis-like hyperkinetic clinical tables without infections could be confused with these definitions. The SIRS criteria used in the definition of sepsis include susceptibility (tachycardia, hyperventilation, leukocytosis) and infection findings primarily (e.g. fever and increased number of white blood cells) to occur with any form of stress. Thus, the misconception that patients who are actually infected but not sepsis may have been included in the definition of sepsis has begun to be discussed.
In 2001, an attempt was made to revise the SIRS criteria, but the list of sepsis symptoms was quite long to be accepted. Despite this insufficiency, the SIRS criteria defined in 1991 continued to be used. In this consensus, a new term for sepsis was proposed and described as "a clinical syndrome with organ damage", but the previous criteria of sepsis continued to be used. Severe sepsis is defined as sepsis complicated by organ dysfunction [12]. In the 2003 update, biochemical markers and their role in early diagnosis were considered [12], categorized as documented or suspected infection- specific findings as general, inflammatory, hemodynamic, organ dysfunction and tissue perfusion parameters.
To define a definitive sepsis according to the SIRS criteria, we need to be able to determine whether sepsis is the same as sterile inflammation. Many noninfectious conditions associated with acute tissue injury and innate immune activation; multiple trauma, pancreatitis, transplant rejection, and autoimmune diseases. Both invasive infection and sterile tissue necrosis are activating inflammatory, coagulation, microbial clearance and other tissue repair pathways [23]. Clinical manifestations are often insufficient to distinguish this sterile inflammatory response alone from the response initiated by the infection. This effect indicates that SIRS can not distinguish between patients with severe infection and those who are not infected but have major injuries. In conclusion, SIRS has low sensitivity and specificity to distinguish no complicated infection from sepsis. The primary reason for the need for an update is the need for rapid implementation of early diagnosis and treatment procedures in the sepsis process. It is widely accepted that the definition should include important parameters such as host response and severe organ dysfunction that may be associated with simple infection and septicemia.
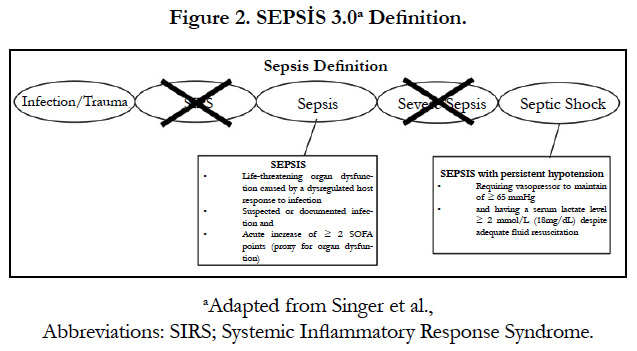
The Society of Critical Care Medicine (SCCM) and the European Society of Intensive Care Medicine (ESICM) to revise the current sepsis and septic shock definitions convened an international task force with 19 participants. Using an expert Delphi consensus process, this group developed the new Sepsis-3 definitions [1]. With these new consensus decisions, sepsis was described as "lifethreatening organ dysfunction that caused a dysregulated host response to infection". As clinical criteria for the diagnosis of sepsis; a suspected or documented focus of infection and two or more acute increases in SOFA score for organ dysfunction. Septic shock; was defined as a subset of sepsis in which the underlying circulatory and cellular/metabolic abnormalities were deep enough to significantly increase mortality. In other words, septic shock, sepsis-related acute circulatory insufficiency. Clinical criteria for septic shock diagnosis are lactate > 2 mmol / L (18 mg/ dL) in spite of adequate fluid resuscitation and the need for vasopressor to make a mean arterial pressure ≥ 65 mmHg with sepsis diagnosis (Figure 2). When a newly developed and unexplained organ dysfunction is defined in a patient, it should be remembered that the patient may be sepsis. According to this consensus, mortality was 10% in patients with sepsis diagnosis and 40% in patients with septic shock diagnosis [1]. However, discussions about the inclusion of lactate in the definition of septic shock by Sepsis-3 and the lactate measurement used in the definition (> 2 mmol/L) are still ongoing. It is recommended to evaluate "lactate clearance" more than spot lactate measurement. Vincent et al., evaluated 96 studies and indicated that the reduction in levels in a lactate measurement every 1-2 hours was clinically more valuable. In clinical practice it is thought that the change in lactate levels over time reflects primarily the change in production. Increased lactate levels are generally associated with circulatory disturbances, with an improvement in circulation suggesting a decrease in lactate levels and a reduction in production (but can not be proved) [24]. At least four different mechanisms should be assessed for the presence of hyperlactatemia. These; anaerobic glycolysis in hypoperfactive areas, especially in severe microcirculation disorders; aerobic glycolysis due to stress-induced adrenergic; impaired liver lactate clearance; and mitochondrial dysfunction that limits pyruvate metabolism. It is important to recognize the clinical pattern of hyperlactatemia associated with hypo perfusion, because more resuscitation in cases not associated with hypo perfusion may result in toxicity due to excessive resuscitation [25, 26]. Persistent hyperlactatemia, which is not associated with hypoperfusion, is associated with a better prognosis, so the distinction must be made well. Simultaneous analysis of parameters such as central venous O2 saturation (ScVO2), central venous-arterial pCO2 gradient (Pcv-aCO2> 6 mmHg) and peripheral perfusion (capillary reflux time, peripheral perfusion index, skin temperature, mottling) is important in the detection of hypo perfusion [25]. The most common reasons for the increase in blood lactate level are; the use of catecholamine in septic shock patients, the increase in alkalosis-induced glucose metabolism, continuous hemofiltration with lactate buffer, liver dysfunction and lung lactate production. Lactate levels have also been associated with the use of specific drugs (nucleoside reverse transcriptase inhibitors used for HIV therapy, metformin), some poisonings (ethylene glycol, methanol and steroids) [27, 28]. Sepsis is a heterogeneous disease that can be associated with many different types of infections and some other features. This heterogeneity has attempted to explain the different components of the complex disease process with the PIRO classification system, which was defined about 10 years ago. In this model, P predisposing factors are genetic, past history, clinical context; I aspects of the (confirmed or suspected) infectious source and the microorganism responsible (when this information is available) R; vital signs of the patient and sepsis markers such as CRP, procalcitonin and human leucocyte antigen DR; O represents organ dysfunction based on six easily assessable functions [12]. Another priority is to identify the sepsis early. The best known and valuable method for this is the SOFA score, but the calculation for early diagnosis is quite complicated. Large database analyzes have shown that three simple elements (tachycardia, hypotension, and altered menstrual condition) in the score can provide sufficient information and an adequate alarm in the diagnosis of sepsis, and qSOFA is defined. This model is easy to remember and can be quickly assessed by nurses and other health personnel who are unfamiliar with the symptoms of sepsis. In a patient with a suspected infection, the QSOFA is very stimulating to initiate the necessary laboratory tests by informing the intensive care team or the educated staff. Importantly, the SOFA (and qSOFA) score reflects both chronic and acute changes in organ function, so changes in SOFA scores over time are more beneficial than a single static value [29]. Early diagnosis and hemodynamic resuscitation provide rapid application of broad spectrum antibiotics to target infectious microorganisms as well as rapid control of the infection. There is very little data on the use of qSOFA as a screening method for early and accurate estimation of sepsis and mortality in admission to the ICU. In addition, it is suggested that qSOFA has inadequate prognostic accuracy in anticipating hospital mortality in ICU patients with suspected infection. SOFA was found to be more valuable than both SIRS and qSOFA for predicting in-hospital mortality [30].
Current Developments in Sepsis
It is important to remember that sepsis is not just a disease but a heterogeneous syndrome associated with a specific infectious disease. Many methods for diagnosis and treatment of sepsis continue to be developed. In recent years, molecular methods have been started to provide more perceptible data for SIRS, qSOFA and SOFA for rapid diagnosis of sepsis. Miller et al. investigated the efficacy of molecular diagnostic tests in separating sepsis from sterile inflammation. The SeptiCyteTM LAB is a real-time, reverse-transcription, quantitative polymerase chain reaction (RTqPCR) assay that quantitates the relative expression levels of four genes (CEACAM4, LAMP1, PLAC8, PLA2G7) with a turnaround time of approximately 6 hours. The proposed test generates score in four groups, and uses a binary cutoff of 3.1 to classify patients as high or low risk of sepsis [31]. However, the most recently accepted Third International Sepsis and Septic Shock ("Sepsis-3") excluded molecular testing due to lack of evidence and pragmatism within the recommended criteria. The answers to these questions are still unclear for SeptiScore™; what should be the optimal working time (s)? , if less than 3.1, should antibiotics be cut off? Should it be used in the clinical routine? Is it anticipated to start antibiotics until the conclusion? [32]. According to the results of a recent published study, the results of SeptiCyte LAB are based on gene expression profiles, so test results may vary between populations. For this reason, prospective studies are needed to determine the clinical benefit of this new test [33]. The patient's sepsis phenotype identifies the host's genetic variability, comorbidities, individual characteristics, and possibly explains differences in treatment response. Grimaldi and Vincent emphasize that in the future sepsis diagnosis and treatment will no longer focus on the so-called sepsis drugs and that the patient with special sepsis phenotypes will allow the right treatments to be administered right away [34]. On the other hand, Marik has recently stated that vitamin C is used in endogenous catecholamine biosynthesis in septic patients, markedly decreasing and acting as a stress hormone rather than as a nutrient. Vitamin C is a key cellular antioxidant, detoxifying exogenous oxidants radical species that have entered cells or which have arisen within cells due to excess superoxide generation by mitochondrial metabolism, by NADPH oxidase, xanthine oxidase or by uncoupled nitric oxide synthase (NOS) [36]. Experimental studies show that intravenous use of vitamin C reverses the organ dysfunction of sepsis. It can also act synergistically with corticosteroids, thiamine and Vitamin C to improve patient outcomes in sepsis and septic shock. It is argued that this cheap and easily found drug combination has the potential to reduce sepsis-induced mortality [35]. Key interventions in treatment, as is known in patients with sepsis and septic shock; antibiotics, hemodynamic interventions including fluid replacement and, if necessary, vasopressor support. Surviving Sepsis Campaign: The International Guidelines for Management of Sepsis and Septic Shock 2016 were revised in February 2018 and updated to the "hour-1bundle" recommendation. The previous sepsis was defined as "time zero" or "time of presentation" as defined in the bundle, when emergency care triage time or if presenting from another care venue. The most important change in the revision of the SSC bundles is that the 3-h and 6-h bundles have been combined into a single “hour-1 bundle” with the explicit intention of beginning resuscitation and management immediately. The first 1 hour bundle is recommended; lactate measurement, > 2 mmol / L re-measurement, draw of blood cultures without antibiotic initiation, initiation of broad spectrum antibiotics, during fluid resuscitation, the patient is hypotensive, and there is vasopressor administration to keep the mean arterial ressure at 65 mmHg [37].
Conclusion
When describing the Sepsis, it is necessary to remember the underlying physiological and terminological rules. The most recent definition of sepsis is conceptually based on infection and emphasizes organ dysfunction first. Current targets for which the physician in Sepsis should be synchronized with the predictions about the patient; should be easy to use at the bedside, provide simple parameterization and provide patient-specific treatment by determining organ dysfunctions.
References
- Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016 Feb 23;315(8):801-10. doi: 10.1001/jama.2016.0287. PubMed PMID: 26903338.
- Vincent JL, Mira JP, Antonelli M. Sepsis: older and newer concepts. Lancet Respir Med. 2016 Mar;4(3):237-40. doi: 10.1016/S2213-2600(15)00522- 6. PubMed PMID: 26917436.
- Vincent JL, Opal SM, Marshall JC, Tracey KJ. Sepsis definitions: time for change. Lancet. 2013 Mar 2;381(9868):774-5. doi: 10.1016/S0140-6736(12)61815-7. PubMed PMID: 23472921.
- Majno G. The ancient riddle of sigma eta psi iota sigma (sepsis). J Infect Dis. 1991 May;163(5):937-45. PubMed PMID: 2019770.
- Vincent JL, Marshall JC, Ñamendys-Silva SA, François B, Martin-Loeches I, Lipman J, et al. Assessment of the worldwide burden of critical illness: the intensive care over nations (ICON) audit. Lancet Respir Med. 2014 May;2(5):380-6. doi: 10.1016/S2213-2600(14)70061-X. PubMed PMID: 24740011.
- Kissoon N, Daniels R, van der Poll T, Finfer S, Reinhart K. Sepsis - the final common pathway to death from multiple organ failure in infection. Crit Care Med. 2016 Jun;44(6):e446. doi: 10.1097/CCM.0000000000001582. PubMed PMID: 27182871.
- GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016 Oct 8;388(10053):1545-1602. doi: 10.1016/S0140-6736(16)31678-6. PubMed PMID: 27733282.
- Karlsson S, Karlsson S, Ruokonen E, Varpula T, Ala-Kokko TI, Pettilä V. Longterm outcome and quality-adjusted life years after severe sepsis. Crit Care Med. 2009 Apr;37(4):1268-74. doi: 10.1097/CCM.0b013e31819c13ac. PubMed PMID: 19242321.
- Levy MM, Artigas A, Phillips GS, Rhodes A, Beale R, Osborn T, et al. Outcomes of the Surviving Sepsis Campaign in intensive care units in the USA and Europe: a prospective cohort study. Lancet Infect Dis. 2012 Dec;12(12):919-24. doi: 10.1016/S1473-3099(12)70239-6. PubMed PMID: 23103175.
- Vincent JL, Sakr Y, Sprung CL, Ranieri VM, Reinhart K, Gerlach H, et al. Sepsis in European intensive care units: results of the SOAP study. Crit Care Med. 2006 Feb;34(2):344-53. PubMed PMID: 16424713.
- Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992 Jun;101(6):1644-55. PubMed PMID: 1303622.
- FLevy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 sccm/esicm/accp/ats/sis international sepsis definitions conference. Crit Care Med. 2003 Apr;31(4):1250-6. PubMed PMID: 12682500.
- Kushimoto S, Gando S, Saitoh D, Mayumi T, Ogura H, Fujishima S, et al. The impact of body temperature abnormalities on the disease severity and outcome in patients with severe sepsis: an analysis from a multicenter, prospective survey of severe sepsis. Crit Care. 2013 Nov 13;17(6):R271. doi: 10.1186/cc13106. PubMed PMID: 24220071.
- Öncü S. A clinical outline to fever in intensive care patients. Minerva Anestesiol. 2013 Apr;79(4):408-18. PubMed PMID: 23370123.
- Kaukonen KM, Bailey M, Suzuki S, Pilcher D, Bellomo R. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000-2012. JAMA. 2014 Apr 2;311(13):1308-16. doi: 10.1001/jama.2014.2637. PubMed PMID: 24638143.
- Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003 Apr 17;348(16):1546-54. PubMed PMID: 12700374.
- Dulhunty JM, Lipman J, Finfer S, Sepsis Study Investigators for the ANZICS Clinical Trials Group. Does severe non-infectious SIRS differ from severe sepsis?. Intensive Care Med. 2008 Sep;34(9):1654-61. doi: 10.1007/s00134-008-1160-2. PubMed PMID: 18504549.
- Sprung CL, Sakr Y, Vincent JL, Le Gall JR, Reinhart K, Ranieri VM, et al. An evaluation of systemic inflammatory response syndrome signs in the Sepsis Occurrence In Acutely Ill Patients (SOAP) study. Intensive Care Med. 2006 Mar;32(3):421-7. PubMed PMID: 16479382.
- Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996 Jul;22(7):707-10. PubMed PMID: 8844239.
- Vincent JL, Martin GS, Levy MM. qSOFA does not replace SIRS in the definition of sepsis. Crit Care. 2016 Jul 17;20(1):210. doi: 10.1186/s13054- 016-1389-z. PubMed PMID: 27423462.
- Cortés-Puch I, Hartog CS. Opening the debate on the new sepsis definition change is not necessarily progress: revision of the sepsis definition should be based on new scientific insights. Am J Respir Crit Care Med. 2016 Jul 1;194(1):16-8. doi: 10.1164/rccm.201604-0734ED. PubMed PMID: 27166972.
- Machado FR, Salomão R, Pontes de Azevedo LC. Why LASI did not endorse the new definitions of sepsis published today in JAMA. on behalf of the Latin American Sepsis Institute. 2016.
- Andersson U, Tracey KJ. HMGB1 is a therapeutic target for sterile inflammation and infection. Annu Rev Immunol. 2011;29:139-62. doi: 10.1146/ annurev-immunol-030409-101323. PubMed PMID: 21219181.
- Vincent JL, E Silva AQ, Couto L, Taccone FS. The value of blood lactate kinetics in critically ill patients: a systematic review. Crit Care. 2016 Aug 13;20(1):257. doi: 10.1186/s13054-016-1403-5. PubMed PMID: 27520452.
- Alegría L, Vera M, Dreyse J, Castro R, Carpio D, Henriquez C, et al. A hypoperfusion context may aid to interpret hyperlactatemia in sepsis-3 septic shock patients: a proof-of-concept study. Ann Intensive Care. 2017 Dec;7(1):29.doi: 10.1186/s13613-017-0253-x. PubMed PMID: 28281216.
- Hernandez G, Luengo C, Bruhn A, Kattan E, Friedman G, Ospina-Tascon GA, et al. When to stop septic shock resuscitation: clues from a dynamic perfusion monitoring. Ann Intensive Care. 2014 Oct 11;4:30. doi: 10.1186/s13613-014-0030-z. PubMed PMID: 25593746.
- Garcia-Alvarez M, Marik P, Bellomo R. Sepsis-associated hyperlactatemia. Crit Care. 2014 Sep 9;18(5):503. doi: 10.1186/s13054-014-0503-3. Pub- Med PMID: 25394679.
- Jansen TC, van Bommel J, Bakker J. Blood lactate monitoring in critically ill patients: a systematic health technology assessment. Crit Care Med. 2009 Oct;37(10):2827-39. doi: 10.1097/CCM.0b013e3181a98899. PubMed PMID: 19707124.
- Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001 Oct 10;286(14):1754-8. PubMed PMID: 11594901.
- Raith EP, Udy AA, Bailey M, McGloughlin S, MacIsaac C, Bellomo R, et al. Prognostic accuracy of the SOFA score, SIRS criteria, and qSOFA score for in-hospital mortality among adults with suspected infection admitted to the intensive care unit. JAMA. 2017 Jan 17;317(3):290-300. doi: 10.1001/jama.2016.20328. PubMed PMID: 28114553.
- Miller III RR, Lopansri BK, Burke JP, Levy M, Opal S, Rothman RE, et al. Validation of a Host Response Assay, Septicyte™ LAB, for Discriminating Sepsis from SIRS in the ICU. Am J Respir Crit Care Med. 2018 Apr 6. doi: 10.1164/rccm.201712-2472OC. PubMed PMID: 29624409.
- Seymour CW, Bernard G. Making Sepsis Molecular–Is There Enough Time for New Tests?. Am J Respir Crit Care Med. 2018 Apr 20. doi: 10.1164/ rccm.201804-0684ED. PubMed PMID: 29676931.
- Koster-Brouwer ME, Verboom DM, Scicluna BP, van de Groep K, Frencken JF, Janssen D, et al. Validation of a novel molecular host response assay to diagnose infection in hospitalized patients admitted to the ICU with acute respiratory failure. Crit Care Med. 2018 Mar;46(3):368-374. doi: 10.1097/ CCM.0000000000002735. PubMed PMID: 29474322.
- Grimaldi D, Vincent JL. Clinical trial research in focus: rethinking trials in sepsis. Lancet Respir Med. 2017 Aug;5(8):610-611. doi: 10.1016/S2213- 2600(17)30268-0. PubMed PMID: 28748806.
- Marik PE. Vitamin C for the treatment of Sepsis: The Scientific Rationale. Pharmacol Ther. 2018 Apr 21. pii: S0163-7258(18)30070-6. doi: 10.1016/j. pharmthera.2018.04.007. PubMed PMID: 29684467.
- Oudemans-van Straaten HM, Spoelstra-de Man AM, de Waard MC. Vitamin C revisited. Crit Care. 2014 Aug 6;18(4):460. doi: 10.1186/s13054-014-0460-x. PubMed PMID: 25185110.
- Levy MM, Evans LE, Rhodes A. The surviving sepsis campaign bundle: 2018 update. Intensive Care Med. 2018 Jun;44(6):925-928. doi: 10.1007/ s00134-018-5085-0. PubMed PMID: 29675566.