Clinical Application of Upper Airways Topical Anesthesia in Endotracheal Intubation in Awake Patients of Giant Goiters
Cangyuan J1,2,4, Weiping Z2, Danbing X2, Lijian C2, Haifei X2, Feng L2, Liping J2, Ying Y2, Jun L3, Dong X4,5, Hongcai C2, Xianju L2, Seydou T6*
1 Taizhou Hospital of Zhejiang Province, Taizhou Zhejiang, China.
2 Taizhou Enze Hospital, Taizhou Zhejiang, China.
3 The 2nd Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical University, Wenzhou Zhejiang, China.
4 25th Chinese Meidcal Team, Mali Hospital, Bamako, Mali.
5 The Second Affiliated Hospital of Zhejiang Chinese Medical University, Hangzhou Zhejiang, China.
6 Department of Thoracic Surgery of Mali Hospital, Bamako, Mali.
*Corresponding Author
Togo Seydou MD, PHD,
Department of Thoracic Surgery of Mali Hospital, Bamako, 999053; Mali.
Tel: +223 65511651
E-mail: drseydoutg@yahoo.fr
Received: February 19, 2019; Accepted: March 25, 2019; Published: March 27, 2019
Citation: Cangyuan J, Weiping Z, Danbing X, Lijian C, Haifei X, Seydou T, et al., Clinical Application of Upper Airways Topical Anesthesia in Endotracheal Intubation in Awake Patients of Giant Goiters. Int J Anesth Res. 2019;7(2):565-571. doi: dx.doi.org/10.19070/2332-2780-19000113
Copyright: Seydou T© 2019. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: The aim is to investigate the feasibility and advantages of intratracheal topical anesthesia with self-made tracheal topical anesthesia tube combined with isoflurane (ISO) inhalation in the intubation under unconscious and spontaneous breath in patients with giant goiter.
Methods: A total of forty-four patients undergoing general anesthesia during elective thyroidectomy were enrolled in our hospital. The patients with ASA grade I~II, aged 21~65 years, were randomly divided into group A (the self-made tube topical anesthesia group) and group B (those with the traditional topical anesthesia group). Each group was 22 cases. The SBP, DBP, MAP, HR, and SpO2 data and the indexes of evaluation during induction and postoperative intubation time, tidal volume (VT) during ISO induction, respiratory rate during ISO induction, level 4 score of cough during ISO induction, glottal score during intubation, score of mandibular slackness, score of difficulty in placement of laryngoscope, level 4 score of assessment of airway patency during ISO induction, level 5 score of tracheal intubation comfortability, level 3 score after endotracheal intubation, the different complications in the second day after surgery, postoperative memory sore and postoperative throat pain score were recorded.
Results: In the comparison of vital signs between the 2 groups: SBP, DBP, MAP and HR of group B were significantly higher than those of group A (P<0.05). In the comparison of vital signs in the same groups between before and after operation: SBP, DBP, MAP and HR of T2 in group A and group B were higher than those at T1 (P<0.05), and DBP and MAP in group A were higher than those at T3 (P<0.05). The SBP, DBP, MAP and HR in group B were higher than those at T3 (P<0.05). The SBP, DBP, MAP and HR of group B were higher than those at T5 (P<0.05). The hemodynamics during induction and intubation in group A are more stable than in group B. In comparison with the group B, the intubation time of group A was shorter (P<0.05), the tidal volume (VT) during ISO induction was larger (P<0.05), postoperative throat pain score was lower (P<0.05).
Conclusions: The self-made tube topical anesthesia is more complete than that on the traditional glottic and upper glottic area. The incidence and score of postoperative throat pain were lower in patients, which was higher in comfort and satisfaction than traditional methods.
2.Abbreviations
3.Introduction
4.Materials and Methods
5.Results
6.Discussion
7.Conclusions
8.References
Keywords
Topical Anesthesia; Unconscious; Spontaneous Breathing; Giant Goiter; Endotracheal Intubation.
Abbreviations: ASA
TV: Tidal Volume; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure; MAP: Mean Arterial Pressure; HR: Heart Rate; ECG: Electrocardiogram; BMI: Body Mass Index; MV: Minute Ventilation.
Introduction
Airway management is fundamental to the practice of anaesthesia and tracheal intubation is frequently required to ensure adequate airway control, while providing optimal operating conditions. Intubation by direct laryngoscopy is usually satisfactory. However, providing anaesthetic care to the patient with a difficult airway keenly interests anaesthesiologists. The African countries have a large number of patients with giant goiter. The giant goiter is easy to oppress or invade the trachea [2], causing tracheal stenosis, softening and displacement. The artificial airways are established by retaining spontaneous breath to prevent the risk in ventilation or tracheal intubation. The hospital lacks anesthetic drugs (only has some basic drugs), routinely performed 2% lidocaine on the glottis and glottic area topical anesthesia combined with intravenous, isoflurane (ISO) inhalation anesthesia to retain spontaneous breath for the tracheal intubation. This method is easy to cause serious hemodynamic fluctuations, which is under high risk, and low patient satisfaction. How to perform the topical anesthesia of the trachea, effectively reduce the stimulation of the ISO and the intubation to the trachea is the key to solve the above problems. In this type of patients with giant goiter, the cricothyroid membrane is often covered by thyroid masses. It is difficult to perform topical anesthesia through the thyrocricocentesis. Once a difficult airway occurs, it is even impossible to perform tracheotomy. Therefore, tracheal topical anesthesia tube ("self-made tube") was fabricated. The self-made tube can directly inject the local anesthetic into the trachea through the glottis to ensure the effect of the topical anesthesia of the tracheal mucosa. We compared the intratracheal topical anesthesia with self-made tube with the traditional method, and discuss the feasibility and advantages for the intubation under unconscious and spontaneous breath in patients of giant goiter.
Materials and Methods
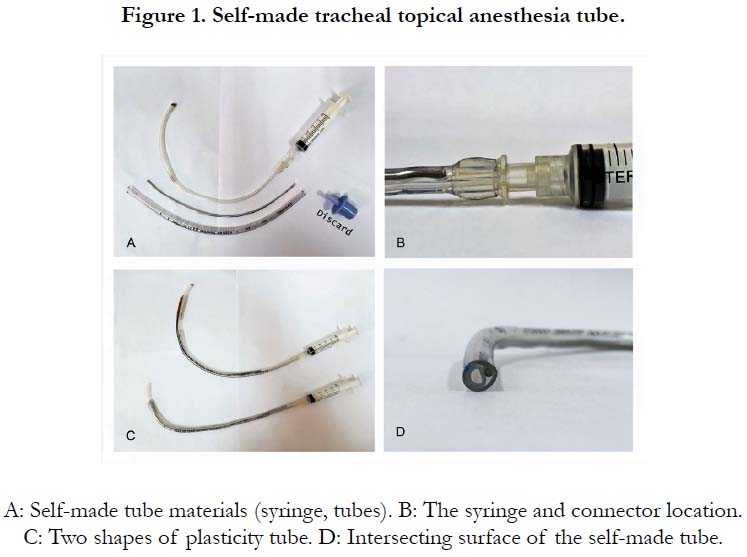
This study was approved by the ethics committee of the hospital and signed informed consent with the patient or his family. The trial was registered prior to patient enrollment at the local BIOMEDICAL ETHICS COMMITTEE. Principal investigator: Jincang Yuan, Date of registration: 12/11/2017. Forty-four patients with general anesthesia underwent elective thyroidectomy from September 2017 to October 2018. Patients were ASA grade I~II, aged 21~65 years. They were randomly divided into self-made tube topical anesthesia group (group A) and traditional topical anesthesia group (group B). Therefore, to achieve the experimental study, we make a "self-made tube" (Figure 1) depending to the existing conditions. We cut the 4.5# endotracheal tube and the infusion extension tube to the appropriate length and insert the infusion extension tube and metallic wire into the endotracheal tube. The front of the infusion extension tube is 1.5cm beyond the front of the endotracheal tube and the end of the infusion extension tube is connected to a syringe containing a local anesthetic. The self-made tube is randomly plasticized for different oral structures of the patient. Inclusion criteria was mouth opening≥ 3.0 cm; hyperthyroidism distance ≥ 6.0 cm; 18.5 ≤ body mass index (BMI) < 30; Plan and sign informed consent. Exclusion criteria was usual clinical manifestations of dyspnea and chest tightness, palpitation; history of asthma; major diseases of the circulatory system; severe abnormalities of liver and kidney function; neurological and psychiatric diseases; Sedative drugs were taken within 6 months. Fasting 12 hours before surgery and 6 hours of banned drinking; 30 min before surgery, the patient was given a topical anesthesia interpretation; we try to get the patient to cooperate fully and intramuscular injection of atropine 0.5mg was done. After installation, expelling the secretions of airway and oral, supine position, monitoring systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP), heart rate (HR), electrocardiogram (ECG), pulse oxygen saturation (SpO2) and open venous access were performed. Intravenous dexamethasone 10mg, midazolam 0.04mg/kg, fentanyl 1.5μg/kg, light buckle mask with oxygen flow 6L/min.
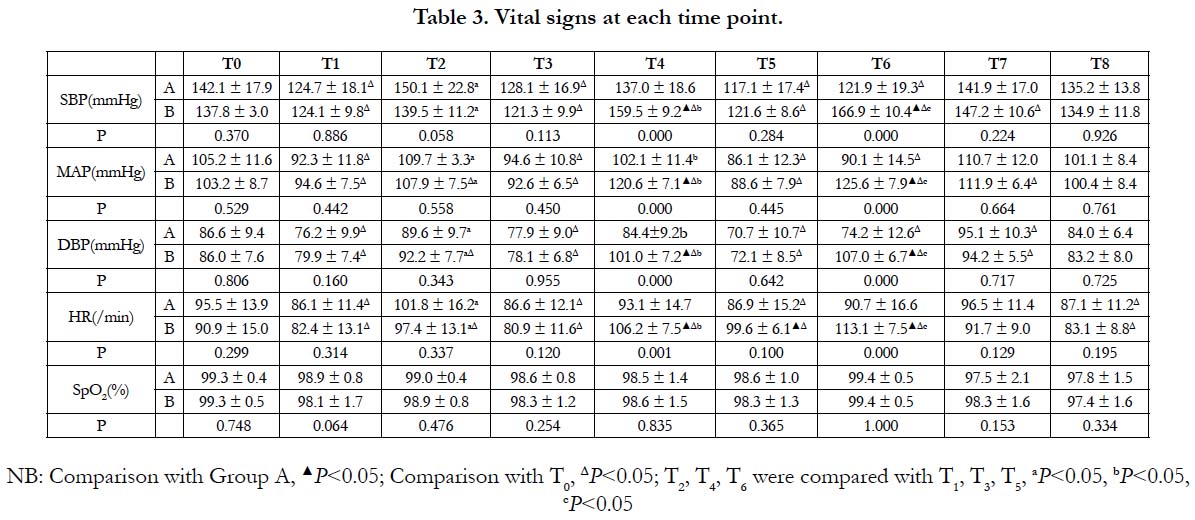
Patients in groups A and B were treated with 2% lidocaine, and the upper glottis area and the glottis area was sprayed three times through the mouth. The total amount of 2% lidocaine used in three sprays is 2-3 ml. In group A we used then a laryngoscope to uplift the epiglottis. When the glottis opened, the self-made tube was quickly placed 1 cm under the glottis and injected with 3ml of 2% lidocaine and then pulled out; the patient coughed, lidocaine was fully diffused inside, complete the mucosal topical anesthesia in the trachea. Both groups of patients were inducted with ISO increasing concentration inhalation after 3 minutes of topical anesthesia. The inhalation of vaporizer scale was 1.0% for 30s, 2.0% for 30s, 3.0% for 30s, 4.0% for 30s, 5.0% for 4min, then closed the vaporizer to complete the endotracheal intubation under the video laryngoscope, the monitor showed the PETCO2 waveform, adjusted the tracheal tube to a suitable depth and the intubation was confirmed to be successful. Then, vecuronium bromide (0.8 mg/kg) was intravenously injected and mechanical ventilation was performed after the disappearance of the breath. The oxygen flow was adjusted to 2 L/min. Topical anesthesia and endotracheal intubations of both groups were operated by the same doctor. If there is severe resistance after tracheal intubation, immediately intravenous anesthesia with propofol 1.0~2.0mg/kg was given to deep anesthesia. The observation indicators were the SBP, DBP, MAP, HR, and SpO2 data of T0, 10 min after installation, T1 before topical anesthesia, T2 peak of topical anesthesia, T3 before ISO inhalation, T4 peak of ISO inhalation, T5 before tracheal intubation, T6 immediately after tracheal intubation, T7 before tracheal extubation,T8 10 min after extubation were the indicators. T2 and T4 were recorded as peak vital signs during topical anesthesia and ISO inhalation.
The indexes of evaluation during induction and postoperative were recorded: Intubation time, VT during ISO induction, Respiratory rate during ISO induction, Cough score of level 4 during ISO induction, Glottal score of level 4 in intubation, Mandibular slackness, Easiness of laryngoscope insertion of level 4, Airway patency score of level 4 during ISO induction, Comfort score of level 5 in tracheal intubation, Evaluation score of level 3 after tracheal intubation, Memory in the second day after surgery, Score of pain of level 4 in the throat. Each evaluation index is recorded by the same doctor to reduce subjective differences in evaluation. The SPSS 22.0 statistical software was used for data processing. The measurement data were expressed as mean±standard deviation ( ±SD). Paired measurement data were compared using paired t-test. Simultaneous point comparison between the two groups was performed by One-way ANOVA, if the variance was not uniform. The Welch test was used; the multiple comparisons in the group were performed by LSD-t test. If the variance was not uniform, Dunnett's T3 test was used. The count data was compared by χ2 test and rank sum test. The single order data was analyzed by contingency table; P<0.05 was the difference with statistical significance.
Results
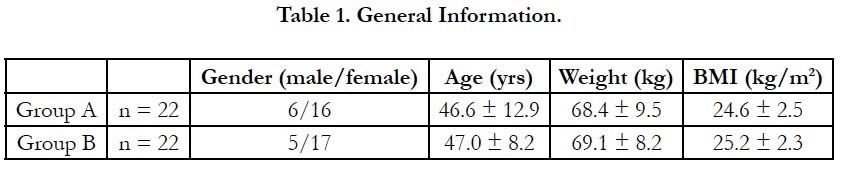
A total of 44 patients were enrolled in the study, 22 in group A and 22 in group B. There were no significant differences in gender ratio, mean age, mean body weight, and mean body mass index (BMI) between the two groups (Table 1).
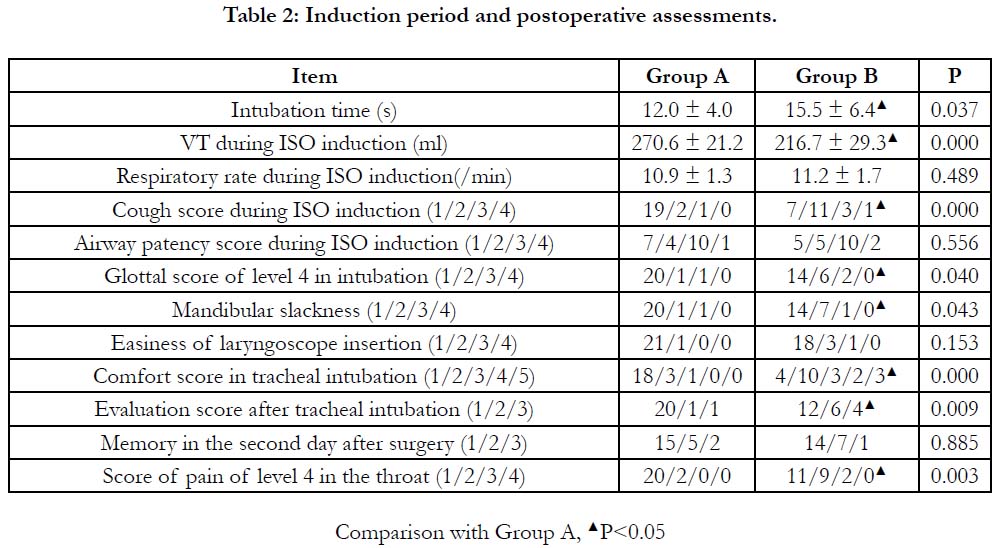
There were no significant differences in respiratory rate, airway patency, easiness of laryngoscopy insertion and memory scores in the second day after surgery between the two groups. Compared with group B, the intubation time of group A was shorter (P<0.05), the VT of ISO induction period was larger (P<0.05), and the cough score of ISO induction period was lower (P<0.05). The glottic opening was better (P<0.05), the mandibular slackness was better (P<0.05), the intubation comfort was better (P<0.05), and the intubation response was more mild (P<0.05). The pain score was lower (P<0.05) (Table 2). Three patients in the two groups had breath holding during the ISO induction process, including 1 patient in group A and 2 patients in group B. Both patients could maintain spontaneous breathing after opening the glottis with temporary hands-controlled ventilation. There were 5 cases with drastic reaction after intubation in the two groups, including 1 case in group A and 4 cases in group B, then performing anesthesia with propofol immediately.
4) All patients were intubated smoothly without difficult maskventilation and difficult intubation.
The results in comparison of vital signs at each time point were as follow.
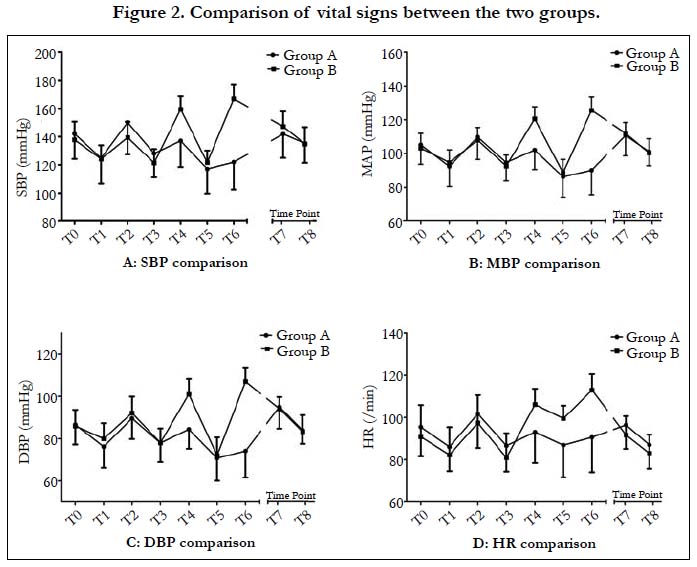
In comparison between groups: SBP, DBP, MAP and HR of group B in T4 and T6 were significantly higher than those in group A (P<0.05).
In comparison with T0: Group A: SBP, MAP, DBP of T1, T3, T5, T6 were lower than T0 (P<0.05), T7 DBP was higher than T0 (P<0.05), The HR of T1, T3, T5 and T8 were slower than T0 (P<0.05). Group B: SBP, DBP, MAP, HR of T1, T3 were lower than T0 (P<0.05), SBP, DBP, MAP, HR of T4, T6 were higher than T0 (P<0.05), DBP, MAP and HR of T2 were higher than T0 (P<0.05), SBP, DBP and MAP of T5 were lower than T0 (P<0.05), and HR of T5 was higher than that of T0 (P<0.05). SBP, MAP and DBP of T7 were higher than T0 (P<0.05), and HR of T8 was lower than T0 (P<0.05). In comparison between before and after operation: SBP, DBP, MAP and HR of T2 in group A and group B were higher than those in T1 (P<0.05); DBP and MAP of T4 in group A were higher than those in T3 (P<0.05), SBP, DBP, MAP and HR of T4 in group B were higher than those of T3 (P<0.05). There was no significant difference of the vital signs between T5 and T6 in group A (P>0.05). The SBP, DBP, MAP and HR of T6 in group B were higher than T5 (P<0.05) (Table 3). There was no statistically significant difference in SpO2 between the two groups.
Discussion
In The standard for the classification of giant goiter [3]: the cricoid cartilage could not be touched in upper goiter, or the lower part is located in the thorax, or the trachea is displaced by >10 mm, or there is tracheal stenosis according to the X-ray. Reported in the literature [4], about 11% of patients with goiter combined with tracheal compression, combined with tracheal softening accounted for 0.04~17.1%. The giant goiter causes tracheal compression, displacement and softening, and the risk/crisis of “can’t intubate, can't oxygenate” (CICO) easily occurs under rapid sequential induction. “Difficult airway society 2015 guidelines for the management of unanticipated difficult intubation in adults” [5] pointed out that once CICO occurs, it should be immediately subjected to thyrocricocentesis. However, because the patient's cricothyroid membrane is usually covered by goiter, it can not only perform a tracheotomy, or even perform a thyrocricocentesis, which endangers the patient's life safety. The Chinese Society of Anesthesiology Airway Management Group issued the "Difficult Airway Management Guide" [6] pointed out that the foreseeable difficulty of the airway should try to keep the endotracheal intubation under spontaneous breathing to prevent the predictable difficult airway from becoming an emergency airway.
Studies have shown that [7], the intratracheal mucosa is a region that is more susceptible to irritation and cough response than the glottis and throat, so comprehensive and effective topical anesthesia for the trachea is very important. The usual method is thyrocricocentesis. This method is invasive, easily causes mental stress and fear, and is easy to provoke patients with cough, bronchospasm and cardiovascular reactions. If improperly operated, subcutaneous and mediastinal emphysema or even tracheoesophageal fistula may occur. Patients with giant goiter are often difficult to perform a thoracentesis.
Completing the operation of inserting the glottis and injecting the local anesthetic merely by single hand "British Thoracic Society 2001 Guidelines" [8] recommended that the total amount of lidocaine should be limited to 8.2 mg/kg during bronchoscopy, while the maximum estimated amount of lidocaine to 9.0 mg/ kg did not reach the poisoning concentration of plasma. In this study, the amount of lidocaine used in groups A and B (<3.0 mg/ kg) was much lower than this standard, which could avoid the risk of lidocaine toxicity.
The BP and HR of the two groups were higher than those before the operation of tropical anesthesia, and the difference was statistically significant (P<0.05). Patients in group A accepted intratracheal tropical anesthesia in addition and had more airway irritation during topical anesthesia well-regulatedly, but the difference between the two groups was not statistically significant (P>0.05). Maybe during the topical anesthesia of the glottis and throat, the lidocaine spray stimulated the throat and glottis area, or the front of the throat sprayer touched the root of the tongue and the throat caused vomiting and coughing, which caused the BP and HR of the patient to increase significantly. The operation of performing intratracheal topical anesthesia with self-made tube in the group A is rapid and convenient. Reasonable shaping can effectively reduce touch with the oral cavity and throat tissue and avoid stimulation. Combined with effective intravenous sedation and analgesia, it effectively avoids excessive hemodynamic fluctuations during intratracheal topical anesthesia.
The rational use of sedative and analgesic drugs is essential for the retention of adequate spontaneous breathing. It’s only available with midazolam and fentanyl as sedative and analgesic drugs in our hospital, and midazolam has an anterograde amnesia effect. Alexander CM [9] have shown that intravenous infusion of 0.1mg/kg midazolam has no significant respiratory inhibition but Bailey [10] showed that midazolam 0.05mg/kg combined with fentanyl 2μg/kg can cause severe hypoxemia (11/12) and asphyxia (6/12). It has been reported that midazolam and opioid combination can increase the efficacy by up to 8 times [11]. Gao Chao [12] have shown that the median effective dose (ED50) of midazolam resulting in amnesia is 0.031mg/kg( 95% CI:0.027mg/ kg~0.036mgkg); Under intravenous injection of midazolam of 0.04mg/kg, the respiratory and circulatory system was basically stable, no serious adverse events occurred, and the ratio of amnesia was 88.5%. Referring to the above data, the study finally selected midazolam 0.04mg/kg combined with fentanyl 1.5μg/kg for intravenous sedation and analgesia, all patients could maintain the status of SpO2>95% before ISO inhalation.
However, ISO is highly irritating [13, 14], which can directly or indirectly activate the bulbus medulla center through airway stimulation receptors, resulting in increasing sympathetic output and its stimulation intensity is positively correlated with the inhalation concentration [15]. Rapidly increasing the inhalation concentration of isoflurane can easily cause adverse reactions such as cough, breath holding, and body movement. Increasing concentration inhalation of ISO can not only effectively reduce the incidence of adverse reactions but also gradually observe the patient's respiratory changes as the inhalation concentration increases. If there is insufficient ventilation, the inhalation concentration can be lowered or the inhalation can be stopped in time to ensure safety of the patient's airway. One patient in group A and two patients in group B had a breath holding when inhaling 5% ISO. After using the manual breathing several times to open the glottis, they could resume spontaneous breath. No throat spasm and apnea occurred. The rest of the patients could keep the airway open by the neck hypso kinesisk, uplifting jaw or placing a oropharyngeal airway.
Group A had better airway topical anesthesia than group B. The glottis and trachea were relatively less stimulated by ISO, which may cause the glottic opening area to be larger than that of group B; the tracheal contracture was lower at the same time, so the VT was larger than that of group B and there was no significant difference in respiratory rate between the two groups during the induction period (P>0.05). Therefore, the minute ventilation volume (MV) of group A was larger than that of group B. According to the following formula:
EtAG [16] = InAG - FGF × (VaAG - EtAG)/MV( EtAG: concentration of end-tidal anesthetic gas; InAG: concentration of inhalating anesthetic gas; FGF: fresh gas flow; VaAG: concentration of anesthetic gas from vaporizer; MV: minute ventilation volume.) It can be seen that in the induction phase of anesthesia, under the same conditions, the MV is larger; the concentration of end-tidal anesthetic gas (EtGas) is closer to the concentration of inhaled anesthetic gas, so the ISO concentration is higher in group A than in group B, resulting in less coughing during ISO inhalation. The glottal condition is better in the intubation. The mandibular slackness is better and the intubation time is shorter. The better glottal condition in group A may also be related to the self-made tube topical anesthesia which makes the vocal cord more fully topical anesthesia.
Isoflurane, similar to other inhaled anesthetics showed a dosedependent decrease in MAP, HR and inhibition of arterial baroreflex [17]. According to the inhalation protocol of this study, in group A the MAP of patients decreased comparing to the baseline level from the beginning of ISO inhalation to intubation ,but they were all within the clinical safety range and the range of decline was within 25% of the baseline value. In group B the MAP when inhaling ISO and intubating were significantly higher than the baseline value and the difference was statistically significant (P<0.05). The MAP at the other time points was lower than the baseline value within 20%.
In comparison of the vital signs between after and before ISO inhalation, SBP, MAP, DBP, and HR in group A increased by 6.9%, 7.9%, 8.3%, and 7.5% respectively. In group B, they increased by 31.5%, 41.0%, 29.3%, and 31.3%. We compared the vital signs of endotracheal intubation with before intubation in Group A, SBP, MAP, DBP, and HR increased by 4.1%, 5.8%, 5.0%, and 5.5% respectively; In Group B they increased by 37.2%, 41.8%, 48.4%, and 13.6% (Figure 2). Compared with group B, ISO inhalation and endotracheal intubatioin in group A stimulated the airway less, and the hemodynamics during induction period was more stable.
Endotracheal intubation can cause stimulation of the pharynx and tracheal distal nerves, which can lead to an increase in sympathetic output, resulting in increase of patient's blood pressure and heart rate and even change the state of consciousness [18]. The subglottic trachea is an area that is prone to cough stimulation. Reducing subglottic stimulation can effectively reduce the incidence of cough response [7]. There were 2 cases of severe cough and 3 cases of limb confrontation in group B and no occurrence in group A by comparison. In group B, 4 cases of severe resistance occurred after intubation, which needed to perform general anesthesia with propofol and muscle relaxant immediately and only 1 case occurred in group A. This is due to its well-established intratracheal topical anesthesia. In group A, cough response during inhalation and glottal conditions, body movement and cough during intubation were better than those in group B. Therefore, the injury to the throat and vocal cords was slighter. Only 2 cases of mild sore throat occurred in group A, 9 cases of mild sore throat and 2 cases of moderate sore throat occurred in group B. There was no unspeakable severe sore throat in both groups.
There were 5 cases of painless memory and 2 cases of painful memory in group A, 7 cases of painless memory and 1 case of painful memory in group B but there was no significant difference in the overall score of memory between the two groups after operation (P>0.05). The patients reported that their bad memory occurred during topical anesthesia and did not occur during ISO inhalation and tracheal intubation, which was related to not only the midazolam and fentanyl but also isoflurane which is with hypnotic and analgesic effects.
The loss of consciousness may be related to the following two aspects: 1) directly acting on the spinal cord to inhibit the transmission of external impulses into the thalamus and cerebral cortex, thereby weakening the arousal stimulation intensity of the cerebral cortex and leading to the disappearance of consciousness; 2) indirectly acting on the thalamus, midbrain reticular formation and cerebral cortex and leading to the disappearance of consciousness [19]. It’s analgesic effect is mainly mediated by the spinal cord. Although the mechanism of action is not completely clear, it is currently thought to be related to NMDA receptors, GABA receptors, glycine receptors and nicotinic receptors, by enhancing inhibitory neurotransmitters and /or inhibiting excitatory neurotransmitters [20, 21].
There was no significant difference in blood pressure and heart rate between the A and B groups before and after extubation (P>0.05). The duration of 2% lidocaine in airway topical anesthesia is about 15-30 minutes [22], the operation time of goiter in this study is more than 60 mins, and the effect of airway topical anesthesia is over until the end of surgery.
Intramuscular injection of atropine before installation, expelling the secretions of trachea and oral cavity before performing the topical anesthesia, keeping it dry allows patients to get better anesthesia. Related literatures [23] show that, video laryngoscope has large mobility and good visibility. Compared with ordinary laryngoscope, it can reduce the difficulty of endotracheal intubation. The stimulation of compression on the root of the tongue and throat is smaller, the nausea, vomiting reaction and cardiovascular stress are slighter, which is the first choice for tracheal intubation, which ensured smooth and successful operation.
Conclusion
The topical anesthesia is more perfect in the self-made tube topical anesthesia group than the traditional topical anesthesia group. Under the premise of ensuring the safety of airway in patients with giant goiter, the stimulation of airway is effectively reduced, so that patients have greater MV and better inhalation anesthesia, ensuring more stable hemodynamics and fewer adverse reactions during induction. The patient was completely unconscious during endotracheal intubation, which was more satisfactory and comfortable than traditional awake intubation.
References
- WHO . World Health Statistics 2015. 2015;7:125-135.
- Luo Jun. Report of 6 cases of sudden asphyxia in perioperative thyroid gland. Chin J Modern Oper Surg. 2002;6(1):78-78.
- Mallat J, Robin E, Pironkov A, Lebuffe G, Tavernier B. Goitre and difficulty of tracheal intubation. InAnnales francaises d'anesthesie et de reanimation. 2010. Elsevier Masson. 2010 Jun 1;29(6):436-439.
- Shang Kaizhen, Xia Zongjing, Zhang Wei. Airway management and literature review of giant goiter resection in Tibetan areas. Tibet Med. 2017;6:50.
- Hagberg CA, Gabel JC, Connis RT. Difficult Airway Society 2015 guidelines for the management of unanticipated difficult intubation in adults: not just another algorithm. Br J Anaesth. 2015 Dec;115(6):812-4. doi: 10.1093/bja/aev404. PubMed PMID: 26556850.
- Yu Buwei, Wu Xinmin, Zuo Mingzhang. Guidelines for difficult airway management. J Clin Anesth. 2013;29(1):93-98.
- Xu JQ, Ye TH, Huang YG, Luo AL. Application of propofol target controlled infusion combined with dribbled and nebulized lidocaine in tracheal intubation under spontaneous respiration. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2010 Oct;32(5):569-73. doi: 10.3881/j.issn.1000-503X.2010.05.020. PubMed PMID: 21050564.
- Woodall NM, Harwood RJ, Barker GL. Complications of awake fibreoptic intubation without sedation in 200 healthy anaesthetists attending a training course. Br J Anaesth. 2008 Jun;100(6):850-5. doi: 10.1093/bja/aen076. PubMed PMID: 18424806.
- Alexander CM, Gross JB. Sedative doses of midazolam depress hypoxic ventilatory responses in humans. Anesth Analg. 1988 Apr;67(4):377-82. PubMed PMID: 3354874.
- Bailey PL, Pace NL, Ashburn MA, Moll JW, East KA, Stanley TH. Frequent hypoxemia and apnea after sedation with midazolam and fentanyl. Anesthesiology. 1990 Nov;73(5):826-30. PubMed PMID: 2122773.
- Riley ET, Walker D, Hamilton CL, Cohen SE. Intrathecal sufentanil for labor analgesia does not cause a sympathectomy. Anesthesiology. 1997 Oct;87(4):874-8. PubMed PMID: 9357890.
- Gao Chao, Yan Jing, Yue Yun. Determination of half effective dose and duration of amnesium for amnesia 2012 National Youth Anesthesiologist Academic Forum. 2012.
- Pandit UA, Steude GM, Leach AB. Induction and recovery characteristics of isoflurane and halothane anaesthesia for short outpatient operations in children. Anaesthesia. 1985 Dec;40(12):1226-30. PubMed PMID: 4083453.
- Wren WS, McShane AJ, McCarthy JG, Lamont BJ, Casey WF, Hannon VM. Isoflurane in paediatric anaesthesia: induction and recovery from anaesthesia. Anaesthesia. 1985 Apr;40(4):315-23. PubMed PMID: 4003734.
- Ebert TJ, Muzi M. Sympathetic hyperactivity during desflurane anesthesia in healthy volunteers. A comparison with isoflurane. Anesthesiology. 1993 Sep;79(3):444-53. PubMed PMID: 8363068.
- Zhao Jun. New Anesthesiology. Beijing: People's Military Medical Press. 2002;272.
- Zhang Yu, Yao Wei, Kong Gaoyin. Application of sevoflurane slow induction general anesthesia in uvulopalatopharyngoplasty in patients with obstructive sleep apnea syndrome. Modern Med. 2013;1:1-3.
- Guignard B, Menigaux C, Dupont X, Fletcher D, Chauvin M. The effect of remifentanil on the bispectral index change and hemodynamic responses after orotracheal intubation. Anesth Analg. 2000 Jan;90(1):161-7. PubMed PMID: 10624998.
- Yan Mei, Dai Tijun. The relationship between analgesic and hypnotic effects of inhaled anesthetics and GABA receptors. Chin J Pharm. 2004;20(5):521-523.
- Dai Tijun, Yu Tian. Anesthetic pharmacology. 3rd edition. Beijing People's Medical Publishing House; 2005. p. 43-72.
- Zhou Meiyan, Dai Tijun. Advances in research on the mechanism of analgesic and hypnotic receptors in inhaled anesthetics. J Xuzhou Med Coll. 2010;30(5):346-348.
- Cavallone LF, Vannucci A. Extubation of the difficult airway and extubation failure. Anesth Analg. 2013 Feb;116(2):368-83. doi: 10.1213/ANE.0b013e31827ab572. PubMed PMID: 23302983.
- Xue FS, Zhang GH, Li XY, Sun HT, Li P, Li CW, et al. Comparison of hemodynamic responses to orotracheal intubation with the GlideScope® videolaryngoscope and the Macintosh direct laryngoscope. J Clin Anesth. 2007 Jun;19(4):245-50. PubMed PMID: 17572317.