Annular Lichen Planus with Central Clearing
Julia Accetta1, Dylan Conroy2, Thomas N. Helm3*
1.The George Washington University, Washington DC, USA
2. Canisius College, Buffalo NY, USA
3.Buffalo Medical Group, Buffalo NY, USA
*Corresponding Author
Thomas N. Helm MD,
Buffalo Medical Group,
Department of Dermatopathology,
6225 Sheridan Drive, street 208, Bidg B,
Williamsville, New York 14221, USA.
Tele: (716) 630-2582; Fax: (716) 630-2594.
E-mail: jlaccetta@gmail.com (point of contact)
Article Type: Case Report
Received: September 03, 2014; Accepted: September 29, 2014; Published: September 30, 2014
Citation: Julia Accetta, Dylan Conroy, Thomas N. Helm (2014) Annular Lichen Planus with Central Clearing. Int J Clin Dermatol Res. 2(6), 37-39,
doi: dx.doi.org/10.19070/2332-2977-1400011
Copyright: Thomas N. Helm© 2014. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Annular lichen planus is an uncommon clinical variant of lichen planus. Characteristics include an annular configuration associated with a narrow rim of erythema and inflammation and a depressed center. There is a tendency toward central clearing. We present an illustrative case of annular lichen planus in an 82-year-old woman.
2.Patient History
3.Discussion
4.Conflict of Interest Statement
5.References
Keywords
Lichen planus, Annular lichen planus, Dermatosis.
Patient History
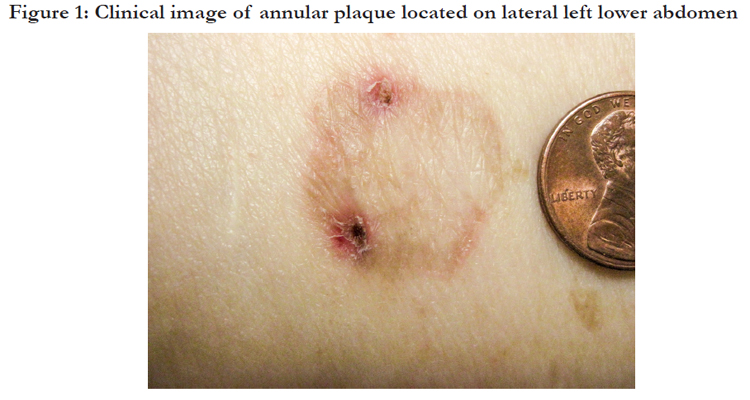
An 82 year-old white woman with a history of basal cell carcinoma presented for routine follow up and was noted to have a 2.5 cm hyper-pigmented annular plaque on her left lower abdomen. She reported that the plaque had been present and stable for over one year. Examination also revealed small hyperpigmented macules in her right axilla. The remainder of her skin exam, including her buccal mucosa and nails, was unremarkable. Her past dermatologic history was significant for scalp psoriasis, which responded to topical steroids and had remained in remission for several years. Three biopsies were obtained, two from the larger annular plaque and one from an axillary lesion. All demonstrated histologic findings consistent with lichen planus. A review of her medications failed to identify mediations associated with lichenoid drug eruptions.
Discussion
Lichen planus is an inflammatory dermatosis involving the skin and mucous membranes characterized by an autoimmune reaction mediated by CD8+ T cells [1].Several variants of lichen planus are recognized and all may exhibit differing features during acute or chronic phases (Table 1). Although annular lichen planus (ALP) is a long-recognized clinical variant of lichen planus, it is rare. Tinea, granuloma annulare, porokeratosis, mycobacterial infection, figurate erythema, borrelia infection, as well as other annular eruptions all need to be considered in the histologic differential diagnosis. Furthermore, ALP may present with striking central atrophy, which is typically classified as annular atrophic lichen planus [2]. A retrospective review of 20 patients identified the distribution and presentation of annular lichen planus and found that the morphology typically included violaceous plaques with an annular configuration and a narrow rim of activity and residual hyperpigmentation [3]. ALP commonly involves the male genitalia and intertriginous areas such as the axilla and groin folds [4]. In addition, characteristic oral mucosal, vulval, scalp or nail lesions that are associated with other variants of lichen planus are typically absent in ALP. Similarly, pruritus, a symptom that occurs often in typical lichen planus, is very slight or altogether absent in ALP, with recurrence and aggravation related to long exposure to sunlight [5].
Our patient’s presentation and clinical course are typical and illustrative. She presented with an annular lesion with indurated borders and a tendency toward central clearing (Figure 1). Biopsy captured the inflammatory component of both sides of the annular rim as well as the quiescent midline area. Microscopic examination revealed a patchy lichenoidlymphohistiocytic inflammatory infiltrate with melanophages in the papillary dermis. Discrete areas demonstrated lichenoid inflammation (Figure 2a). Higher power revealed typical hypergranulosis with dyskeratotic keratinocytes and a band-like lymphocytic infiltrate (Figure 2b). Eosinophils and plasma cells were not conspicuous within the inflammatory infiltrate. The histologic findings confirmed the clinical diagnosis of ALP. Mainstays of therapy include topical corticosteroids. In our patient, the lesions were asymptomatic and not cosmetically apparent, and so the patient elected to forgo treatment.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Roopashree MR, Gondhalekar RV, Shashikanth MC, George J, Thippeswamy,SH, et al(2010). Pathogenesis of oral lichen planus–a review. J Oral Pathol Med;39(10):729-734.
- Sugashima Y, Yamamoto T (2012). Annular atrophic lichen planus of the lip. Dermatol Online J;18(2).
- Sakakibara K, Nakada T, Sueki H, Irisawa K (2004). Annular lichen planus. J Cutan Med Surg.;8(3):173-175.
- Reich HL, Nguyen JT, James WD (2004). Annular lichen planus: a case series of 20 patients. J Am AcadDermatol.;50(4):595-599.
- Katzenellenbogen I (1962). Lichen planusactinicus (lichen planus in subtropical countries). Dermatology;124(1):10-20.
- Salman SM, Kibbi AG, Zaynoun S (1989). Actinic lichen planus: a clinicopathologic study of 16 patients. J Am AcadDermatol.;20(2):226-231.
- Wagner G, Rose C, Sachse M (2013). Clinical variants of lichen planus. J DtschDermatolGes,;11(4):309-319.
- Friedman DB, Hashimoto K (1991). Annular atrophic lichen planus. J Am AcadDermatol.;25(2):392-394.
- Gunduz K, Sacar T, Inanir I, Demireli P (2009). Flexural follicular lichen planus. ClinExpDermatol;34(7):e297-e298.
- Rieder E, Kaplan J, Kamino H, Sanchez M, Pomeranz MK (2013). Lichen planuspigmentosus. DermatolOnline J;19(12).
- Cram DL,Kierland R, Winkelmann RK(1966). Ulcerative lichen planus of the feet: bullous variant with hair and nail lesions. Arch Dermatol.; 93(6):692-701.