Hypersensitivity to Latex Gloves among Dental Students: Is the Pre-Matriculation Evaluation and Periodic Health Surveillance Necessary?
Bakiri A1,2,3, Skenderaj S4, Kraja D5, Petrela E6, Mingomataj D2, Mingomataj Ç2, Rama A1, Mingomataj EÇ7,8*
1 Logos University, Faculty of Applied Sciences, Department of Advances Technics in Medical Laboratory, Tirana, Albania.
2 Albanian University, Faculty of Medical Sciences, Department of Stomatology, Tirana, Albania.
3 Hygeia Hospital Tirana, Department of Outpatients Service, Tirana, Albania.
4 Medicine University of Tirana, Faculty of General Medicine, Department of Environmental and Work Medicine, Tirana, Albania.
5 Medicine University of Tirana, Faculty of General Medicine, Department of Infective and Dermato-Venerologic Diseases, Tirana, Albania.
6 Medicine University of Tirana, Faculty of General Medicine, Department of Statistics and Epidemiology, Tirana, Albania.
7 Medicine University of Tirana, Faculty of Technical-Medical Sciences, Department of Paraclinical Disciplines, Tirana, Albania.
8 Mother Theresa School of Medicine, Department of Allergology and Clinical Immunology, Tirana, Albania.
*Corresponding Author
Ervin Ç. Mingomataj,
Mother Theresa School of Medicine,
Department of Allergology and Clinical Immunology, Tirana, Albania.
E-mail: allergology@gmx.de
Received: January 31, 2017; Accepted: March 03, 2017; Published: March 07, 2017
Citation: Bakiri A, Skenderaj S, Kraja D, Petrela E, Mingomataj EÇ, et al., (2017) Hypersensitivity to Latex Gloves among Dental Students: Is the Pre-Matriculation Evaluation and Periodic Health Surveillance Necessary?. Int J Clin Med Allergy. 5(1), 55-64. doi: dx.doi.org/10.19070/2332-2799-1700011
Copyright: Mingomataj EÇ© 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Latex allergy is a common occupational disease among healthcare workers who use latex gloves. Self-administrated questionnaires, physical examination and diverse allergic tests are largely used to assess data about natural history, risk factors, type of allergic reaction, etc. The aim of the present study was to determine the prevalence of allergy to latex gloves among dental students.
In this prospective study, a total of 240 students separated as non-exposed, shortly-exposed and longer-exposed during school practice completed a self-administrated questionnaire that comprised of a total of different items and gave information about the participants and their glove use, working habits and glove use, signs and symptoms related to glove use, precautions taken to minimize it, etc. Challenge and patch tests were performed through latex gloves, skin prick test with commercial extracts.
Questionnaire items and diagnostic tests revealed that one-fourth of subjects were suspicious for latex gloves hypersensitivity. Their mean value for skin reactions like contact urticaria, irritant or allergic dermatitis was between 10% and 14%, while for other symptoms the mean value was under 5%. In general, students who experienced latex exposure over 2 years during their school practice have shown about a two-fold positive response for statements or diagnostic tests about latex gloves hypersensitivity. Also the Kendall tau coefficient progressed from non-exposed group to longer-exposed one for the majority of items.
Because of relationship between allergic reactions to latex gloves and some medical histories, it seems to be necessary for pre-matriculation evaluation and periodic health surveillance of dental students.
2.Method
3.Results
4.Discussion
5.References
Introduction
Latex allergy is a common occupational disease among healthcare workers who use latex gloves, whose prevalence has reached epidemic proportions in highly exposed populations [1-3]. The use of latex gloves by healthcare workers can lead to multiple symptoms: eczema, contact urticaria, rhinitis, conjunctivitis, asthma, and anaphylaxis [4, 5]. Diagnosis of latex allergy is based on personal history, physical examination, skin prick tests, specific IgE, patch test and challenge test, while self-administrated questionnaires are largely used to assess the respective data about natural history, risk factors, etc [6-9].
Today, gloves are worn routinely by many dental practitioners while treating patients, with natural rubber latex being the most commonly used glove material worldwide [10]. There is lack of data on the prevalence of latex allergy in the dental care setting in Albania. The aim of the present study was to determine the prevalence of allergy to latex gloves among dental students in the Albanian University of Tirana, Albania, and its correlation to different factors (obtained by questionnaire and diagnostic tests).
Method
In this prospective study, a total of 240 students (42% males and 58% females, mean age 22.8 ± 3.4 years) were first surveyed using a self-administered questionnaire during academic years 2012-2013 and 2013-2014. The questionnaire was comprised of different items and gave information about the participants in regard to working habits, their glove use, concentration on the work, previous chirurgical interventions, signs and symptoms related to latex gloves usage, any other type of allergy, symptoms associated with toy balloons, familiar atopy and tobacco smoking, as well as precautions taken to minimize it. According to latex gloves exposure during school practice, population was classified in three groups: as non-exposed (n=33), exposed for a few months (shortly exposed, n=136), and exposed for a longer period than two years (longer exposed, n=71). Apart from questionnaire (completed by all subjects), prevalence of latex-related symptoms and sensitization was determined in a randomized sample of students by commercial skin prick tests (Stallergenes), patch tests with natural rubber glove (including latex-free glove as control), as well as through challenge test with dermal and airborne exposure to nature rubber latex and latex-free gloves. Similarly to self-administrated questionnaire, the challenge test has been performed by all students.
The suspected cases for adverse reactions during latex exposure were further classified as irritant skin reactions (dried skin, localized erythema, adverse reactions to detergents or disinfectants - mentioned on disease history questionnaire items and confirmed during challenge test, but lack of positive or relevant results for the latex allergy tests), allergic skin reactions (diverse allergy skin reactions like erythema, eczema/cracked hands, hives, angioedema, associated with positive results for latex allergy tests), and internal organs allergic reactions (breathlessness attacks, cough, rhinitis and/or conjunctivitis symptoms, arterial hypotension, associated by positive tests for latex allergy).
Comparisons were made between the different variables by Fisher’s exact test and Kendall´s tau correlation coefficient.
Results
A natural rubber latex allergy was reported by 10% of subjects, reaching about 20% in students who were longer exposed (p< 0.003). Ninety-five percent of students were regular users of natural rubber gloves, and 60% of subjects used latex-free gloves when possible. Hand erythema along work procedures was observed in about 10% of cases and a short-term one developed (immediately after gloves wearing) in more than 12% of cases showing a progressive trend up to 21% (p < 0.03).
About 14% of subjects reported for irritant dermatitis after hand wash or washout procedures, reaching a value over 22% in the longer exposed group (p < 0.02). About 10% of subjects complained for irritant symptoms after application of disinfectants.
Hand eczema within two days after natural rubber latex gloves use is reported by 14% of subjects, reaching a value of 28% in the longer exposed subpopulation (p < 0.0003).
Immediate facial allergic symptoms, rhino-conjuctival symptoms, lower respiratory symptoms, and visit of emergency services after latex exposure were reported by 5%, 5.4%, 2.5% and 7.1% of subjects respectively.
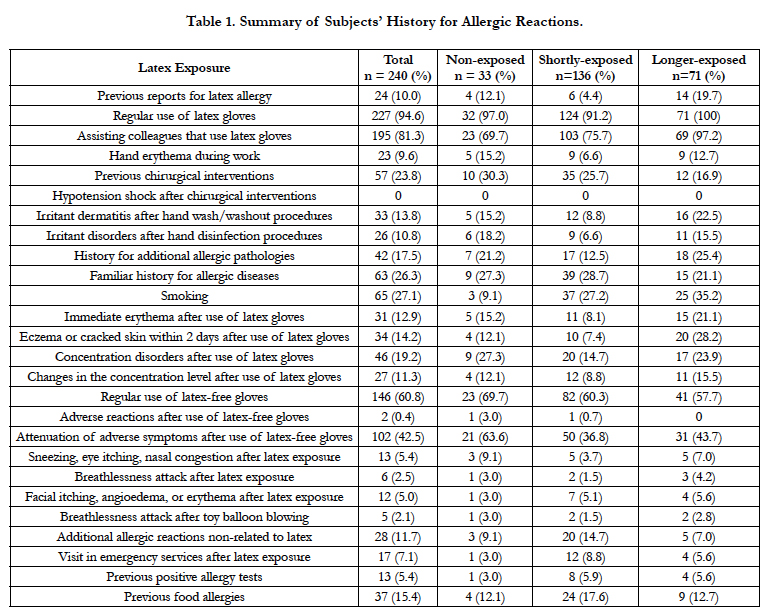
More than 20% of subjects were exposed to chirurgical procedures (like dental extractions). Dyspnea after toy balloon blowing is reported in about 2% of cases. Concentration disorders or oscillations are reported by 10%-20% of subjects. About one-quarter of subjects were tobacco smokers. Only 2 subjects complained for adverse reactions from latex-free gloves, while more than 40% of all subjects reported for attenuation of them during their regular use. At least 11% of subjects reported for allergic reactions independent to the latex exposure on workplace. Additional allergic pathologies and familiar history for such diseases reported about 17% and 26% of subjects respectively. In addition, 15% of subjects reported for food allergies. One-third of latex-independent allergic pathologies (5.4%) were confirmed by allergy tests. These findings are summarized on Table 1.
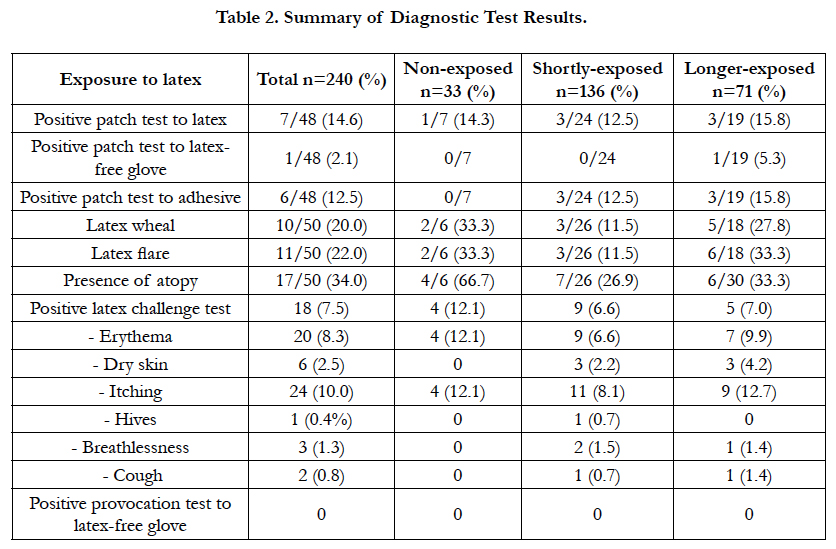
With regards to diagnostic procedures, the patch test to latex resulted positive in about 15% of subjects. More than 12% of subjects showed a positive reaction to adhesive of patch test (one subject with parallel sensitivity to latex-free glove, and one other to latex). Commercial skin prick test to latex revealed a sensitization to latex on 20% and atopy (a positive result to airborne and/ or food allergens) on 34% of subjects. Airborne challenge with natural rubber latex gloves confirmed the allergic sensitization on 7.5% of subjects, which was reinforced by parallel negative results to challenge with latex-free gloves. An additional population showed irrelevant or irritant skin symptoms (like itching, erythema or dried skin), while respiratory allergic symptoms are shown in a few cases. For more information see Table 2.
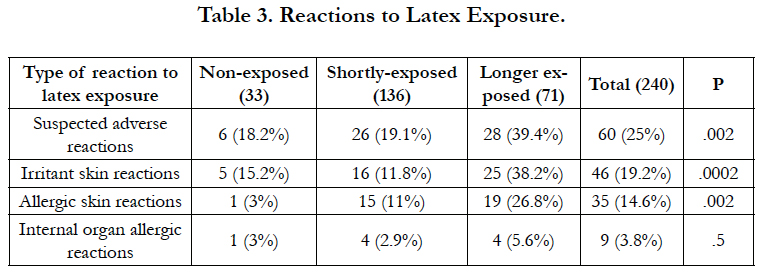
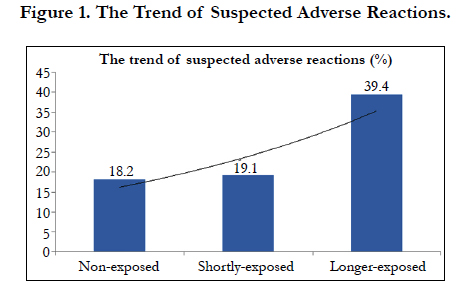
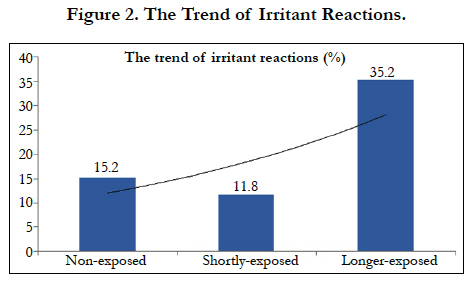
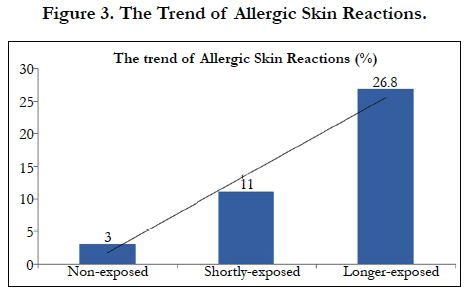
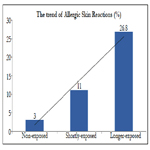
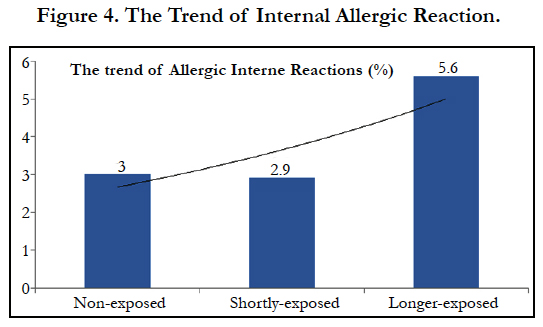
In total, 25% of subjects (60 cases) were suspected for adverse reactions during natural rubber latex exposure. According to school practice grouping, in the non-exposed group were suspected 6 cases (18.2%), in the shortly-exposed group 26 cases (19.1%), and in longer exposed group were suspected 28 cases (39.4%, p < 0.002). With respect to irritant contact reactions, these values were 15.2%, 11.8% and 35.2% respectively (p < 0.0002). Regarding allergic reactions on the skin, the respective values were 3%, 11% and 26.8% (p < 0.002). With respect to allergic symptoms manifested on internal organs, these values were 3%, 2.9% and 5.6% (ns) (see also Table 3, and Figures 1, 2, 3, 4).
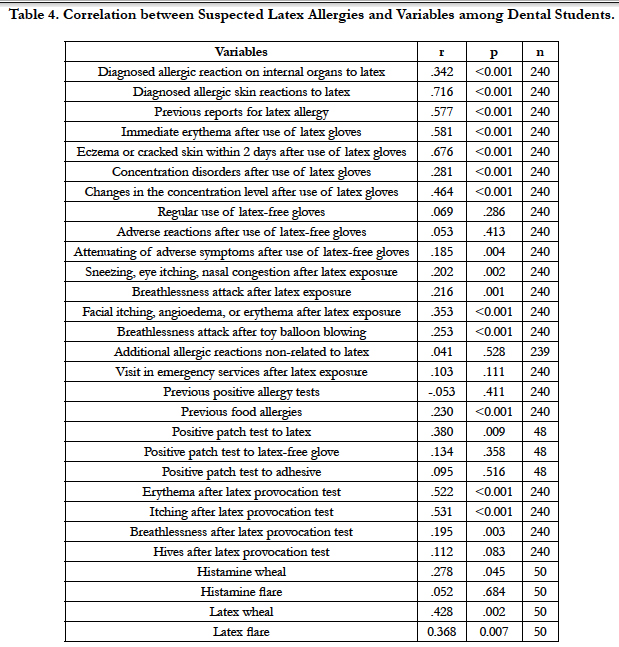
With regards to correlation between studied variables and the suspicion of natural rubber latex allergy, our findings revealed consistent to strong links to confirmed allergy, self-reporting of latex allergy, hand erythema or eczema, changes in concentration level, occurrence of skin allergic symptoms after latex exposure, attenuation of symptoms during regular use of latex-free gloves, occurrence of allergic skin symptoms during challenge test or positive result for latex skin prick and patch tests. A less consistent but significant correlation is observed between the suspicion of latex allergy and some variables like self-observation of respiratory symptoms after latex exposure, observation of the same symptoms during challenge test, attenuation of symptoms during regular use of latex-free gloves, or history for food allergy (see also Table 4).
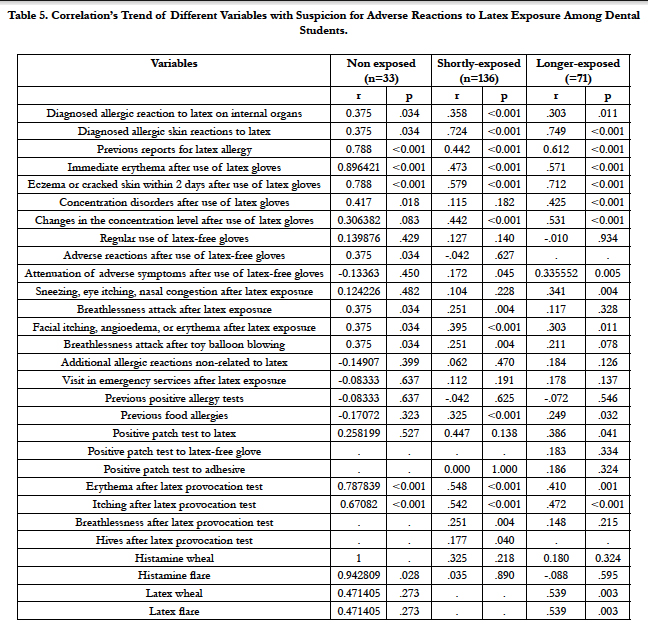
The majority of mentioned correlations were observed according to student practice grouping. A progressive trend on these correlations is observed with regards to diagnosed skin allergy (including skin prick and patch tests), occurrence of concentration’s disorders, the attenuated symptoms after regular use of latex-free gloves, and history for food allergy (see also Table 5).
Table 5. Correlation’s Trend of Different Variables with Suspicion for Adverse Reactions to Latex Exposure Among Dental Students.
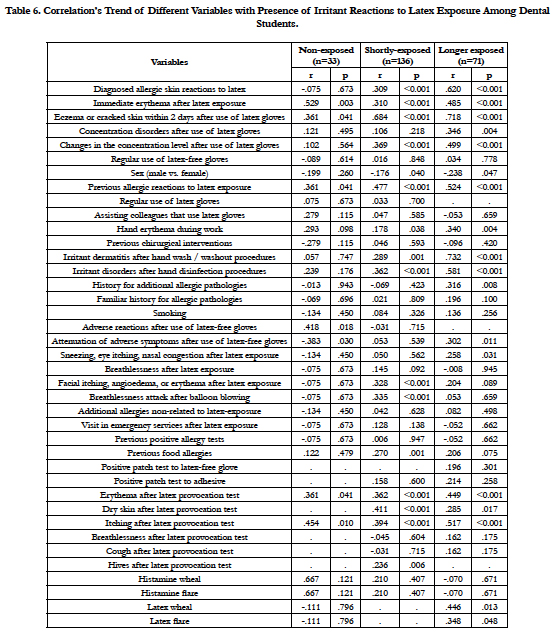
The correlation between occurrence of irritant reactions to latex and studied variables revealed a progressive trend for association with diagnosed skin allergy (including eczema, facial allergy symptoms, positive skin prick test and of course occurrence of irritant dermatitis symptoms during challenge test), allergic eye or nasal symptoms, occurrence of concentration disorders/oscillations, occurrence of allergic or irritating symptoms to latex, hand wash or washout substances, and female sex. For more information see Table 6.
Table 6. Correlation’s Trend of Different Variables with Presence of Irritant Reactions to Latex Exposure Among Dental Students.
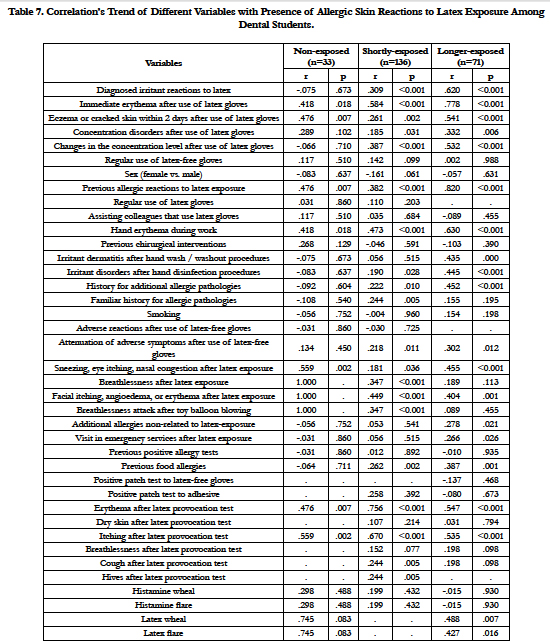
The correlation between occurrence of allergy skin reactions to latex and studied variables revealed a progressive trend with respect to additional irritant dermatitis (including respective symptoms during/after disinfectant or wash/washout procedures), immediate or long-term erythema after gloves wearing, development of eczema or other allergy skin symptoms after latex exposure, concentration’s disorders, visit of emergency services after latex exposure, history for additional allergic pathologies including food allergies, attenuation of symptoms during regular use of latex-free gloves, reports for latex-independent allergic reactions. Diagnostic tests were helpful, but correlation level did not show any progressive trend (for more information, see Table 7).
Table 7. Correlation’s Trend of Different Variables with Presence of Allergic Skin Reactions to Latex Exposure Among Dental Students.
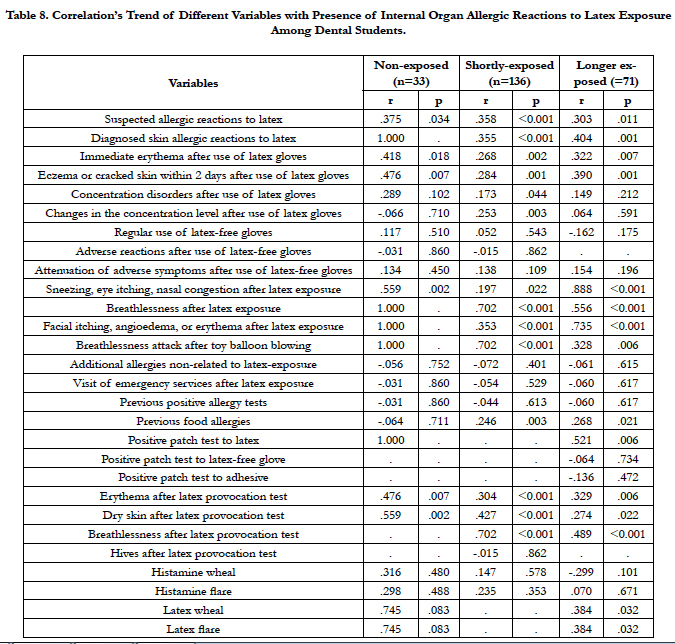
The correlation between occurrence of allergy reactions to latex on inner organs and studied variables revealed a progressive trend with respect to diverse reported symptoms on eye, nose and lower respiratory airways (confirmed by challenge test), facial allergy symptoms, and food allergies (for more information, see Table 8).
Table 8. Correlation’s Trend of Different Variables with Presence of Internal Organ Allergic Reactions to Latex Exposure Among Dental Students.
Discussion
Latex allergy is a major occupational health problem in health care workers, affecting according various studies 0.5 to 18% of subgroups at risk [1, 2, 11-15]. Above-mentioned epidemiologic findings agree with some items in our self-administrated questionnaire, which reports for natural rubber latex allergy among dental students on 10% of cases, hand erythema especially after latex glove wearing in more than 12%, or hand eczema in 14%. A similar frequency is reported among our subjects about concentration disorders or oscillations during the work, which is not mentioned in the literature.
The trend of various questionnaire items shows a progression in concordance with latex exposure along school practice, over-whelming the prevalence value of 20% significantly. This includes self-reporting of latex allergy, occurrence of allergic and irritant contact dermatitis, whereas respiratory symptoms were reported in a smaller subjects’ proportion. A similar prevalence progression for allergic and irritant skin symptoms is observed in an additional study among dental students, showing a significant difference between students of first to third year and them of fourth to sixth year [2]. This trend is demonstrated also in a survey among dental workers in military dental centers [16]. The increased prevalence over 20% in our subpopulation could be related to the gloves quality, which consists both on more efficacious protection level against biological materials (compared to gloves of different material) and on high concentration level for the natural rubber latex (as compared to nitrile gloves [8, 12, 16, 17]. In addition, a sub-proportion of suspected cases for latex allergy in the dental practice could be related to other allergens [2]. Such allergens on dental practice are in nowadays determined and include: quaternary ammonium compounds (commonly used in cleaning/ disinfection products), rubber additives (including carbamates, thiurams, 2-mercaptobenzothiazole, tetramethylthiuram monosulfide, and 1,3-diphenylguanidine), etc [2, 8, 18-20]. Moreover, it is demonstrated a significant association between patch test positivity to latex and rubber additives as well as between allergic and irritant dermatitis in hyper-sensitized subjects to latex gloves [13, 20]. In our study, the potential role of mentioned factors above is reflected on the lower proportion of positive response to diagnostic tests for the latex hypersensitivity, and on the consistent proportion of self-reported to detergents, disinfectants and cases of allergic reactions in workplace that are independent to latex exposure. Thus, the positive response for skin prick test is shown in 20%, for patch test in 15% and for challenge test in 7.5% of cases. The prevalence’s variation between diverse allergic pathologies has been noted in a recent survey, which reported for glove-related cutaneous and non-cutaneous symptoms in 11.3% and 5.9% of the respondents [4]. This finding also suggests that respiratory exposure plays an important role, in addition to dermal exposure [5, 21].
More than one-third of subjects reported for symptoms improvement after systematical avoiding of latex gloves, showing an effective prevention measure against latex allergy especially among subjects with longer study period experience or work practice [21, 22]. This indicates that simple measures such as the use of nonpowdered latex gloves and use of latex-free gloves by sensitized subjects can stop the progression of latex symptoms and can avoid new cases of sensitization [23]. Being often an IgE-mediated disease, the latex allergy among our subjects is associated with other IgE-mediated pathologies like food allergy, and positive skin prick tests to various atopenes in a large proportion. Similarly to this study, previous surveys have noted that family history of allergy, history of personal food allergy, or symptoms associated with toy balloons are frequent among individuals with latex allergy [2-4, 7, 8, 11]. Apart from the frequency trend, the majority of mentioned questionnaire and allergy tests items demonstrated also a progressive correlation trend from the latex non-exposed group to the longer exposed one. This can suggest that questionnaire statements in concert with diagnostic tests are more convincing and conclusive when the pathologic processes and disease’s installation reach an advanced stage due to latex exposure along years of dental practice [24]. This is reinforced by the finding that quantity of gloves use should be considered a risk factor for latex allergy, and the recent confirmation that some commercial tests are useful diagnostic tools only for patients with a history of latex allergy and not for screening the population with a low prevalence of latex sensitization [4, 24].
This study reinforces the conclusion that it is essential to recognize which professionals are sensitized to latex in order to provide appropriate treatment and to establish adequate prevention [3]. A positive history for allergic and irritant symptoms, as determined by questionnaire was significant predictor of a positive response to latex antigens. Healthcare enterprise-wide interventions requiring use of low-allergen gloves, changing gloves to non-latex ones, or even using low-allergen latex gloves, in the affected individuals appears to confer adequate secondary prevention [5, 25]. Because of relationship between allergic reactions to latex gloves and some medical histories, it seems to be necessary the pre-matriculation and pre-employment evaluation, as well as periodic health surveillance of dental students/workers [16].
References
- Risenga SM, Shivambu GP, Rakgole MP, Makwela ML, Nthuli S, et al., (2013) Latex allergy and its clinical features among healthcare workers at Mankweng Hospital, Limpopo Province, South Africa. S Afr Med J. 103(6): 390-4.
- Vangveeravong M, Sirikul J, Daengsuwan T (2011) Latex allergy in dental students: a cross-sectional study. J Med Assoc Thai. 94(3): S1-8.
- Buss ZS, Fröde TS (2007) Latex allergen sensitization and risk factors due to glove use by health care workers at public health units in Florianopolis, Brazil. J Investig Allergol Clin Immunol. 17(1): 27-33.
- Boonchai W, Sirikudta W, Iamtharachai P, Kasemsarn P (2014) Latex gloverelated symptoms among health care workers: a self-report questionnairebased survey. Dermatitis. 25(3): 135-9.
- Supapvanich C, Povey AC, De Vocht F (2014) Latex sensitization and risk factors in female nurses in Thai governmental hospitals. Int J Occup Med Environ Health. 27(1): 93-103.
- Lamberti M, Buonanno R, Ritonnaro C, Giovane G, Crispino V, et al., (2015) Molecular profile of sensitization in subjects with short occupational exposure to latex. Int J Occup Med Environ Health. 28(5): 841-8.
- Köse S, Mandiracioğlu A, Tatar B, Gül S, Erdem M (2014) Prevalence of latex allergy among healthcare workers in Izmir (Turkey). Cent Eur J Public Health. 22(4): 262-5.
- Liu QL, He XZ, Liang K, Xie R, Fang HP, et al., (2013) Prevalence and risk factors for latex glove allergy among female clinical nurses: a multicenter questionnaire study in China. Int J Occup Environ Health. 19(1): 29-34.
- Nabavizadeh SH, Anushiravani A, Amin R (2009) Natural rubber latex hypersensitivity with skin prick test in operating room personnel. Iran J Allergy Asthma Immunol. 8(4): 219-20.
- Agrawal A, Bhatt N, Kk S, Singh K, Chaudhary H, et al., (2010) Prevalence of allergy to latex gloves among dental professionals in Udaipur, Rajasthan, India. Oral Health Prev Dent. 8(4): 345-50.
- Galindo MJ, Quirce S, Garcia OL (2011) Latex allergy in primary care providers. J Investig Allergol Clin Immunol. 21(6): 459-65.
- Copertaro A, Bracci M, Barbaresi M, Bianchini G (2006) Usefulness of a questionnaire and RAST in screening of health care workers allergic to latex. Med Lav 97(6): 779-86.
- Ly F, Mbaye I, Wone I, Gaye-Fall C, Sow ML, et al., (2006) Allergy to latex gloves among healthcare workers in Dakar. Ann Dermatol Venereol. 133(12): 971-4.
- Wan KS, Lue HC (2007) Latex allergy in health care workers in Taiwan: prevalence, clinical features. Int Arch Occup Environ Health. 80(5): 455-7.
- Zeiss CR, Gomaa A, Murphy FM, Weissman DN, Hodgson M, et al., (2003) Latex hypersensitivity in Department of Veterans Affairs health care workers: glove use, symptoms, and sensitization. Ann Allergy Asthma Immunol. 91(6): 539-45.
- Ghasemi IM, Rezaee M, Jonaidi Jafari N, Izadi M (2007) Latex gloves allergy in dental workers, Iran. Pak J Biol Sci.10(7): 1068-72.
- Crippa M, Gelmi M, Sala E, Zefferino R, Baccolo TP, et al., (2004) Latex allergy in health care workers: frequency, exposure quantification, efficacy of criteria used for job fitness assessment. Med Lav. 95(1): 62-71.
- Gonzalez M, Jégu J, Kopferschmitt MC, Donnay C, Hedelin G, et al., (2014) Asthma among workers in healthcare settings: role of disinfection with quaternary ammonium compounds. Clin Exp Allergy. 44(3): 393-406.
- Cao LY, Taylor JS, Sood A, Murray D, Siegel PD (2010) Allergic contact dermatitis to synthetic rubber gloves: changing trends in patch test reactions to accelerators. Arch Dermatol. 146(9): 1001-7.
- Miri S, Pourpak Z, Zarinara A, Heidarzade M, Kazemnejad A, et al., (2007) Prevalence of type I allergy to natural rubber latex and type IV allergy to latex and rubber additives in operating room staff with glove-related symptoms. Allergy Asthma Proc. 28(5): 557-63.
- Kelly KJ, Wang ML, Klancnik M, Petsonk EL (2011) Prevention of IgE sensitization to latex in health care workers after reduction of antigen exposures. J Occup Environ Med. 53(8): 934-40.
- Al-Ali K, Hashim R (2012) Occupational health problems of dentists in the United Arab Emirates. Int Dent J. 62(1): 52-6.
- Filon FL, Radman G (2006) Latex allergy: a follow up study of 1040 healthcare workers. Occup Environ Med. 63(2): 121-5.
- Accetta Pedersen DJ, Klancnik M, Elms N, Wang ML, Hoffmann RG, et al., (2012) Analysis of available diagnostic tests for latex sensitization in an at-risk population. Ann Allergy Asthma Immunol. 108(2): 94-7.
- Reunala T, Alenius H, Turjanmaa K, Palosuo T (2004) Latex allergy and skin. Curr Opin Allergy Clin Immunol. 4(5): 397-401.