Oral Mucositis - A Hindrance in Management of Oral Malignancy
Sangavi.R1*, Uma Maheshwari2
1 Senior Lecturer, Department of oral medicine, Radiology and Special Care Dentistry, Saveetha Institute of Medical and Technical Science, Chennai, India.
2 Professor, Department of Oral Medicine, Radiology and special care Dentistry, Saveetha Institute of Medical and Technical Science, Chennai, India.
*Corresponding Author
Sangavi. R,
Senior Lecturer, Department of oral medicine, Radiology and Special Care Dentistry, Saveetha Institute of Medical and Technical Science, Chennai, India.
Tel: 9940588033
E-mail: sangaviramesh12@gmail.com
Received: September 05, 2022; Accepted: April 20, 2023; Published: June 13, 2023
Citation: Sangavi.R, Uma Maheshwari. Oral Mucositis - A Hindrance in Management of Oral Malignancy. Int J Cancer Stud Res. 2023;10(1):156-158.
Copyright: Sangavi. R©2023. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Oral Mucositis (OM) is one of the major and the commonest toxicities of cancer therapy. It occurs in almost all patients who undergoes radiation therapy or chemotheraphy in which the mucosal areas of oral and oropharyngeal region are included in the treatment zone. The pathophysiology of oral mucositis has always been a puzzle to the physicians and there are still many unanswered questions left about the risk factors for developing OM, Clinicians and researchers should join hands in pursuit of understanding and expanding the treatment strategies for Management of inflammatory conditions like OM in oncology. This will lead path to development of effective treatments and thereby reducing the burden of Oral mucositis and other inflammatory conditions in oncology. This article summarizes and gives clear insightson the risk factor, patient factors that is responsible for developing OM, elaborates the pathogenesis, clinical presentation, grading and management of the condition in detail.
2.Introduction
3.Epidemiology
4.Pathophysiology
5.Clinical Presentation
6.Evaluation
7.Management
8.Pain Management
9.Chemoprotective Agent
10.Low-Level Laser Therapy
11.Cryotherapy
12.Antioxidants
13.Anti-inflammatory Agents
14.Zinc Supplementation
15.Diet
16.Conclusion
17.References
Keywords
Oral Mucositis, Radiotherapy, Chemotherapy, HSCT.
Introduction
Oral mucositis is a severely debilitating condition that occurs during
the Treatment of malignancy with radiation therapy (RT),
chemotherapeutic agents, and hematopoietic stem cell transplantation
(HSCT)[1]. It represents an area of erythema followed by
rupture of the oral mucosa with subsequent pain and reduction in
oral intake. The lesions can also shatter the skin barrier resulting
in local or systemic infection.[2] In severe cases, this can lead to
nutritional deficiency and ultimately lead to poor quality of life.
[3] This article gives an insight into the diagnosis and management
of oral mucositis and the role of the interdisciplinary team
in managing complications of oral mucositis to improve patient
wellbeing.[4]
Epidemiology
The incidence of Oral Mucositis depends upon the intensity of
the drug and radiation and duration of the treatment.[8] A study
reported that patients who receive high doses of chemotherapy
or undergo bone marrow transplantation have a 76 % risk of getting
mucositis. Radiation-induced oral mucositis (RIOM) occurs
in 100% of altered fractionation radiotherapy head and neck cancer
patients.[7] Patients with poor nutritional status and poor oral
care are more susceptible to developing Oral mucositis. [6]
Pathophysiology [8]
The pathophysiology behind the development of oral mucositis
due to chemotherapy and radiotherapy is thought to be due to a
complex process that starts with injury to the tissue. This mechanism
is described in a five-phase model suggested by Sonis.
Phase 1: Initiation of tissue injury: Radiation and/or chemotherapy
induce direct cellular damage resulting in lysis of the basal
epithelial cells. The generation of reactive oxygen species (free
radicals) by radiation or chemotherapy is also believed to exert a
role in the initiation of mucosal injury. These small highly reactive
molecules are by-products of oxygen metabolism and can cause
significant cellular damage.
Phase 2: Messaging and Signalling: Besides causing direct cell
death and production of free radicals it also upregulates inflammation
via the production of messenger signals. The free radicals
produced in the previous phase activate the second messengers
that transmit signals from the cell surface receptors to the internal
environment of the cell. This leads to the upregulation of proinflammatory
cytokines which in turn leads to tissue injury and
cell death.
Phase 3: Signaling and amplification: increased production
of proinflammatory cytokines like tumor necrosis factor-alpha
(TNF-α), not only leads to mucosal cell injuries besides activates
molecular pathways that in turn amplify mucosal injury.
Phase 4: Ulceration and inflammation: Due to the upregulation
of proinflammatory cytokines the mucosa is infiltered with
an enormous number of inflammatory cells associated with the
mucosal ulcerations, furthermore the metabolic by-products (proinflammatory
cytokines) of the colonizing oral microflora also
further upregulates the process and leads to secondary infection.
Phase 5: Healing: Healing is characterized by epithelial proliferation
and cellular differentiation which contributes to restoring
the integrity of the epithelium.
Clinical Presentation
Mucositis is usually limited to non-keratinized surfaces of the
Oral cavity e.g. buccal and labial mucosa, lateral tongue, ventral
tongue, and soft palate.[4] Patients complain of discomfort/pain
with eating or may have increased bleeding while brushing. Oral
mucositis due to RT begins after the initiation of treatment to the
head and neck it starts as acute inflammation in the oral mucous
membrane like buccal mucosa, tongue, and pharynx and lasts
between 7 and 98 days.[10] furthermore, oral mucositis due to
chemotherapy has a periodic association with the dose of cytotoxic
drug usually develops within 1 - 2 weeks of the given quantity
[11]. It initially develops as erythema which later progresses
into erosion and ultimately ulcerates later the ulcerated region is
covered with a pseudomembranous layer which eventually peels
off. [12] In patients undergoing HSCT, the oral mucositis resolves
as the absolute neutrophil count recover.
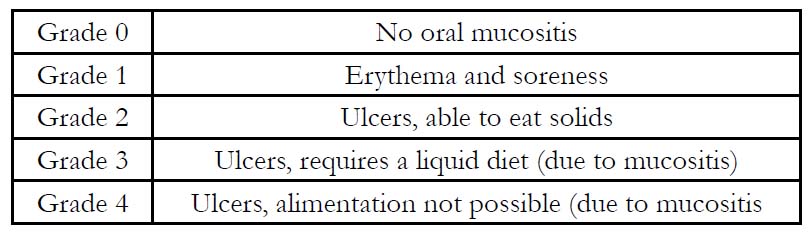
Evaluation
History and Clinical examination play a key role in the evaluation
of Oral Mucositis. The intensity of oral mucositis is evaluated on
a well-defined scale. Various scales like.
Common Terminology Criteria for Adverse Events (CTCAE),
Oral Mucositis Assessment Scale (OMAS), Eastern Cooperative
Oncology Group, and WHO scale. Out of all the available scales,
the Universally accepted is the WHO scale which combines both
subjective and objective measures of oral mucositis.[13,14].
Management
Oral Hygiene Protocol
Maintenance of good oral hygiene protocols has been shown to
help prevent mucositis and shorten the duration and intensity.
Furthermore, It also helps to cut down the microbial load in the
oral cavity which prevents the development of secondary infections.[
16] Regular Oral care includes removal of dentures, gentle
cleansing which includes flossing and brushing using ultra-soft
bristles, and oral rinses. Several Oral rinses are available which
include saline water rinse, sodium bicarbonate rinse, a mix of sodium
bicarbonate and saline water, hydrogen peroxide (diluted 1:1
with saline or water), and miracle mouthwash.[1]“Magic mouthwash”
which consists of diphenhydramine, viscous lidocaine, bismuth
subsalicylate, and corticosteroid has proven to be the best
mouth wash for treating oral mucositis [17].
Pain Management
Topical anesthetic agents such as lidocaine are efficacious in reducing
the intensity of the lesions and also relives pain; however,
this effect varies depending on the agent used. Topical agents
would be a great at-home treatment option to allow for relief of
pain and reduction in inflammation Also, opioid analgesics are
given to alleviate pain.[16]
Chemoprotective Agent
Palifermin is a keratinocyte growth factor and works as a chemoprotective
agent, which has been recommended for severe oral
mucositis (mucositis greater than or equal to grade 3) associated
with autologous hematopoietic stem cell transplant regimens. In
such patients, it has been shown to decrease the incidence and
duration of severe oral mucositis. [16]
Low-Level Laser Therapy
low-level laser therapy is being currently explored to amplify
wound healing with a reduction in pain and inflammation; Nevertheless,
standard treatment protocols are not currently present
for all chemotherapy agents. A double-blinded study showed
that low-level laser therapy was beneficial in the prevention of
oral mucositis in patients receiving high-dose chemotherapy for
HSCT.[17] It has been postulated that low-level laser therapy
combats against the production of reactive oxygen species and/
or pro-inflammatory cytokines that imparts a role in the pathogenesis
of mucositis.
Cryotherapy
For some chemotherapy agents, data suggests the use of placing
ice chips in the mouth is beneficial, for example, during bolus of
5-fluorouracil and high dose melphalan.[18]
Antioxidants
Amifostine which is a radioprotective agent is believed to act as a
scavenger of reactive oxygen species which are potential agents to
initiate mucositis . However, due to insufficient data, a MASCC/
ISOO guideline could not be established regarding the usage of
this agent in oral mucositis in patients receiving chemotherapy
or radiotherapy. The topical application of amifostine in the oral
cavity consists of the antioxidant, N-acetylcysteine. In a placebocontrolled
trial in patients receiving radio and chemotherapy with
head and neck cancer, amifostine remarkably reduced the incidence
of severe oral mucositis up to doses of 50 Gy radiation.[19]
Anti-inflammatory Agents
Benzydamine hydrochloride is a non-steroidal anti-inflammatory
drug that suppresses the pro-inflammatory cytokines including
TNF-α. In a Phase III trial, benzydamine hydrochloride mouth
rinse reduced the intensity of mucositis in patients with head and
neck cancer undergoing radiation therapy up to a total dose of
50 Gy radiation therapy. [20] Based on this report and other literature,
the MASCC/ISOO guidelines recommended the use of
Benzydamine hydrochloride in patients receiving moderate-dose
of radiation therapy. Nevertheless, this agent has not received approval
for this use from the U.S. FDA; besides, most patients with
head and neck cancer receive over 50 Gy radiation therapy along
with concomitant chemotherapy. A more recent Phase III trial of
Benzydamine hydrochloride in radiation-induced oral mucositis
in patients with head and neck cancer was discontinued based on
negative results of an interim analysis.
Zinc Supplementation
Zinc helps in the re-epithelisation of the tissues as well as scavenges
the free radicals and protects the mucosa from further damage
It is beneficial as adjuvant therapy in patients with oral cancer
undergoing chemoradiation.[16]
Diet
Diet during the period of mucositis plays a pivotal role in managing
the flare-up of the condition. The diet is restricted to soft
and land food that doesn’t traumatize the oral mucosa Foods that
contains less salt, and acid are advisable, sipping water frequently
helps to combat the friction of the oral mucosa due to lack of
saliva which in turn prevents further damage.[11]
Conclusion
Radiotherapy and Chemotherapy can be associated with multiple
side effects among which oral mucositis is the condition which
produces major discomfort to the patient it also hinders patient’s
quality of life. As it becomes well understood, most of these side
effects cannot be avoided. Several preventive measures are taken in order to limit their expression. The oral cavity is a usual site of
discomfort and pain caused by Mucositis. The role of dentist is
pivotal inmanaging oral mucositis to provide relief to the suffering
patients.
References
- Beech N, Robinson S, Porceddu S, Batstone M. Dental management of patients irradiated for head and neck cancer. Aust Dent J. 2014 Mar;59(1):20-8. PubMed PMID: 24495127.
- Miranda-Silva W, Gomes-Silva W, Zadik Y, Yarom N, Al-Azri AR, Hong CHL, etal. MASCC/ISOO clinical practice guidelines for the management of mucositis: sub-analysis of current interventions for the management of oral mucositis in pediatric cancer patients. Support Care Cancer. 2021 Jul;29(7):3539-3562. PubMed PMID: 33156403.
- Rubenstein EB, Peterson DE, Schubert M, Keefe D, McGuire D, Mucositis Study Section of the Multinational Association for Supportive Care in Cancer; International Society for Oral Oncology. Clinical practice guidelines for the prevention and treatment of cancer therapy-induced oral and gastrointestinal mucositis. Cancer. 2004 May 1;100(9 Suppl):2026-46. PubMed PMID: 15108223.
- Lalla RV, Sonis ST, Peterson DE. Management of oral mucositis in patients who have cancer. Dent Clin North Am. 2008 Jan;52(1):61-77. PubMed PMID: 18154865.
- Brown TJ, Gupta A. Management of Cancer Therapy-Associated Oral Mucositis. JCO OncolPract. 2020 Mar;16(3):103-109. PubMed PMID: 32048926.
- Vagliano L, Feraut C, Gobetto G, Trunfio A, Errico A, Campani V, et al. Incidence and severity of oral mucositis in patients undergoing haematopoietic SCT--results of a multicentre study. Bone Marrow Transplant. 2011 May;46(5):727-32. PubMed PMID: 20818449.
- Maria OM, Eliopoulos N, Muanza T. Radiation-Induced Oral Mucositis. Front Oncol. 2017 May 22;7:89. PubMed PMID: 28589080.
- Sonis ST. Pathobiology of oral mucositis: novel insights and opportunities. J Support Oncol. 2007 Oct;5(9 Suppl 4):3-11. PubMed PMID: 18046993.
- Lallarv
- Maria OM, Eliopoulos N, Muanza T. Radiation-Induced Oral Mucositis. Front Oncol. 2017 May 22;7:89. PubMed PMID: 28589080.
- Brown TJ, Gupta A. Management of Cancer Therapy-Associated Oral Mucositis. JCO OncolPract. 2020 Mar;16(3):103-109. PubMed PMID: 32048926.
- Lalla RV, Peterson DE. Oral mucositis. Dent Clin North Am. 2005 Jan;49(1):167-84. PubMed PMID: 15567367.
- Lalla RV, Sonis ST, Peterson DE. Management of oral mucositis in patients who have cancer. Dent Clin North Am. 2008 Jan;52(1):61-77. PubMed PMID: 18154865.
- Sonis ST, Eilers JP, Epstein JB, LeVeque FG, Liggett WH Jr, Mulagha MT, et al. Validation of a new scoring system for the assessment of clinical trial research of oral mucositis induced by radiation or chemotherapy. Mucositis Study Group. Cancer. 1999 May 15;85(10):2103-13. PubMed PMID: 10326686.
- Elad S, Cheng KKF, Lalla RV, Yarom N, Hong C, Logan RM, et al. MASCC/ ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy. Cancer. 2020 Oct 1;126(19):4423-4431. PubMed PMID: 32786044.
- Pulito C, Cristaudo A, Porta C, Zapperi S, Blandino G, Morrone A, et al. Oral mucositis: the hidden side of cancer therapy. J ExpClin Cancer Res. 2020 Oct 7;39(1):210. PubMed PMID: 33028357.
- Peterson DE, Ohrn K, Bowen J, Fliedner M, Lees J, Loprinzi C, et al. Systematic review of oral cryotherapy for management of oral mucositis caused by cancer therapy. Support Care Cancer. 2013 Jan;21(1):327-32. PubMed PMID: 22993025.
- Mantovani G, Macciò A, Madeddu C, Mura L, Massa E, Gramignano G, et al. Reactive oxygen species, antioxidant mechanisms and serum cytokine levels in cancer patients: impact of an antioxidant treatment. J Cell Mol Med. 2002 Oct-Dec;6(4):570-82. PubMed PMID: 12611641.
- Epstein JB, Silverman S Jr, Paggiarino DA, Crockett S, Schubert MM, Senzer NN, et al. BenzydamineHCl for prophylaxis of radiation-induced oral mucositis: results from a multicenter, randomized, double-blind, placebocontrolled clinical trial. Cancer. 2001 Aug 15;92(4):875-85. PubMed PMID: 11550161.
- Lalla RV, Schubert MM, Bensadoun RJ, Keefe D. Anti-inflammatory agents in the management of alimentary mucositis. Support Care Cancer. 2006 Jun;14(6):558-65. PubMed PMID: 16565821.