Upper Lid Blepharoplasty Without Cutting the orbicularis Muscle
Van Meer N1, Backaert T2, Verhaert P3, Raus P4*
1 Universitair Ziekenhuis VUB, Jette, Belgium.
2 A.Z. St. Rembert, Torhout, Belgium.
3 Pathology Unity, General Hospital Herentals (AZ Herentals), Herentals, and ProteoFormiX, Beerse, Belgium.
4 Miró Centrum Voor oogheelkunde en Esthetiek, Geel, Belgium.
*Corresponding Author
Dr. Peter Raus,
Miró Centrum voor oogheelkunde en Esthetiek, Geel, Belgium.
E-mail: peter.raus@gmail.com
Received: March 25, 2017; Accepted: April 17, 2017; Published: April 22, 2017
Citation: Van Meer N, Backaert T, Verhaert P, Raus P (2017) Upper Lid Blepharoplasty Without Cutting the orbicularis Muscle. Int J Ophthalmol Eye Res. 5(4), 308-312. doi: dx.doi.org/10.19070/2332-290X-1700063
Copyright: Raus P© 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
We have compared the aesthetic outcomes of upper blepharoplasty with or without resection of the preseptal orbicularis oculi muscle. In addition we evaluated MRI to visualize the differences in the upper eyelids before and after surgery.
An interventional randomized double-blind left right study was conducted in 10 patients with upper eyelid dermatochalazis. One side was randomly chosen for incision of the preseptal orbicularis oculi muscle and direct coagulation or resection of fat pockets.
The orbicularis oculi muscle of the contralateral side was not incised. Only a soft coagulation was performed on the muscle to induce a septal contraction and push the orbital fat back. All interventions were performed with an Ellman Dual frequency high frequency low temperature unit. Digital photos were taken before and after surgery and patients were asked to fill in a questionnaire to evaluate the surgery itself as well as the aesthetic outcome.
In an attempt to objectify these findings, NMR imaging of the orbits was performed before and 6 weeks after surgery. Symptoms scoring was similar in both groups. At 6 weeks post-operation, no significant differences were observed between left and right eye.
In conclusion, patients with dermatochalazis but without prominent fat prolapse in the upper eyelid, did not exhibit significant differences after cutting or not the orbicularis muscle to excise orbital fat. Even in cases with moderate fat prolapse, the fat can be pushed back by soft coagulation of the orbicularis and underlying orbital septum. When the preseptal orbicularis oculi muscle is preserved, the risk of hematoma and orbital cellulitis can be limited.
2.Pathogenesis of Dermatochalazis
3.Blepharoplasty Step by Step
3.1 Marking the Skin to be Excised
3.2 Skin Resection
4.Results
5.Discussion
6.Conclusion
7.References
Introduction
According to the American Society for Aesthetic Plastic Surgery, 161, 389 cosmetic eyelid surgery procedures were performed in the United States in 2013 (www. Surgery.org). This makes blepharoplasty the third most popular elective cosmetic procedure, behind liposuction (363, 912) and breast augmentation (313, 327), but ahead of abdominoplasty (160, 077) and rhinoplasty (147, 996).
For the age group of 51 years and older, blepharoplasty even was one of the top three procedures, the other two being liposuction and facelift.
Blepharoplasty can be performed by many operative approaches and an almost uncountable number of different techniques have been published [1, 9, 13, 14, 18].
Pathogenesis of Dermatochalasis
With age the mesodermal content of the body shrinks. This results in the skin becoming too large, and the appearance of wrinkles and redundant skin folds [3, 4, 18].
In the upper eyelids atrophy of mesodermal structures implies loss of adnexal structural support by the tarsus, the canthal tendons, and orbicularis muscle. This, in combination with a thinning eyelid skin [7], leads to orbital fat prolapse and eyelid malposition [5, 10, 11]. The desinsertion or attenuation of the levator muscle aponeurosis may cause involutional (aponeurotic) ptosis [19].
Involutional changes in the orbital septa cause downward migration of the brow fat, leading to a brow ptosis. It is not uncommon that a brow ptosis is misdiagnosed as upper eyelid dermatochalazis. The potential complication that arises if a blepharoplasty is performed on a patient with significant brow ptosis is that the brow is pulled further downward to the lashes and a shortage of the anterior lamella remains. This can lead to a lagophthalmos or lid lag and even the need for a future skin graft [6]. In the eyelid itself anterior migration of the preaponeurotic fat pads results in pseudoptosis.
Age dependent histological changes in the orbicularis oculi muscleare minimal [2, 8]. That is why in patients without prominent fat pockets, an upper lid blepharoplasty, limited to a simple cutaneous resection often yields satisfactory aesthetic results. In those patients the orbicularis muscle does not need to be incised, but can be fully preserved to maintain eyelid ‘fullness’ and prevent a hollow aspect of the upper lid, particularly in younger patients. Indeed, fullness of the upper eyelid is a sign of youth. The most important question with aesthetically disturbing eyelid fat pockets is whether this is due to a herniation of a normal fat pocket or by an age-related expansion of orbital fat [22]. Upper eyelid fat pockets can mostly be pushed back by a soft coagulation of the orbicularis and underlying orbital septum [13].
Two upper eyelid fat pockets can classically be distinguished: a nasal one and one in the middle of the eyelid. In the lateral part of the upper lateral quadrant of the orbit, just below the orbital rim lies the palpebral part of the lacrimal gland. Care has to be taken not to damage this gland; as this could lead to an irreversible and very difficult to treat dry eye. That is why, even when fat resection in the upper eyelid appears to be mandatory, we advice to always limit the incision of the orbicularis muscle and the orbital septum to the nasal two thirds. In 2004 Persichetti et al., described a third fat compartment in the upper eyelid in 21.3% of the examined upper eyelids (47 patients who underwent upper blepharoplasty and 11 fresh cadavers; [15, 20]). In spite of this high incidence, but given the high similarity de visu of palpebral fat and glandular structures and the risk of causing a terrible dry eye, we prefer not to explore the lateral third of the suborbicular space to look for this extra fat pocket [21].
Preoperative markings should be made with a skin marker before injecting the local anaesthetic and with the patient sitting upright in neutral gaze with the brow properly positioned.
The lower limit of excision should be along the eyelid crease. In cases of a double crease the surgeon should mark the lower one to avoid a double lid crease postoperatively.
The lateral extent of the marking should be limited by an imaginary line from the lateral end of the brow to the lateral canthus. The extent of excision should be at least 10 mm from the inferior border of the natural brow, making a pattern of skin excision with an acute angle laterally and an obtuse angle nasally. We want to emphasize that many women epilate their brows and that the visible inferior border of the brow might be quite a bit higher than the natural border, so surgeons should take care of that.
A skin pinch test can confirm the preoperative markings. Alternatively the patient can be asked to look up. In this position the lower and upper demarcation lines should ‘almost’ join.
For all our surgery we used the Ellman Dual Freqency high frequency low temperature device.
For the skin resection a fine wire electrode is used.
In a first step the border of the skin fragment to be excised is in cised very superficially while care is taken not to hit the orbicularis muscle. Then, with an assistant nurse pulling the eyelid upwards, a superificial excision of only skin is performed. Bleeding vessels can be coagulated by indirect coagulation via a surgical forceps grasping the vessel, touching the forceps with the electrode and activating the unit. Alternatively the RF electrode can also be used for contact coagulation (i.e. in direct contact with the tissue).
Indirect coagulation has our personal preference. When a bleeding vessel is encountered the surgeon can immediatley grasp the ‘bleeder’ and use the indirect coagulation without the need to change electrode, waveform, or power. Indeed, even in the cutting mode of the RF unit, the current has 10% of cutting power that is accumulated when not moving the electrode through the tissue.
The surgeon will then switch to a ball electrode and with the unit in coagulation mode, a soft coagulation of the orbicularis oculi muscle is achieved inducing limited fibrosis of the muscle and a septal contraction. Attempts should be made to avoid to coagulate tissues close to the wound edges because this might delay the healing time due to clogged feeding capillaries.
In the majority of cases no fat resection is needed. The soft coagulation of the oribicularis muscle and underlying orbital septum will be enough to push back the orbital fat pockets. The local fibrosis, induced by the coagulation will consolidate the position of the fat pockets after the surgery. In these cases the skin can already be sutured with a 6/0 monofilament suture material. I personally prefer to separate sutures starting with one in the middle and then suturing the skin in the temporal to nasal direction.
Even when some fat resection appears to be mandatory to achieve an acceptable result, a soft coagulation of the orbicularis musclewith a ball electrode is still preferred before making an incision in the orbicularis at about 14 mm above the lid margin. This high incision gives direct acces to the fat pockets with out the risk of damaging the underlying levator muscle or aponeurosis. For the incision in the orbicularis we use a thicker electrode to limit the bleeding. This incision is limited to the nasal two thirds of the eyelid to avoid damage to the lacrimal gland. The fat is carefully disected and directly resected without using a clamp but with the unit in a cut-coagulation mode.
The orbicularis is sutured with a few Vicryl 6/0 sutures.
To compare the outcome of upper lid blepharoplasty with or without incision of the orbicularis + fat resection we performed a bilateral upper blepharoplasty in 10 patients with a fat resection on one side and without fat resection on the other eye.
The side with or without fat resection was randomly chosen and the patient was not aware of this choice.
After standardized excess skin marking, one side was randomly chosen to remove skin and a slice of orbicularis muscle with a RF electrode and excision of prolapsed medial and central orbital fat pads. The skin of the contralateral upper eyelid was also excised with radio frequency using the needle electrode and the underlying orbicularis muscle and orbital septum was shrunk with radio frequency using a ball electrode and switching the unit from a pure cut to a coagulation setting.
The orbicularis, when incised, was closed with 3 to 4 Vicryl 6/0 sutures. The skin was sutured with separate Prolene 6/0 sutures that were removed after 6 days.
All patients had an ophthalmic examination before, 1 and 6 weeks after surgery. All patients had standardized digital photographs before and 6 weeks after surgery.
All patients had standardized orbital magnetic resonance imaging before and 6 weeks after surgery.
All patients were asked to compete a patient satisfaction questionnaire after 6 weeks.
They were asked to quote on the following parameters.
Pain: a scale from 0 (no pain) to 4 (severe pain).
Swelling: a scale from 0 (no swelling) to 4 (severe swelling).
Eye irritation: a scale from 0 (no irritation) to 4 (severe irritation) Difficulty with closing the eyes in the first week after surgery 0 = no 1 = yes.
Aesthetic outcome: scale from 1 (not good) to 10 (perfect). Preference between left or right eye, without knowing the technique used for which eye.
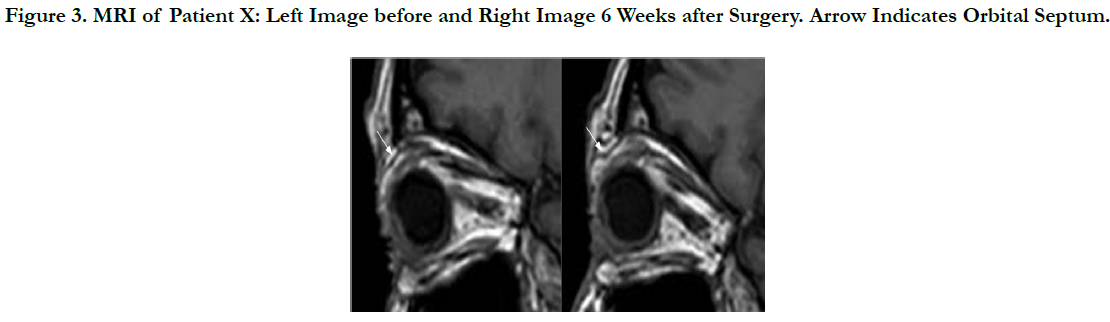
The purpose of MR imaging was to ascertain whether MR imaging could show the effect of the proposed blepharoplasty technique, compared with the original technique (with excision of orbital fat) and whether we could detect a difference in the localization of the septum orbitale [16, 17].
Our patients underwent bilateral orbital high-resolution MR imaging on a 3T system pre- and postoperatively using T1-imaging. We look for differences in fat quantity pre-and postseptal, and evaluate the position of the septum, comparing both eyes and thus both techniques.
Results
Originally 10 patients were included in our study but one patient was lost for follow-up so the respective data are not included.
These included 8 female and 1 male patient participated. The average age was 57.3 (spread between 51-70).
In 3 cases the left eye was operated without orbicularis incision; of the 6 other patients the right eye.
On the pain scale (from 0 [no pain] to 4 [severe pain]), 4 patients recorded “0” and 5 patients “1”.
For the parameter ‘swelling’ (a scale from “0” [no swelling] to “4” [severe swelling]), 2 patients reported “0”, 3 patients scored “1”, and 3 others noted “2”.
Of all patients, 1 reported a swelling of “2” at the side without orbicularis incision and “3” on the eyelid where the orbicularis was opened with fat resection.
For the parameter ‘bruising’ (hematoma) 8 patients reported the same bruising on both sides, whereas 3 patients recorded no bruising at all, 3 patients reports limited bruising (value “1”) and 2 patients value “2”.
Only 1 patient reported a limited bruising on the side where the orbicularis was incised.
For the parameter “irritation”, 7 patients scored “0” (did not experience any irritation at all), 1 reported score “1” and 1 patient scored “2”.
Only 2 patients reported some difficulty in closing the eyes (score “1”) in the first week after surgery.
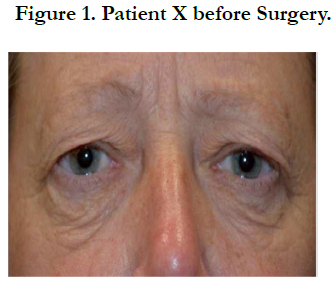
All patients were happy with the aesthetic outcome of the surgery with no preference for left or right eye with a minimum score of 8/10 (4 patients), 9/10 (2 patients) and 10/10 (3 patients) (Figures 1-2).
Unfortunately only in one case the septum was clearly depicted on both pre-and post op scans. In this case a difference in the position between the septum pre- and postoperative could be shown even in the eye where the orbicularis was not incised and only coagulated (Figure 3). In the other cases the septum could not be visualized in one or both examinations due to small motion artefacts, or a slightly different eye orientation, making a good comparison impossible. As the septum is a very thin structure, results are very dependent on the cooperation of the patient and on the patient’s ability to lie perfectly still for 5-10 min. without moving his/her eyes. No significant change was observed in the amount of retroseptal fat but the expected volume change is very limited. So, high-resolution MR imaging showed a different septum position comparing pre- and postoperative scans using our technique in one patient. An exact depiction of the septum orbitale remains very much conditional on the cooperation of the patient.
Figure 3. MRI of Patient X: Left Image before and Right Image 6 Weeks after Surgery. Arrow Indicates Orbital Septum.
Due to motion artifacts and the very subtle changes no volume difference could be seen.
Discussion
Upper lid blepharoplasty is a common surgical intervention and many different techniques can be employed to achieve a good functional and aesthetic outcome. Although only 9 patients (18 eyelids) were included in the present study, our results suggest that in most cases surgery can be limited to an appropriate skin resection and soft coagulation of the orbicularis muscle and underlying orbital septum. Also, omitting the incision of the orbicularis muscle limits the risk of superficial and deep bleeding and orbital cellulitis.
Patients’ acceptance is excellent thanks to the good aesthetic outcome and the fast recovery.
Conclusion
Upper lid blepharoplasty without cutting the orbicularis muscle appears to be an excellent technique for patients with dermatochalasis with no or only moderate orbital fat prolapse. Unfortunately MRI of the orbit is not appropriate to visualize the orbital septum and other imaging techniques should be explored if a visualization of surgical results is needed.
References
- Pfeiffer MJ (2006) Update on upper lid blepharoplasty. Oculoplastics and Orbit. Springer Science & Business media.
- Salvi SM, Akhtar S, Currie Z (2006) Ageing changes in the eye. Postgraduate Medical J. 82(971): 581-587.
- De Backer CM, Putterman AM, Zhou L, Holck DE, Dutton JJ (1998) Agerelated changes in type-I collagen synthesis in human eyelid skin. Ophthal Plast Reconstr Surg. 14(1): 13-16.
- Krutmann J, Béhar-Cohen F, Baillet G, de Ayguavives T, Reme C, et al., (2014) Towards standardization of UV eye protection: what can be learned from photodermatology? Photodermatol Photoimmunol Photomed. 30(2-3): 128-136.
- Jacobs LC, Liu F, Bleyen I, Gunn DA, Hofman A, et al., (2014) Intrinsic and extrinsic risk factors for sagging eyelids. J Am Assoc Dermatol. 150(8): 836-843.
- Keyvan N (2008) Complications in Dermatologic Surgery. Elsevier Health Services. 286.
- Hwang K, Kim DJ, Kim SK (2006) Does the upper eyelid skin become thinner with age? J Craniofac Surg. 17(3): 474-476.
- Manners RM, Weller RO (1994) Histochemical staining of orbicularis oculi muscle in ectropion and entropion. Eye. 8(3): 332-335.
- Damasceno RW, Cariello AJ, Cardoso EB, Viana GA, Osaki MH (2011) Upper blepharoplasty with or without resection of the orbicularis oculi muscle: randomized double-blind left-right study. Ophthal Plast Reconstr Surg. 27(3): 195-197.
- Goldberg RA, McCann JD, Fiaschetti D, Ben Simon GJ (2005) What causes eyelid bags? Analysis of 114 consecutive patients. Plast Reconstr Surg. 15(5): 1395-1402.
- Feher J, Olah Z (2008) Age related changes of the human eye. Age-Related changes of the eyelid. Springer. 9-33.
- Stricker M, Pujo J, Simon E (2009) Controversies regarding the orbital septum, Ann Chir Plast Esthet. 54(6): 551-566.
- Van der Lei B, Timmerman IS, Cromheecke M, Hofer SO (2007) Bipolar coagulation-assisted orbital (BICO) septoblepharoplasty: a retrospective analysis of a new fat-saving upper-eyelid blepharoplasty technique. Ann Plast Surg. 59(3): 263-267.
- Meyer DR, Linberg JV, Wobig JL, McCormick SA (1991) Anatomy of the orbital septum and associated eyelid connective tissues. Implications for ptosis surgery. Ophthal Plast Reconstr Surg. 7(2): 104-113.
- Persichetti P, Di Lella F, Delfino S, Scuderi N (2004) Adipose compartments of the uper eyelid: anatomy applied to blepharoplasty. Plast Reconstr Surg. 113(1): 373-378.
- Al-BakriM, Rasmussen AK, Thomsen C, Toft PB (2014) Orbital Volumetry in Graves' Orbitopathy: Muscle and Fat Involvement in relation to Dysthyroid Optic Neuropathy. ISRN Ophthalmol. 2014: 435276.
- Darcy SJ, Miller TA, Goldberg RA, Villablanca JP, Demer JL, et al., (2008) Magnetic resonance imaging characterization of orbital changes with age and associated contributions to lower eyelid prominence, Plast.Reconstr Surg. 122(3): 921-929.
- MoraxS, Herdan ML (1990) The aging eyelid. Schweiz Rundsch Med. Prax. 79(48): 1506-1511.
- Shore JW, McCord CD Jr (1984) Anatomic changes in involutional Blepharoptosis. Am.J Ophthalmol. 98(1): 21-27.
- Malhotra R, Mahadevan V, Leatherbarrow B, Barrett AW (2015) The Post-Levator Aponeuros is Fat Pad. Ophthal Plast Reconstr Surg. 31(4): 313-317.
- Schaudig U, Schumacher S (2012) Simple rules for orientation in transcutaneous ptosis surgery: a contribution to the surgical anatomy or: how not to get lost in the upper eyelid. Klin Monbl Augenheilkd. 229(1): 31-34.
- Pessa JE, Desvigne LD, Lambros VS, Nimerick J, Sugunan B, et al., (1999) Changes in ocular globe-to-orbital rim position with age: Implications for aesthetic blepharoplasty of the lower eyelids. Aesthetic Plast Surg. 23(5): 337-342.