Correlation of Visual Outcome with Postoperative Glycemic Control in Patients with Diabetes Following Cataract Surgery
Shruthi K1, Venugopal KC2*, Acharya P3, Spoorti M4, Renuka SK5, Parvathy PS6
1 Postgraduate Student, Department of Ophthalmology, Hassan Institute of Medical Sciences, Hassan, Karnataka, India.
2 Professor, Department of Ophthalmology, Hassan Institute of Medical Sciences, Hassan, Karnataka, India.
3 Assistant Professor, Department of Ophthalmology, Hassan Institute of Medical Sciences, Hassan, Karnataka, India.
4 Postgraduate Student, Department of Ophthalmology, Hassan Institute of Medical Sciences, Hassan, Karnataka, India.
5 Postgraduate Student, Department of Ophthalmology, Hassan Institute of Medical Sciences, Hassan, Karnataka, India.
6 Postgraduate Student, Department of Ophthalmology, Hassan Institute of Medical Sciences, Hassan, Karnataka, India.
*Corresponding Author
Kavitha Chikkanayakanahalli Venugopal MBBS, MS (Ophthal),
Professor, Department of Ophthalmology,
Hassan Institute of Medical Sciences, Hassan, Karnataka, India.
Tel: 9448064116
E-mail: kavithacv_mys@yahoo.com
Received: May 28, 2019; Accepted: December 23, 2019; Published: December 27, 2019
Citation: Shruthi K, Venugopal KC, Acharya P, Spoorti M, Renuka SK, Parvathy PS. Correlation of Visual Outcome with Postoperative Glycemic Control in Patients with Diabetes Following Cataract Surgery. Int J Ophthalmol Eye Res. 2019;7(3):412-417. doi: dx.doi.org/10.19070/2332-290X-1900083
Copyright: Venugopal KC© 2019. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Purpose: To evaluate visual outcome and analyse the correlation of visual acuity and ocular findings with glycemic control following cataract surgery in diabetic patients.
Setting: Department of ophthalmology, Hassan Institute of Medical Sciences, Hassan, Karnataka, India Design: Prospective Observational Study.
Methods: Prospective observational study in 54 diabetic patients with cataract. These patients were followed up for 6 months after cataract surgery with evaluation of visual acuity, ocular findings and were correlated with the postoperative glycemic control.
Results: 1 week after cataract surgery, 13 patients with normal RBS (<140mg/dl) had visual acuity of 6/6-6/12, four patients with RBS more than 141mg/dl had visual acuity of 6/60- 3/60. Anterior chamber reaction was seen in eight patients with RBS >141mg/dl. At the end of six months, 36 patients with normal RBS had visual acuity of 6/6- 6/12. Remaining patients with RBS >141mg/dl had visual acuity less than 6/12
Conclusion: Good glycemic control after cataract surgery is essential for good postoperative visual outcome in diabetic patient.
2.Objectives of the Study
3.Materials and Methods
3.1 Inclusion Criteria
3.2 Exclusion Criteria
3.3 Methodology
4.Results
5.Discussion
6.Conclusion
7.What was Known before this Paper
8.What this Paper Adds
9.References
Introduction
Cataract in diabetic patients is a major cause of blindness in developed and developing countries. Diabetic patients are at a higher risk of developing cataract and at a faster rate. Diabetic patients also have a higher risk of complications after cataract surgery compared to nondiabetics. Although cataract surgery has been demonstrated to improve vision in up to 95% of patients, those with diabetes may be at increased risk of complications and poor visual outcomes [4]. Surgery may cause a rapid acceleration of retinopathy, induce rubeosis or lead to macular changes, such as macular edema or cystoid macular edema. The worst outcomes may occur in operated eyes with active proliferative retinopathy and/or pre-existing macular edema [4].
Patients with pre-existing proliferative diabetic retinopathy are more likely to progress rapidly after cataract surgery. Factors responsible for worsening of retinopathy post surgery could be hyperglycemia, posterior capsular rupture, prolonged duration of surgery and vitreous loss [4].
Cataract is the leading cause of blindness in diabetics. Visual outcome after cataract surgery in diabetic may not be as good as in non-diabetics due to poor glycemic control leading to anterior segment changes like corneal oedema and breech in blood aqeous barrier and worsening diabetic retinopathy. As the blood sugar level is a controllable factor, we wanted to analyse the effect of blood sugar levels post-operatively on the visual outcome.
Hence, we aimed at studying the relation of blood sugar levels with visual outcome of diabetic patients following cataract surgery.
Objectives of the Study
1. To evaluate visual outcome of diabetic patients following cataract surgery.
2. To correlate visual outcome with glycemic control post cataract surgery among diabetic patients.
3. To correlate ocular findings with glycemic control post cataract surgery among diabetic patients.
Materials and Methods
A prospective observational study was conducted in about 108 patients attending out patient Department of Ophthalmology at HIMS Hassan. Prior approval from Institutional Ethical Committee was obtained for conducting the study. The study period was from 1/02/2018 to 31/07/2018. The patients were included in the study by applying the following Inclusion and Exclusion criteria.
1. Patients belonging to either sex irrespective of age who are known case of diabetes mellitus or newly diagnosed to have diabetes mellitus attending outpatient department of ophthalmology who underwent cataract surgery in HIMS teaching hospital, Hassan were included in the study.
Following patients were excluded from the study -
1. Patients with traumatic cataract
2. Patients with uveitis
3. Patients with complicated surgery like posterior capsular rent, iris prolapse, iridodialysis, capsular dialysis
4. Patients with lens induced glaucoma
5. Patients with other co-morbidities like hypertension, chronic obstructive pulmonary disease.
Patients fulfilling the inclusion criteria were recruited into the study.
The aims and objectives of the intended study was properly explained to the subjects and informed consent was taken. Data was collected as per the proforma sheet.
Ophthalmological workup was done as follows. Visual acuity, slit lamp bio microscopy, direct and indirect ophthalmoscopy, retinoscopy, intraocular pressure measurement using applanation tonometry lacrimal sac syringing, keratometry and A-scan and biometric calculation of IOL power were done in all patients.
All patients diagnosed with cataract were subjected for the following laboratory investigations-
1. Random Blood Sugars
2. Fasting Blood Sugars and Post Prandial Blood Sugars
3. HIV
4. HBsAg
5. Complete blood count
6. Glycated hemoglobin (HbA1c).
ECG was also done for these patients. Physician fitness was obtained.
All patients who were known cases of diabetes and the newly diagnosed diabetic patients with cataract with a RBS of ≤ 160mg/ dl on the day of surgery were considered for the surgery. They underwent manual Small incision cataract surgery with posterior chamber intraocular lens implantation under peribulbar block. Postoperatively these patients were given the following medications- Tab Ciprofloxacin 500mg for 5 days, Tab Ranitidine 150mg for 5 days, Tab Diclofenac 50mg for 5 days, Moxifloxacin with Dexamethasone eye/drops 10 hourly for 1 week and was tapered over a period of 6 weeks, Nepafenac e/d % 10 TID.
These patients were then followed up at post-op day 1, 1 week after cataract surgery with visual acuity, anterior segment evaluation, dilated fundoscopy and blood sugar estimation. Later patients were followed up at 3 weeks and 6 weeks after surgery. Then patients were followed up on a monthly basis till 6 months. At every follow up patients were examined for visual acuity, anterior segment evaluation, dilated fundoscopy and random blood sugar estimation. At the end of 3rd month and 6th month patients glycemic control was assessed with HbA1c levels.
Visual outcome and ocular findings postoperatively correlated with glycemic control and analyzed.
Data was analyzed using descriptive statistics.
Results
Out of 108 patients, 64 (59.3%) were males and 44 (40.7%) were females (Figure 1). Mean age was 61.80 with range between 23 to 82 years. Among them, 60 (55.6%) patients had diabetes for a duration less than 5 years, 30 (27.8%) had 5-10years of diabetes , and 18 (16.7%) patients had diabetes for a period more than 10 years.
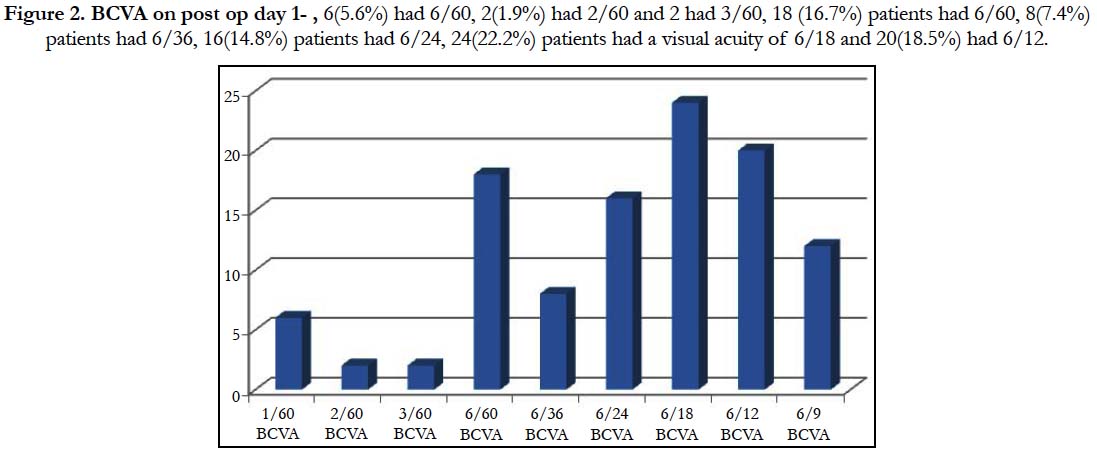
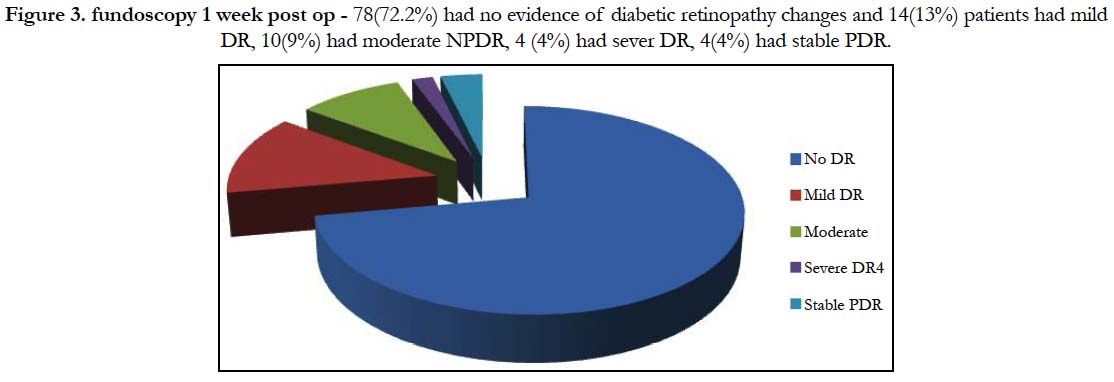
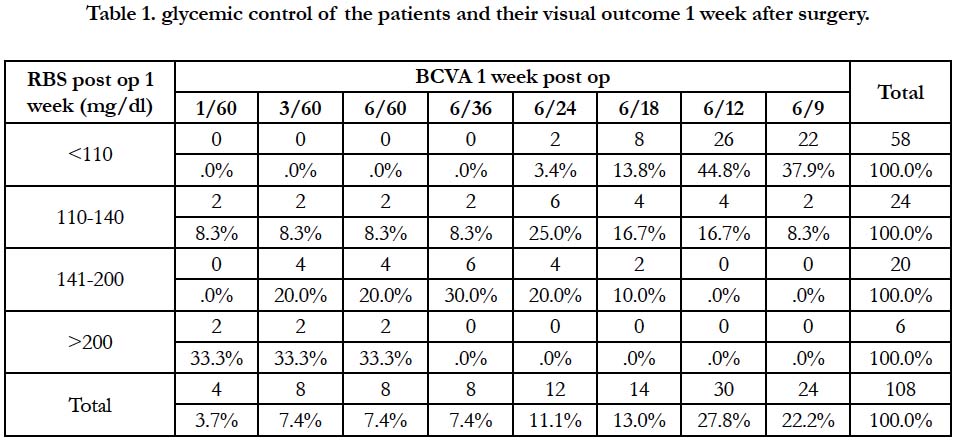
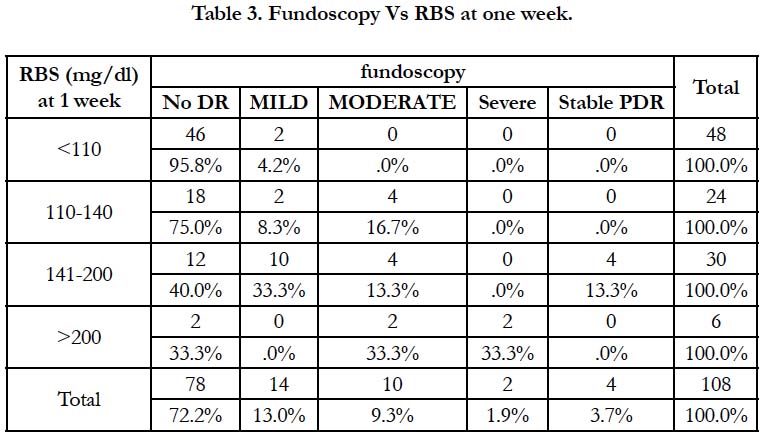
1 week following cataract surgery, 16 (14.8%) patients had 6/24, 24 (22.2%) patients had a visual acuity of 6/18 and 20 (18.5%) had 6/12 (Figure 2). 32 (29.6%) had AC reaction and 76 (70.4%) did not have any AC reaction at their first follow up. 78 (72.2%) of them had no evidence of diabetic retinopathy changes and 14 (13%) patients had mild DR, diabetic retinopathy changes (Figure 3). 48 (44.4%) of them had blood sugar less than 110mg/dl, 24 (22.2%) had RBS in the range of 110-140mg/dl, 30 (27.8%) patients had RBS between 141-200mg/dl (Table 1). 68(63%) of the patients had a HbA1c less than 6.5, 26(24.1%) had HbA1c between 6.5 to 8, and only 14 patients (13%) had HbA1C more than 8.
Figure 2. BCVA on post op day 1- , 6(5.6%) had 6/60, 2(1.9%) had 2/60 and 2 had 3/60, 18 (16.7%) patients had 6/60, 8(7.4%) patients had 6/36, 16(14.8%) patients had 6/24, 24(22.2%) patients had a visual acuity of 6/18 and 20(18.5%) had 6/12.
Figure 3. fundoscopy 1 week post op - 78(72.2%) had no evidence of diabetic retinopathy changes and 14(13%) patients had mild DR, 10(9%) had moderate NPDR, 4 (4%) had sever DR, 4(4%) had stable PDR.
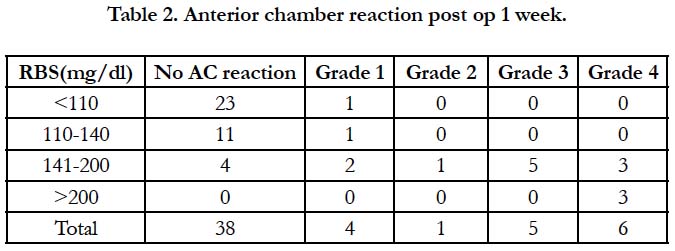
Among 108 patients, 26(44.8%) patients with visual acuity of 6/12 had normal RBS <110mg/dl, four(20%) patients with vision 3/60 and four (20%) patients with vision 6/60 had RBS more than 141mg/dl and this difference was statistically significant (TABLE 1). Anterior chamber reaction was seen in 22 (73.3%) patients with a RBS in the range of 141-200mg/dl and 6(100%) of patients with RBS more than 200mg/dl which is found to be statistically significant (Table 2). 46 (95.8%) patients with a normal fundus had RBS less than 110mg/dl and two patients (33.3%) with moderate diabetic retinopathy had RBS more than 200mg/ dl, four patients( 13.3%) with stable Proliferative diabetic retinopathy had RBS between 141-200mg/dl (Table 3). This difference was found to be statistically significant.
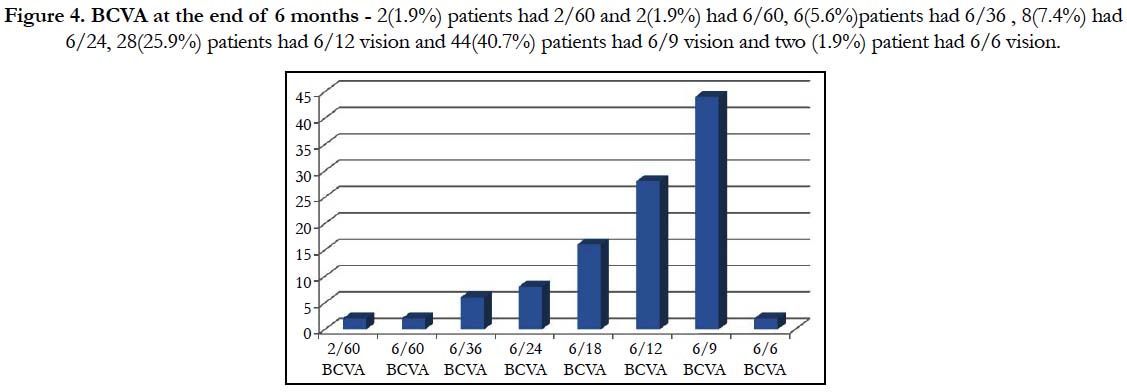
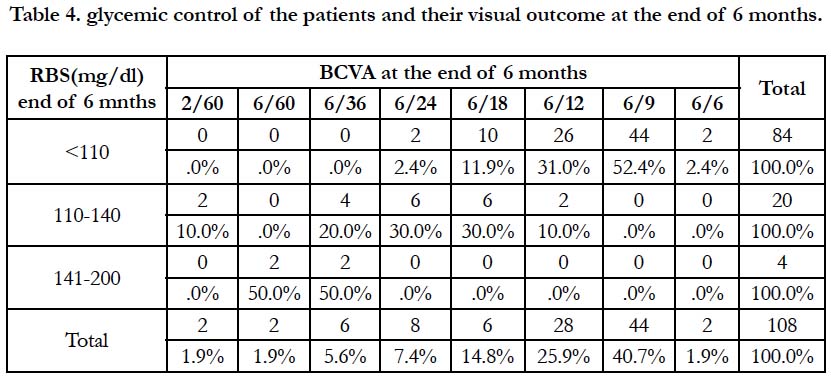
At the end of six months, 28(25.9%) patients had 6/12 vision and 44(40.7%) patients had 6/9 vision and two (1.9%) patient had 6/6 vision (Figure 4). 104 (96.3%) patients had random blood sugar of less than 140mg/dl. Only four (3.7%) patients had random blood sugar more than 140mg/dl. At the end of six months, 84 patients had HbA1C less than 6.5, 24(22.3%) patients had HbA1c more than 6.5.
Figure 4. BCVA at the end of 6 months - 2(1.9%) patients had 2/60 and 2(1.9%) had 6/60, 6(5.6%)patients had 6/36 , 8(7.4%) had 6/24, 28(25.9%) patients had 6/12 vision and 44(40.7%) patients had 6/9 vision and two (1.9%) patient had 6/6 vision.
Among 108 patients, 44 (52.4%) patients with visual acuity of 6/9 and two (2.4%) patient with vision 6/6 had normal RBS <110mg/ dl, two (50.0%) patients with vision 6/36 had RBS between 141- 200mg/dl and this difference was statistically significant (Table 4). None of the patients had any anterior chamber reaction. 74 (88.1%) patients with a normal fundus had RBS less than 110mg/ dl, two (60.0%) patients with moderate diabetic retinopathy had RBS between 141-200mg/dl. This difference was found to be statistically significant.
At the end of three months, glycemic control assessed with HbA1c. 22(50.0%) patients with visual acuity of 6/9 had HbA1c less than 6.5. Six (42.5%) patients with vision 3/60 had HbA1C more than 8.0. This difference was found to be statistically significant. At the end of six months, 44(52.4%) patients with visual acuity of 6/9 and six (27.3%) patients with vision 6/36 had HbA1C between 6.5-8.0 and two (100%)patients with vision 6/60 had HbA1c more than 8.0.
Discussion
Patients with diabetes mellitus (DM) have a higher prevalence of lens opacities [1] and develop cataract at an earlier age than non-diabetics [13]. Cataract in diabetic patients decreases the visual acuity, makes an adequate examination of the retina harder or impossible, and photocoagulation of diabetic retinopathy more difficult. Therefore, it is important to perform cataract surgery for visual rehabilitation and for diagnostic and therapeutic reasons [4].
We found 20 patients (18.5%) with poor glycemic control had a BCVA less than 6/60 and 68 (63%) patients with good glycemic control had BCVA 6/6-6/18 in the first follow up. Also this study showed final visual outcome of 88 (90.7%) patients with good glycemic control was BCVA 6/24-6/6 and 4 (3.8%) patients with poor glycemic control (RBS >200mg/dl) was BCVA <6/60.
Study by Onakpoya OH et al., showed visual improvement seen following surgery for advanced cataract in diabetics [12]. Post operative monitoring for treatment of diabetic retinopathy may enhance visual outcome.
Abdul Rashid Shaikh et al., concluded that visual outcomes in diabetics after phacoemulsification with IOL is almost as good as that in non-diabetic patient if the diabetics have good glycemic control [14].
We found that there is good visual outcome upto 6/12-6/6 in those patient with good glycemic control upto 6months. In those patients without good glycemic control there was poor visual acuity, anterior chamber reaction like corneal edema, iritis. Two patients with very high blood sugar levels developed iritis and vitritis. Two patients had cystoid macular edema who had high sugar levels.
These complications occur due to breakdown of blood aqueous barrier leading to increased albumin in aqueous which results in flare [4]. Later these patients were treated with systemic steroids, topical steroids and antibiotics and analgesics which reduced symptoms and signs. This again warrants to that steroids may rise the blood sugars which needs to be monitored regularly.
Similar to the above studies we concluded that good glycemic control in a diabetic patient is required for a good visual outcome following cataract surgery.
We found that the final visual outcome was improved in the majority of diabetic eyes which was similar to the study conducted by Zaczek et al., [4].
Conclusion
Blood sugar levels in a diabetic patient who underwent cataract surgery should be monitered for atleast upto 6 months. Patients with good glycemic control upto 6 months will have good visual outcome in the long term in diabetics who have undergone cataract surgery.
What was Known before this Papern
• Hyperglycemia following cataract surgery in any diabetic patient would result in breakdown of blood aqueous barrier and result in AC reaction resulting in decreased vision and also would result in progression of retinopathy and macular edema.
What this Paper Adds
• Hyperglycemia following cataract surgery will result in decreased vision. However, regular monitoring and prompt control of sugars will result in improved vision even in diabetic patient following cataract surgery.
References
- Bowling B. Read Management of age related cataract.8th ed. In: Kanski’s Ophthalmology , A systemic approach; 2016. Elsevier ,Saunders Ltd..2016; 273-297.
- Y Brodie SE. Ophthalmology. 4th ed. M. Yanoff, JS Duker, editor. Elsevier. 2014;129:139-140.
- Krepler K, Biowski R, Schrey S, Jandrasits K, Wedrich A. Cataract surgery in patients with diabetic retinopathy: Visual outcome, progression of diabetic retinopathy, and incidence of diabetic macular oedema. Graefe’s Arch Clin Exp Ophthalmol. 2002 Sep; 240(9):735-8. PMID: 12271370.
- Zaczek A, Olivestedt G, Zetterström C. Visual outcome after phacoemulsification and IOL implantation in diabetic patients. Br J Ophthalmol 1999 Sep; 83(9):1036-41. PMID: 10460771.
- Javadi MA, Zarei-Ghanavati S. Cataracts in Diabetic Patients: A Review Article. J Ophthalmic Vis Res. 2008; 3(1): 52-65. PMID: 23479523.
- Bhadania M. A review: Cataract, a common ocular complication in Diabetes. IJPR. 2016;6(06):189.
- Guo X, Gao Y. The relationship between diabetic retinopathy and cataract extraction with intraocular lens implantation in diabetics. Zhonghua Yan Ke Za Zhi. 1995 Nov; 31(6): 440-2. PMID: 8762573.
- Per Flesner, Birgit Sander, Vibeke Henning, Hans-Henrik Parving, Morten Dornonville de la Cour, Henrik Lund-Andersen. Cataract surgery on diabetic patients. A prospective evaluation of risk factors and complications. Acta Ophthalmol. Scand. 2002: 80: 19–24. PMID: 11906299.
- Urban Eriksson, Albert Alm, Gunilla Bjärnhall, Elisabet Granstam, Anna Wikberg Matsson. Macular edema and visual outcome following cataract surgery in patients with diabetic retinopathy and controls. Graefe's Archive for Clinical and Experimental Ophthalmology. 2011 Mar; 249(3): 349-59. PMID: 20827486.
- Y Liu, L Luo, M He, X Liu. Disorders of the blood-aqueous barrier after phacoemulsification in diabetic patients. Eye. 2004 Sep; 18(9): 900-4. PMID: 15017379.
- Tetsuro Oshika, Satoshi Kato, Hideharu Funatsu. Quantitative assessment of aqueous flare intensity in diabetes. Graefe's Arch Clin Exp Ophthalmol. 1989; 227(6): 518-20. PMID: 2625207.
- Onakpoya OH, Bekibele CO, Adegbehingbe SA. Cataract Surgical Outcomes In Diabetic Patients: Case Control Study. Middle East African Journal of Ophthalmology. 2009; 16(2): 88-91. PMID: 20142968. doi:10.4103/0974-9233.53868.
- Nielsen NV, Vinding T. The prevalence of cataract in insulin-dependent and non-insulin-dependent-diabetes mellitus. Acta Ophthalmol Scand. 1984; 62: 595–602. PMID: 6385608.
- Shaikh AR, Mirani AH, Memon MS, Fahim MF. Visual outcome after phacoemulsification with lens implant in diabetic and non-diabetic patients; A comparative study. Pak J Med Sci. 2017; 33(3): 691-694. PMID: 28811796.