Inflammatory Choroidal Neovascularization Secondary to Posterior Scleritis, A Rare Case Report
Deepaka Kumar D1*, NS Muralidhar2, Hemanth Murthy3, Kavitha Rao4
1 Senior Resident, Department of Ophthalmology, S. S. Institute of Medical Sciences & Research Centre, Davangere, India.
2 President and Vitreo-Retina Surgeon, Retina Institute of Karnataka, Bengaluru, India.
3 Medical Director & Vitreo-Retina Surgeon, Retina Institute of Karnataka, Bengaluru, India.
4 Consultant Vitreo-Retina, Retina Institute of Karnataka, Bengaluru, India.
*Corresponding Author
Dr. Deepaka Kumar Dodamani MS, Vitreo-Retinal and Glaucoma Surgeon,
Senior Resident, Department of Ophthalmology, S. S. Institute of Medical Sciences & Research Centre,
Department of Ophthalmology, Davangere, India.
Tel: +91-8762640870/8660619827
E-mail: deepak.dodamani@gmail.com
Received: September 03, 2019; Accepted: December 27, 2019; Published: December 30, 2019
Citation: Deepaka Kumar D, NS Muralidhar, Hemanth Murthy, Kavitha Rao. Inflammatory Choroidal Neovascularization Secondary to Posterior Scleritis, A Rare Case Report. Int J Ophthalmol Eye Res. 2019;7(3):418-420. doi: dx.doi.org/10.19070/2332-290X-1900084
Copyright: Deepaka Kumar D© 2019. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
We report a rare complication of posterior scleritis in a 38 year old female, who presented with pain and blurring of vision. She was treated with systemic steroids over a period of 6 weeks with resolution of scleritis & improved vision. A year later she again presented with sudden drop in vision in the same eye and a fundus picture of active large choroidal neovascular membrane (CNVM) in the peri-papillary region extending to the fovea. This is a rarely reported complication, possibly due to structural changes in the choroid-bruch membrane complex secondary to posterior scleritis.
2.Introduction
3.Case Report
4.Discussion
5.References
Keywords
Posterior Scleritis; Choroidal Neovascularization; Inflammatory.
Introduction
Posterior scleritis is an under-recognized form of scleral inflammation, which can be either infectious or non-infectious in etiology. It has a wide range of presentations and can be confused with intraocular inflammation, ocular tumors & orbital inflammation. Although CNVM post-inflammatory pathology is well described, the same in posterior scleritis is rarely reported in literature.
We herein report a case of CNVM in a patient who recovered from posterior scleritis.
Case Report
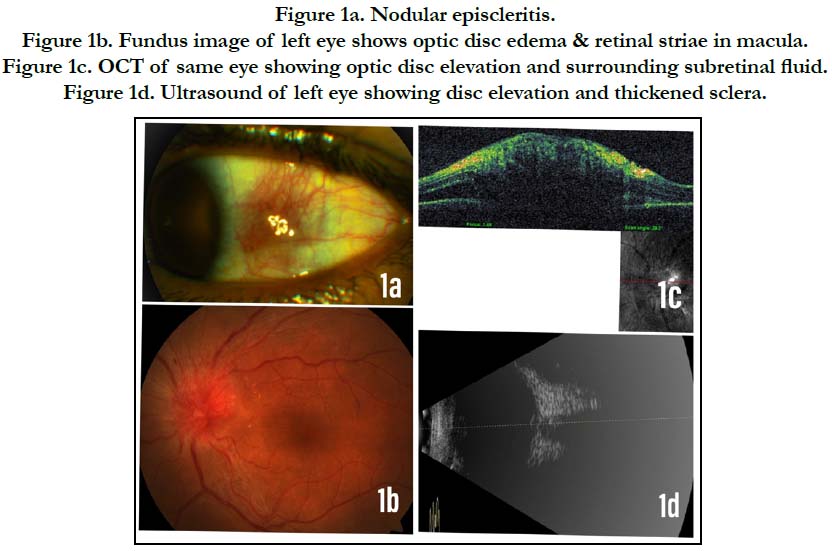
A 38 year old female presented to us with pain and blurring of vision in her left eye since the past 1 month. Her best-corrected visual acuity was 20/20 & 20/80 in right and left eye respectively. Anterior segment was normal in right eye & left eye showed nodular scleritis [Figure 1a]. Fundus examination of left eye showed optic disc edema with retinal striae in macula [Figure 1b], right eye being normal. Optical coherence tomography (OCT) [Figure 1c] & ultrasound (USG) [Figure 1d] confirmed the clinical findings. Blood investigations were normal except raised erythrocyte sedimentation rate(ESR) (70mm/1st hour).
Figure 1a. Nodular episcleritis.
Figure 1b. Fundus image of left eye shows optic disc edema & retinal striae in macula.,br/>
Figure 1c. OCT of same eye showing optic disc elevation and surrounding subretinal fluid.
Figure 1d. Ultrasound of left eye showing disc elevation and thickened sclera.
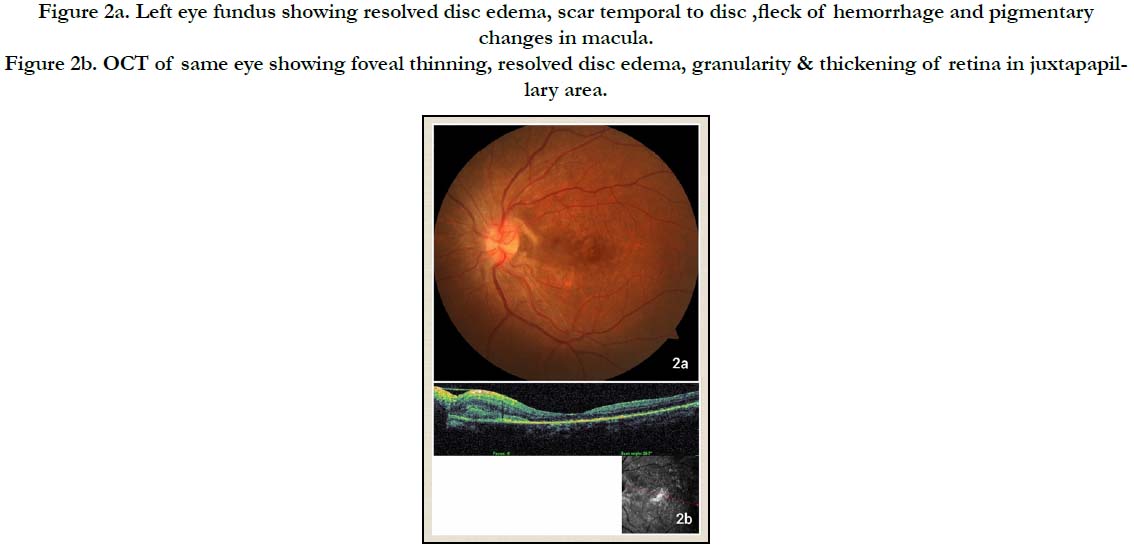
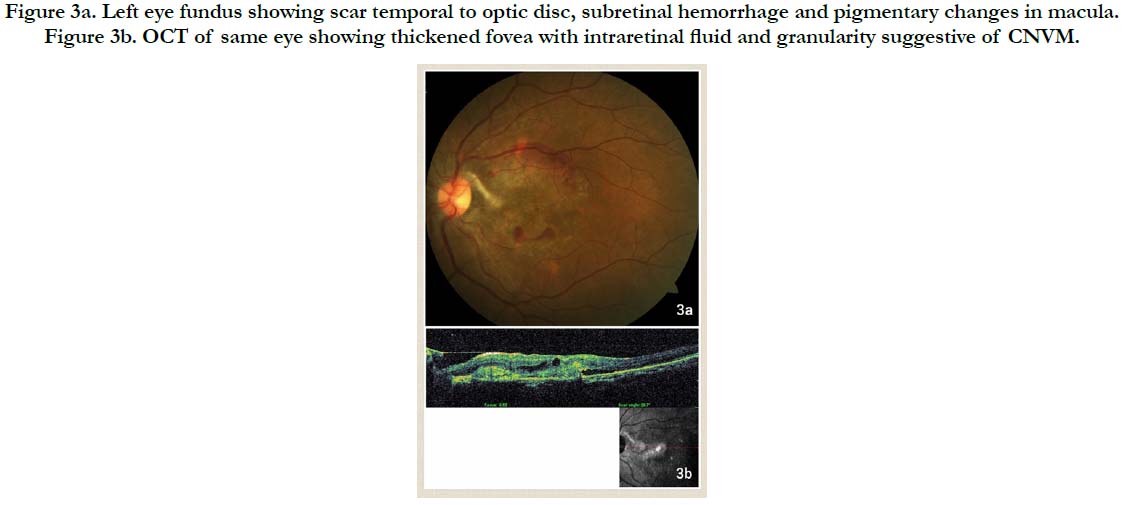
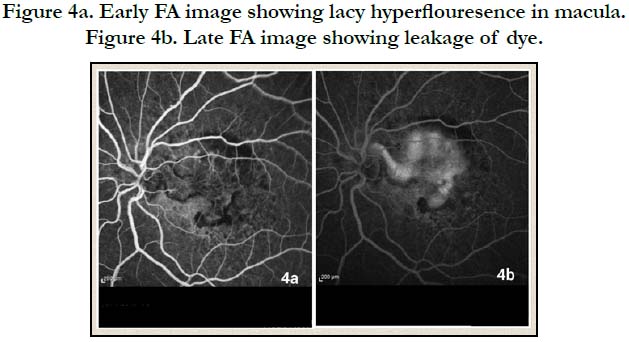
MRI Brain was normal. She was started on oral prednisolone which was tapered over 2 months with progressive improvement in vision to 20/30. Fundus examination at this point of time showed juxtapapillary scar & a fleck of hemorrhage in macula [Figure 2a]. OCT showed foveal thinning & resolved disc edema [Figure 2b]. Than she was lost to follow up, 12 months later she presented with sudden drop in vision (counting finger 1 meter). On examination fundus showed juxtapapillary scar, along with subretinal hemorrhage and pigmentary changes in macula [Figure 3a]. OCT revealed thickened fovea with intraretinal fluid [Figure 3b]. Fluorescein angiography revealed early hyperflourescence with late leakage confirming the diagnosis of choroidal neovascular membrane in macula and peri-papillary area [Figure 4]. Careful retrospective examination of previous OCT images revealed granularity and thickening of retina in juxtapapillary area suggestive of early CNVM which was overlooked as post-inflammatory sequelae [Figure 2b].
Figure 2a. Left eye fundus showing resolved disc edema, scar temporal to disc ,fleck of hemorrhage and pigmentary changes in macula.
Figure 2b. OCT of same eye showing foveal thinning, resolved disc edema, granularity & thickening of retina in juxtapapillary area.
Figure 3a. Left eye fundus showing scar temporal to optic disc, subretinal hemorrhage and pigmentary changes in macula.
Figure 3b. OCT of same eye showing thickened fovea with intraretinal fluid and granularity suggestive of CNVM.
Figure 4a. Early FA image showing lacy hyperflouresence in macula.
Figure 4b. Late FA image showing leakage of dye.
Discussion
CNVM is a rare complication of intraocular inflammation, to the best of our knowledge CNVM secondary to posterior scleritis is even rarer. Gass proposed the most widely accepted theory on formation of CNVM, break in the Bruch's membrane provides an opening in the barrier and subsequent tissue rearrangement through which the new vessels gain admittance into the subretinal space [1], whether similar process occurs in posterior scleritis is unknown.
Histopathology study has revealed fragmentation of scleral collagen, thickened choroid with inflammatory infiltrate, focal loss of RPE [2] which support theory of breakdown of barrier for growth of new vessels. High penetration OCT in acute posterior scleritis has shown thickened choroids confirming histopathological findings [3]. This is further confirmed by indocyanine green angiography studies which have revealed areas of choroidal hyperfluorescence, possibly indicating areas of maximal inflammatory activity [4]. Thus scleral inflammation can lead to choroidal changes which in turn alter the bruch’s membrane - RPE complex and lead to growth of choroidal neovascular membrane.
High index of suspicion is necessary to diagnose inflammatory CNVM. A study by Bansal et al., identified various clinical signs of CNVM that were overlooked which lead to delayed diagnosis in many of there cases [5]. In our case, on retrospective analysis juxtapapillary grey lesion, subretinal hemorrhage and granular thickening on OCT were overlooked.
No clear standard of care currently exists for the treatment of inflammatory CNVM. Studies to evaluate treatment of inflammatory CNVM are limited and mostly retrospective. Laser photocoagulation, local & systemic corticosteroids, anti-VEGF agents and surgery have been tried.
Flaxel et al., concluded that systemic steroids resulted in stabilization of vision (83%), in subfoveal CNVM due to MFC or PIC [6]. Adan and associates described 9 patients with various inflammatory CNVM treated with bevacizumab injections. CNVM resolved in all affected eyes with BCVA improving in 88.8% of eyes over a mean follow-up of 7.1 months and after a mean of 1.3 injections [7]. Unfourtunately our patient declined Anti-VEGF therapy.
Thus importance of early diagnosis of inflammatory CNVM by differentiating its features from underlying primary etiology is very important as highlighted by this case report.
References
- Gass JD. Stereoscopic atlas of macular diseases. Diagnosis and treatment, Mosby Publishers. 1987; 1: 24.
- Calthorpe CM, Watson PG, McCartney ACE. Posterior Scleritis: A clinical and histological survey. Eye. 1988; 2: 267-277. PMID: 3402623.
- Uchihori H, Nakai K, Ikuno Y, Gomi F, Hashida N, Jo Y, et al. Choroidal observations in posterior scleritis using high-penetration optical coherence tomography. International Ophthalmology. 2014 Aug; 34(4): 937-43. PMID: 24398712.
- Auer C, Herbort CP. Indocyanine green angiographic features in posterior scleritis. Am J Ophthalmol. 1998 Sep; 126(3): 471-6. PMID: 9744391.
- Bansal R, Bansal P, Gupta A, Gupta V, Dogra MR, Singh R, et al. Diagnostic challenges in inflammatory choroidal neovascular membranes. Ocular Immunology & Inflammation. 2017; 25(4): 554-562. PMID: 27082010.
- Flaxel CJ, Owens SL, Mulholland B, Schwartz SD, Gregor ZJ. The use of corticosteroids for choroidal neovascularisation in young patients. Eye. 1998; 12(2): 266-72. PMID: 9683952.
- Adan A, Mateo C, Navarro R, Bitrian E, Casaroli-Marano RP. Intravitreal bevacizumab (Avastin) injection as primary treatment of inflammatory choroidal neovascularization. Retina. 2007; 27: 1180-86. PMID: 18046222.